Influence of Hip Muscle Motor Control Training on Pain and Function Post Total Hip Replacement
Citation: Joyal VJ, et al. Influence of Hip Muscle Motor Control Training on Pain and Function Post Total Hip Replacement. Ann Med Health Sci Res. 2017; 7: 96-100
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objectives: To investigate the influence of motor control training of deep external rotators of hip joint on pain and function followed by Total Hip Replacement (THR). Methods: Subjects (n=10) who had posted for unilateral Total Hip Replacements were enrolled. Pre and post intervention data collected from 10 patients, who were posted for total hip replacement. Patient’s received motor control training for deep external rotators of hip joint, twice a day for 8 weeks along with standard THR rehabilitation exercises. Thirty second chair stand test is used as primary outcome measure and NPRS, HOOS and Timed Up and Go test are used as secondary outcome measures. All the outcome measures have taken pre and post 8 weeks of intervention. Paired t-test used for statistical analysis to find out the changes within the group. Results: Overall significant differences were observed before and after the training in all outcomes. 30 sec chair stand test improved by mean of 2.60 ± 1.35 times (p=0.001). NPRS demonstrated a reduction in pain score from 8.90 (0.99) to 2.30 (0.82) with a mean of 5.60 ± 0.96. Timed Up and Go test showed an improvement of 8.10 sec over an 8 weeks from 29.60 sec to 21.50 sec (p=0.003). HOOS total score showed a better shift from 98.89 ± 16.59 to 52 ± 8.92 in 8 weeks. Conclusion: The implementation of motor control training of deep external rotators of hip joint along with standard THR protocol following unilateral Total Hip Replacement improves pain scores and physical function post 8 weeks of surgery.
Keywords
Motor control training; Total hip replacement; THR rehabilitation; Motor control dysfunction; Hip Stabilizers
Introduction
Total Hip Replacement (THR) is a surgical procedure performed for osteoarthritis, avascular necrosis and any infectious conditions affecting hip joint. [1,2] It involves surgical excision of neck of femur and acetabular cartilage which is replaced with prosthetic components. [3] Pain, decreased range of motion, impaired postural stability and mobility are followed with the surgery. [4,5] A systematic review on post THR rehabilitation describes the post THR rehabilitation exercises consisting of ankle toe movements, quadriceps and gluteal sets, hip range of motion exercises, early mobilization and after 8 weeks, the rehabilitation includes weight bearing exercises and hip abductor muscle resistance training. [1]
An interview based study conducted on postoperative THR standard rehabilitation found that exercises prescribed by physiotherapists include quadriceps and hip abductor strengthening, bridging, range of motion exercises and weight bearing exercises. [6] A randomized controlled trial by Jan et al. [7] on home exercise post THR describes the exercise which consists of isotonic strengthening exercises for hip flexors, abductors and extensors with low resistance and 30 minutes walking every day. [7] However analysis of gait, squat manuever and limb loading of post THR patients suggest that dynamic instability persists in this group of individuals even after standard rehabilitation. [8]
For a functionally pain free stable joint, active control of hip muscles are essential. The hip joint stability is contributed by active, passive and neural subsystem. The deep muscles of hip joint contribute to it majorly by closely acting to its axis and gives compression force. The main deep muscles of hip joint includes gamelli superior and inferior, obturators internus and externus, and quadratus femoris, which also functions as the hip external rotators. [9] Studies on cadaveric specimen found that posterior capsule of hip joint is reinforced with obturator externus contributing to hip joint stability. [10] Dysfunction associated with these muscles makes the joint less stable and painful and rehabilitation specifically targeting these muscles improve function and alleviate pain. [9]
Contraction of the local musculature is considered a feed forward strategy of the nervous system. It prepares the joint for pertubations caused by the limb movement. [9] Research shows that pain alters this feed forward strategy and causes rapid atrophy of local muscles. [11] Deep location and proximity of these muscles to sciatic nerves makes difficult to get an accurate electromyogrphic data of their dysfunction.9 Evidence of hyperactivation of global muscles after THR suggests a compensatory mechanism for the local muscle dysfunction. [12]
Motor control is defined as the ability to regulate or direct the mechanisms essential for the movement. [13] Motor control training involves 3 stages: stage of conscious/cognitive, stage of associative/repetition and stage of automatic. The cognitive stage required high levels of awareness from the subjects. It is augmented with visual, verbal and tactile cuing from the therapist, normal breathing pattern and a good understanding about the movements by the subject. This stage retains the activation of local muscle system during the movement. The stage of association primarily involves identification and correction of faulty movements. This stage helps therapist to identify the movement faults and break them into small parts. This followed by repetition of movements in the corrected manner. The final step is incorporating the corrected movements into the functional tasks of daily living. [14]
Sims et al. [15] reported higher gluteus medius EMG firing in subjects with unilateral hip osteoarthritis. A study by Agostini et al. [12] observed altered muscle activation and timing patterns in gluteus medius even after THR. Retcheford et al. [9] proposed that local muscle dysfunction is present in the joint associated with pain and pathology. A specific muscle retraining can restore the muscle function in those joints. The hip joint stability can be enhanced by retraining the deep external rotators of hip. The local muscle activation facilitates the effectivness of the other standard rehabilitation exercises. Thus evidence supports activation of these muscles before global muscle training. [9]
Standard THR protocols are having no components to rehabilitate motor control dysfunction of deep external rotators of hip. There is a paucity of literature for motor control exercise of deep external rotators of hip. Hence this study aimed to investigate the influence of motor control training of deep external rotators on pain and functional performance in subjects who have undergone unilateral THR.
