Interlink of Oral-Maxillofacial Pathology and Oral-Maxillofacial Prosthodontics
2 Department of Prosthodontics, University of science and technology in Fujairah, Fujairah, United Arab Emirates
3 Department of Oral & Maxillofacial Pathology, Kalinga Institute of Dental Sciences, Kalinga Institute of Industrial Technology (KIIT) Deemed to be University, Bhubaneswar, Odisha, India
Received: 09-Jan-2024, Manuscript No. amhsr-24-132725; Editor assigned: 11-Jan-2024, Pre QC No. amhsr-24-132725 (PQ); Reviewed: 26-Jan-2024 QC No. amhsr-24-132725; Revised: 02-Feb-2024, Manuscript No. amhsr-24-132725 (R); Published: 09-Feb-2024
Citation: Shunmugavelu K, et al. Interlink of Oral-Maxillofacial Pathology and Oral-Maxillofacial Prosthodontics. Ann Med Health Sci Res. 2024;14:930-933
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Restricted mouth opening is evidently seen in Oral Potentially Malignant Disorder (OPMD) which is a chronic condition whereas in prosthodontics, for any treatments, mouth opening is of excellent dimension is required which is in contrary to the patients with OPMD. The current systematic review focuses on interlink of oral and maxillofacial pathology especially OPMD and prosthodontics.
Methods: A detailed literature search was done pertaining to OPMD patients and their association with prosthodontics. Inclusion criteria include various studies done on the above based topics whereas exclusion criteria include individual case reports.
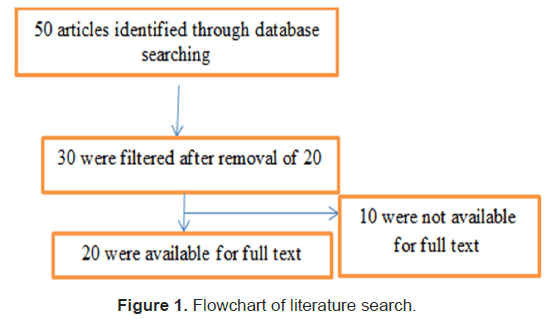
Results: Grand total of 600 cases were identified from 50 papers published in English language literature. Of these 50, 30 were filtered narrowing down to 20 fully downloaded studies pertaining to the topic.
Conclusion: Prosthodontics approach should be done in an exceptional way in patients with OPMD in order to achieve long-term success.
Keywords
OPMD; Prosthodontics; Prosthesis; Oral lesions.
Introduction
Oral cancer is one of the dangerous threats to developing and developed countries. Among the oral cancer, squamous cell sarcoma is the most important. Early detection of the precancerous and oral cancer lesions can result in improved treatment outcome and prognosis. Majority of the countries which involve OPMD are India, Srilanka, Indonesia, Pakistan and Bangladesh [1-5]. Etiology targets to tobacco smoking, human papillomavirus infection, alcohol consumption, and ultra violet radiation from sunlight. There is increased risk of malignancy in case of OPMD which might appear clinically as oral mucosal lesions. The list of OPMD includes erythroplakia, epidermolysis bullosa, leukoplakia, lupus erythematous, palatal lesions in reverse smokers, dyskeratosis congenita, oral lichen planus and oral submucosal fibrosis. Assessment depends on the risk factors which might include duration of habit, type, age, gender, clinical appearance, family history, anatomical location of the lesion and focal infection. Recent advances include microbiome alteration, hemogenic deficiency, systemic sclerosis, micro nutrition deficiency, Zinsser-Engman-Cole syndrome, xeroderma pigmantosum and fanconi anaemia [6-10]. Probable pathogenesis includes mutations in mitochondria, oncogenes dysregulation, epigenetic changes, tumour suppressors like P53, MCM complex protein dysregulation and cytogenetic changes. Therapeutic strategies include electro surgery, photo dynamic therapy which is a non-invasive method which uses a photosensitizer and oxygen which may activate the reactive oxygen species which might lead to microbial death either by necrosis or apoptosis. Alterative treat modalities are cryosurgery, CO2 laser, surgical excision, topical systemic drugs which may include corticoids, vitamin A, lycopene, retinoids and antibiotics [11-15].
Materials and Methods
A comprehensive research was done. Articles from 2013 to till date are considered. The literature databases included were pubmed, web of science, google scholar, SCOPUS, medline followed by cross references. Keywords included were OPMD, oral, dental, prosthodontics, lesions. Multi journals involving oral and maxillofacial surgery, oral and maxillofacial pathology, oral and maxillofacial prosthodontics and oral and maxillofacial medicines were included. Original literatures in English language which are fully available were included. Individual case reports were removed. The important points include publication date, author name, journal name, date of issue, treatment and number of cases (Figure 1) [16-20].