Materials and Methods
A total of 13 subjects who were referred for THR were screened for inclusion and 10 subjects were recruited for the study. The inclusion criteria was unilateral THR and age between 40 to 85 years. [3] subjects were excluded from the study due to bilateral and revision THR, hemiarthroplasty, THR following hip fractures and neurological conditions which affects patients ability to understand and follow commands such as stroke, parkinsons disease. Sample size calculated as 10, based on 30 sec chair stand test with power of study as 80% anticipating MCID of 3 stands with standard deviation of 2.6. The primary outcome measure used was 30 sec chair stand test (30 sec CST). The secondary outcome measures includes Numerical Pain Rating Scale (NPRS), Hip disability and Osteoarthritis Outcome Score (HOOS) and Timed Up and Go test (TUG). The study was approved by the Institutional Research Committee of School of Allied Health Sciences, Manipal Univeristy, India and conducted at Manipal Hospital, Bangalore. The subjects were screened and those who met the inclusion criteria were recruited. The purpose of the study was explained and informed consent was obtained. The recruited subjects were assessed at baseline pre-operatively with both primary and secondary outcome measures. Posterolateral approach is the common approach used, which preserves the abductor mechanism of hip. To access the hip joint the gluteus maximus is split in line with the muscle fibers and the deep external rotators are transected near its insertion. It preserves the integrity of the gluteus medius and vastus lateralis. In order to dislocate the hip joint the posterior capsule is incised thus leading to a higher incidence rate of joint instability and dislocation of hip postoperatively. [16]
Postoperatively subjects received an intervention which involved standard THR protocol along with motor control training for deep external rotators of hip joint. Intervention took place daily till the subject got discharged and after that twice a week for 8 weeks, with each session lasting for 20-30 minutes. The therapist supervised the subjects through telephone once a week for 8 weeks to maintain the continuity of intervention. The subjects underwent another set of assessment of the same outcomes after 8 weeks.
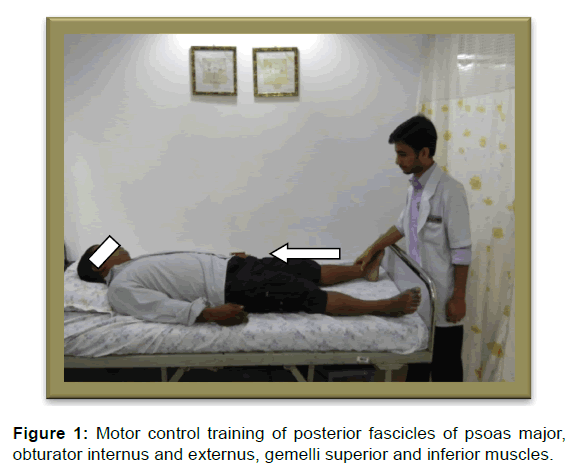
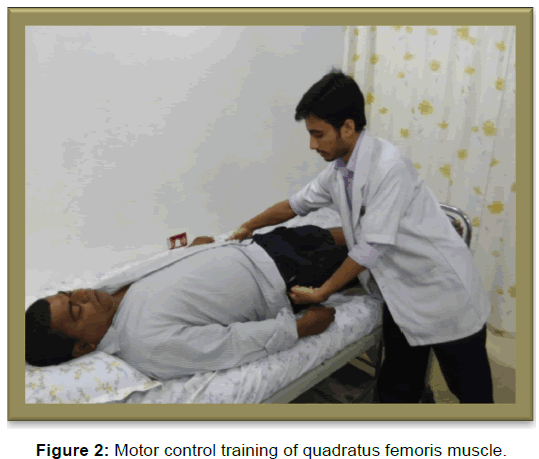
The intervention began within 24 hours after surgery and took place twice a day till discharge. Most of the patient received pain medication and cryotherapy for pain management postsurgery. On an average most of the patients got discharged from hospital after 8 days. Subjects were asked to perform two sets of 10 repetition lasting 10 sec. There was a 30 sec break between sets. To target the posterior fascicles of psoas major, obturator internus and externus, gemelli superior and inferior muscles, the subject was asked to lie in supine and to mentally visualize and approximate the head of femur into the acetabulum without tilting the pelvis. For a better understanding of the exercise, patients were practiced it first in normal leg and after familiarisation they were performed it on the operated leg. [17] [Figure 1]. For the quadratus femoris muscle subject was in supine lying and asked to mentally visualize two points on either side of hip (lateral to the hip joint) at the level of the greater trochanter and approximate them with minimum contraction of the buttocks (gluteus maximus). [17] [Figure 2].
The statistical analysis was done using SPSS software (version 16.0; SPSS. Chicago, IL, USA). Paired ‘t’ test was used to assess the difference within the group with confidence interval set as 95% and p value of <0.005
Results and Discussion
A total of 10 subjects (7 males and 3 females) who had undergone unilateral THR with mean age 60.60 ± 14.93 years were included in our study. Seven subjects underwent THR as a result of OA and the remaining was having AVN of head of femur. The demographic and baseline data of the subjects is given in Table 1. 30 s chair stand test in the present study changed from 6.80 to 9.30 with a mean of 2.60 ± 1.35 times, which was statistically significant (p< 0.001). NPRS demonstrated a reduction in pain score from 8.90 (0.99) to 2.30 (0.82) by a mean of 5.60 ± 0.96 points.
| Baseline characteristics | Baseline measurements mean (SD) |
|---|---|
| Age (years) | 60.60 (14.93) |
| Gender (males and females) | 8 Male, 3 Female |
| Indication for surgery (OA and AVN) | OA=8, AVN=3 |
| 30s CST | 6.80 (3.40) |
| NPRS | 8.90 (0.99) |
| HOOS total score | 98.89 (16.59) |
| HOOS Symptoms | 9.80 (2.44) |
| HOOS Pain | 26.30 (5.38) |
| HOOS ADL | 41.90 (8.58) |
| TUG | 29.60 (9.94) |
Table 1: Demographic and baseline characteristics of subjects.
Timed Up and Go test reported an improvement of 8.10 sec over an 8 weeks from 29.60 sec to 21.50 sec (p< 0.003). Post 8 weeks sub-scales of HOOS such as pain, symptoms and functional disability demonstrated improvement. The total disability score of HOOS reached to 52 ± 8.92 from 98.89 ± 16.59 in 8 weeks (p< 0.001). The pain sub-scale changed from a mean of 26.30 ± 5.38 to 13.10 ± 2.69 points, symptom sub-scale shifted from a mean of 9.80 ± 2.44 to 4.90 ± 1.59 and functional disability decremented to 23.10 ± 3.60 from 41.90 ± 8.58 [Table 2].
| Outcomes | Pre mean (SD) | Post mean SD | Mean difference | 95% CI Upper, lower limit | P-value |
|---|---|---|---|---|---|
| 30 s CST | 6.80 (3.40) | 9.30 (3.23) | 2.60 | 3.58, 1.63 | 0.000 |
| NPRS | 8.90 (0.99) | 2.30 (.82) | 5.60 | 6.29, 4.91 | 0.000 |
| HOOS symptoms | 9.80 (2.44) | 4.90 (1.59) | 4.90 | 6.09,3.81 | 0.000 |
| HOOS pain | 26.30 (5.386) | 13.10 (2.685) | 13.20 | 16.16, 10.25 | 0.000 |
| HOOS ADL | 41.90 (8.569) | 23.10 (3.60) | 18.80 | 24.29, 13.31 | 0.000 |
| TUG | 29.60 (9.94) | 21.50 (5.29) | 8.10 | 12.68, 3.53 | 0.003 |
Table 2: Within group analysis of all outcome measure after 8 weeks of intervention.