Literature search
The vast literature search was ended up in 20 published articles which are fully downloaded in English from various databases. The universal language of science is English. In order to avoid biasing and erroneous decisions, other languages were excluded. 20 duplicate articles were removed. 10 articles which were not able to fully download were removed. Key areas included oral and maxillofacial pathology, oral and maxillofacial surgery, oral and maxillofacial prosthodontics, oral and maxillofacial medicine, etc.
The term OPMD refers to Oral potentially malignant disorder. Risk factors include alcohol and tobacco which might result in alteration of oral mucosal keratinocytes which in turn involves different genes such as NOTCH1, EGFR, TP53, STAT3 and CDKN2a. This in case leads to increased oral mucosa permeability resulting in alteration of the tumour and immune microenvironment thereby resulting in ultimate invasion and cell adhesion loss. Human papillomavirus oncogenic types are seen to be more prevalent in OPMD in comparison to normal healthy oral mucosa. The pathways of damage in areca nut chewing include chronic inflammation, direct damage to DNA, tumour suppressor, inhibition, DNA repair repression resulting in stem cell conversion which might result in damage of epithelial cells of oral mucosa. Oral microbiome alteration includes elevated levels of Streptococcus, Fusobacterium and Actinomyces. This microbiome alteration triggers cell proliferation and genetic mutations in permanent basis with the help of the products and the metabolites and also produce pro-inflammatory cytokines, inhibits anti-tumour immune cells resulting in malignant transformation and cellular invasion. Genetic syndromes which are included in association with OPMD are conditions in which DNA metabolism is dysregulated such as Dyskeratosis congenita otherwise called Zinsser-Engman-Cole syndrome, Bloom syndrome otherwise called congenital telangiectatic erythema, Fanconi anaemia and Xeroderma pigmentosum. The list of investigation includes visual examination, cytology, salivary biomarkers, tissue staining, auto-fluorescence, spectroscopy and chemiluminiscence. OPMD comprises of oral leukoplakia, oral epithelial dysplasia, oral erythroplakia, erythroplakia, oral submucous fibrosis and oral lichen planus. Pathalomodic entities mentioned are as follows-in case of lichen planus, histopathologically, orthokeratosis, parakerotosis, thickened spinous layer, band-like lymphocytic infiltration seen at the superficial submucosa and the basal level and degeneration of basal cell line of epithelial oral mucosa. In oral submucous fibrosis, atrophy in salivary glands, fibrosis, diffuse chronic inflammatory infiltrate, band-like infiltrate, skeletal muscle atrophy, congestion, edema and vesicle formation are noted. Dysplasia of low grade or high grade or in situ carcinoma includes histopathalogically, dyskeratosis, keratin pearls, basal cell anaplasia and hyperplasia. Infiltrating squamous cell carcinoma comprises of histopathologically invasion of stromal epithelial interface. Sites of involvement in oral leukoplakia are any oral mucosal site. Tongue, alveolar ridges, buccal mucosa and gingiva are mostly involved in proliferative verrucous leukoplakia. Oral Erythroplakia involves floor of the mouth, ventral tongue, palate, and buccal mucosa. Buccal mucosa, tongue and gingiva are involved in oral lichen planus. Any oral mucosal areas are involved in oral submucous fibrosis.
Results and Discussion
Oral leukoplakia
It is defined as a white plaque of questionable risk which excluded known disorders or diseases which might carry no increased risk for cancer. Risk factors include tobacco, alcohol, areca nut chewing and HPV. Two sub divisions are mentionedhomogenous and non-homogenous. Homogenous lesions are superficial flat whereas non-homogenous lesions are verrucous, exophytic and more irregular. Non-homogenous lesions may have higher risk for malignancy. Useful investigation tool is biopsy. Treatment includes bleomycin, retinoids, surgical excision, photodynamic therapy, cryotherapy, and CO2 laser therapy.
Proliferative verrucous leukoplakia
Aggressive behaviour is noticed in this disease. Mostly effected gender is women during her sixth decade of life. Clinically, asymptomatic white and verrucous plaque is seen in this disease.
Oral erythroplakia
It is represented by a single erythematous oral mucosal lesion with high rate of malignancy. Risk factors are alcohol and tobacco. Clinically, appears as solitary erythematous flat lesion. Treatment includes surgical excision, ablation by CO2 laser therapy.