Discussion
The present study aims to find the influence of hip muscle motor control training on pain and function following unilateral total hip replacement. 8 weeks motor control training improved the outcome measures in our study.
The primary outcome measure 30 sec chair stand test changed from a baseline measure of 8 to 9 stands with a mean difference of 2 stands. The observed change was clinically significant since the MCID of 30 s CST is 2-3 stands.[18] A study done by Mikkelsen et al. [19] to evaluate the effect of early progressive resistance training in subjects who had undergone unilateral THR found a mean change of 2 stands in 30 s CST in the intervention group. The progressive resistance training group had received 2 days of supervised resistance training and 5 days of unsupervised home exercises from the first week of surgery for 10 weeks. The observed improvements in Mikkelsen et al. [19] study may be due to increased hip muscle strength whereas, in our study motor control training of hip muscles demonstrated the same result in a comparatively shorter duration. This may indicate higher muscle recruitment of hip stabilizers and thus shortened the duration for recovery [20]
The NPRS score for pain intensity in the present study reduced post 8 weeks of intervention by a mean difference of 6 point from the baseline score of 8.90. The MCID for NPRS was reported as 3 points; and current study demonstrated a change of 6 points which was a clinically significant.[20] A multicenter randomized controlled trial by French et al. [21] to test the effect of manual therapy with exercises on hip OA observed a mean change of 1.82 points after 9 weeks of intervention. These 5 days sessions in each week consists of 30 min of stretching, strengthening, generalized body exercises and 15 min of manual therapy sessions. It shifted the NPRS score from 6.02 to 4.20 after 9 weeks of intervention. The manual therapy interventions (low grade hip joint mobilization) may have caused micro-trauma of soft tissues and prevented the pain score to change significantly. The comparatively major improvement in pain score in the present study may be due to motor control training of hip muscles. It may have prevented the uncontrolled movement between the articular surfaces of the hip joints during daily activities. In addition to that the muscular dysfunction present between local and global muscle systems of hip after THR may be reduced by the motor control training. Collectively it helps to prevent micro-trauma; thus leading to a major shift in pain score.
Timed up and go test of the present study improved from 29.60 sec to 21.50 sec with a mean difference of 8.10 sec. A randomized controlled trial on a center based postoperative rehabilitation in subjects who had undergone unilateral THR demonstrated an improvement in TUG after 8weeks of intervention. The time duration reduced from a baseline measure of 13.5 sec to 11.1 sec with a mean difference of 2.4 sec. [22] The center based group had received exercise focused on functional tasks, daily living tasks, balance, strength and endurance which was delivered 5 sessions in a week. The variety of exercises to the center based group may have resulted in better strength and balance. At the same time comparatively larger difference in TUG in the present study may be due to the higher baseline of 29.60 sec compared to 13.5 sec of the center based group. This change may indicate increased muscle size and higher muscle activation of hip external rotators during TUG. A study by Mendis et al. [23] to test the effect of motor control in subjects with and without low back pain found that 8 weeks of motor control training increased the hip muscle size and prevented hip muscle atrophy.
The HOOS pain sub-scale had improved from a baseline of 34.25% to 68.25% with a mean difference of 33%. The symptom sub-scale had demonstrated a change of 24.5% from 51% to 85.5%. The present study observed a 28.64% change in ADL/functional disability sub-scale. Since the MCID is not established for HOOS, it is difficult to comment on the significance of the observed change. However this improvement may have resulted from the replacement of damaged hip with a new artificial joint. It is augmented by motor control trainingwhich could have improved the balance between local and global muscle system, preventing micro-trauma resulting from an imbalanced muscle system in the hip. This explains the lower pain level and optimized function.
Limitations of the Study
Since the present study had a small sample size the findings of the study cannot be generalized.
Recommendations for Future Research
A Randomized controlled trial is recommended to evaluate the role of motor control training alone in postoperative rehabilitation following THR. The present study did not use EMG analysis or ultrasonography of hip muscles to evaluate the changes in the muscle structure and function. The use of either can give a strong evidence to support the muscle recruitment as well as muscle size changes.
Conclusion
The implementation of a 8 week motor control training for deep external rotators of the hip with the standard THR rehabilitation improves pain and functional outcomes post unilateral THR.
Conflict of Interest
There are no conflicts of interest to report.
REFERENCES
- Monaco MD, Vallero F, Tappero R, Cavanna A. Rehabilitation after total hip arthroplasty: A systematic review of controlled trials on physical exercise programs. Eur J Phys Rehabil Med. 2009; 45: 303-317.
- Coulter CL, Scarvell JM, Neeman TM, Smith PN. Physiotherapist-directed rehabilitation exercises in the outpatient or home setting improve strength, gait speed and cadence after elective total hip replacement: a systematic review. J Physiother. 2013; 59: 219-226.
- Siopack JS, Jergesen HE. Total hip arthroplasty. West J Med. 1995; 162: 243-249.
- Kisner C, Colby LA. Therapeutic exercise foundations and technique. 5th edition. F.A. Davis Company. 2007. Chapter 20. The hip; p: 652-663.
- Jinks C, Lewis M, Croft P. Health status after hip or knee arthroplasty. Ann Rheum Dis .2003; 62: 700-701.
- Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005; 6: 1.
- Jan MH, Hung JY, Lin JCH, Wang SF, Liu TK, Tang PF. Effects of a home program on strength, walking speed, and function after total hip replacement. Arch Phys Med Rehabil. 2004; 85: 1943-1951.
- Brauner T, Wearing S, Ramisch E, Sportwiss D, Zillober M, Horstmann T. Can measures of limb loading and dynamic stability during the squat maneuver provide an index of early functional recovery after unilateral THA?. Arch Phys Med Rehabil. 2014; 95: 1946-1943.
- Retchford T, Crossley K, Grimaldi A, Kemp J, Cowan S. Can local muscles augment stability in the hip? A narrative literature review. J Musculoskelet Neuronal Interact. 2013; 13: 1-12.
- Gudena R, Alzahrani A, Railton P, Powell J, Ganz R. The anatomy and function of the obturator externus. Hip Int. 2015; 25: 424-427.
- Hodges PW, Moseley GL, Gabrielsson A, Gandevia SC. Experimental muscle pain changes feed forward postural responses of the trunk muscles. Exp Brain Res. 2003; 151: 262-271.
- Agostini V, Ganio D, Facchin K, Cane L, Moreira Carneiro S, Knaflitz M. Gait parameters and muscle activation patterns at 3,6 and 12 months after total hip arthroplasty. J Arthroplasty.2014; 29: 1265-1272.
- Cook AS, Woollacott M, Motor control translating research into clinical practice.3rd edition. Philadelphia: Lippincott Williams and Wilkins; 2007. Chapter 1, Motor control issues and theories p: 4.
- Camerford M, Mottram S. Kinetic control the management of uncontrolled movement. Australia. Churchilliving stoneelsevier; 2012. Chapter 4, Retraining strategies for uncontrolled movement. p: 63-78.
- Sims KJ, Richardson CA, Brauer SG. Investigation of hip abductor activation in subjects with clinical unilateral hip osteoarthritis. Ann Rheum Dis. 2002; 61: 687-692.
- Kelmanovich D, Parks ML, Sinha R, Macaculay W. Surgical approaches to total hip arthroplasty. J South Orthop Assoc.2003: 90-94.
- Myers T. Extensor coxaebrevis: Treatment strategies for the deep lateral rotators in pelvic tilt. J Body Mov Ther. 2010; 14: 262-271.
- Dobson F, Hinman RS, Roos EM, Abbott JH, Stratford P, Davis AM et al. OARSI recommended performance based tests to asses physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthr Cartil. 2013; 21: 1042-1052.
- Mikkelsen LR, Mechlenburg I, Søballe K. Effect of early supervised progressive resistance training compared to unsupervised home-based exercise after fast-track total hip replacement applied to patients with preoperative functional limitations. A single blinded randomized controlled trial. Osteoarthr Cartil. 2014; 22: 2051-2058.
- Sloman R, Wruble AW, Rosen G, Rom M. Determination of clinically meaningful levels of pain reduction in patients experiencing acute postoperative pain. Pain Manag Nurs. 2006; 7: 153-158.
- French HP, Cusack T, Brennan A, et al. Exercise and manual physiotherapy arthritis research trial (EMPART) for osteoarthritis of the hip: A multicenter randomized controlled trial. Arch Phys Med Rehabil. 2013; 94: 302-314.
- Galea MP, Levinger P, Lythgo N. A targeted home and center based exercise program for people after total hip replacement: A randomized clinical trial. Arch Phys Med Rehabil. 2008; 89: 1442-1447.
- Mendis MD, Hides JA. Effect of motor control training on hip muscles in elite football players with and without low back pain. J Sci Med Sport. 2016; 1440-2440.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.