Oral lichen planus
It is an auto-immune chronic inflammatory disease involving skin, oral and genital mucosa. Malignancy rate is low. Frequently occurs in women of middle age. Occurrence involves buccal mucosa, bilaterally and it is usually asymptomatic. Types are reticular, plaque-like, bullous, erosive and atrophic. Wickham’s striae refer to a thin white plaque with reticular subtype. Pain may felt in the atrophic and erosive patterns. Bullae formation occurs in the bullous pattern. Plaque-like type may be observed in smokers. Treatment includes topical steroids.
Oral submucous fibrosis
This disease is characterised by fibrosis and collagen deposition. Has an increased risk of malignant transformation. Etiology relates to betel nut chewing. Clinical examination, we come across pain, dry mouth, burning sensation, dysguesia and trismus. Biopsy is a standard method for histopathological investigation. The four stages seen in this disease are fibrosis, chronic inflammation, progressive atrophy which may lead to degeneration of muscle fibres. The reason for malignant transformation are production of cytokines especially TGFbeta signaling which may lead to activation of immune cells. These events may trigger in alteration in the microenvironment, dysregulation in cell proliferation, differentiation, survival, transformation of the tumour and finally DNA repair function. The therapy includes anti-fibrosis drugs such as IFN-gamma, collagenase and steroids and anti-inflammatory drugs, mouth exercising devices and surgery.
Oral epithelial dysplasia
This type of disorder has an increased malignancy transformation rate. The three tiers are mild, moderate and severe. The recent edition of WHO classification of head and neck tumours as a binary system has been given that suggested high grade and low grade. Architectural changes are loss of intracellular cohesion, irregular stratification, squamous eddies within rete ridges, loss of basal cell polarity, premature keratinisation in single cell, bulbous rete ridges and increased number of mitotic figures. Cytological changes include hyperchromasia, abnormal variation in size and shape of the nucleus, atypical mitotic figures, abnormal variation in size and shape of the cell, and increased nuclear cytoplasm ratio (Table 1).
| S.no | Author | Year | Sample size | Result | Oral pathology |
|---|---|---|---|---|---|
| 1 | G. Hoad-Reddick | 1989 | 233 | 41% positive | Carcinoma |
| Oral cavity inflammation | |||||
| Ulceration associated with denture | |||||
| Cheek biting | |||||
| Retained roots | |||||
| Fibroma | |||||
| Leukoplakia | |||||
| Angular cheilitis | |||||
| Denture stomatisis | |||||
| Hyperkeratosis | |||||
| 2 | Shankargouda Patil | 2017 | 21 | 4 cases positive | Oral submucous Fibrosis |
| 3 | Aditi Sharma et al., | 2013 | 1 | - | Oral submucous Fibrosis |
| 4 | Poonam Malik et al., | 2014 | - | - | Oral submocosal fibrosis |
| Microstomia | |||||
| 5 | Laxman singh et al., | 2011 | 1 | - | Oral submucous Fibrosis |
| 6 | Shital Jalandar Sonune et al., | 2012 | 1 | - | Oral submucous Fibrosis |
| 7 | Dr. Chet an Oswal et al., | 2013 | 1 | - | Oral submucous Fibrosis |
| 8 | Shivangi Gajwani et al., | 2008 | 1 | - | Oral submucous Fibrosis |
| 9 | Saraf V et al., | 2014 | - | - | Oral submucous Fibrosis |
| 10 | Anupama Prasad D et al., | 2012 | 1 | - | Oral submucous Fibrosis |
| 11 | RushadHosi Nariman et al., | 2014 | 1 | - | Oral submucous Fibrosis |
| 12 | Kaira et al., | 2011 | 1 | - | OPMD |
| 13 | Kumar et al., | 2014 | 1 | Hyaluronidase | OPMD |
| 14 | Sheela et al., | 2015 | 1 | Surgery | OPMD |
| 15 | Varghese et al., | 2014 | 1 | Surgery | OPMD |
| 16 | Caculo et al., | 2013 | 1 | - | OPMD |
| 17 | Ibrahim et al., | 2012 | 1 | Corticosteroid | OPMD |
| 18 | Abbasali et al., | 2013 | 1 | Graft | OPMD |
| 19 | Vinayagavel et al., | 2014 | 1 | - | OPMD |
| 20 | Patil and Pati et al., | 2012 | 4 | - | OPMD |
Table 1: Data Summary
Prosthodontics
Patients with OPMD in relation to habits and non-habits should be carefully assist for prosthodontics rehabilitation. Salivary substitutes can be given prior to prosthodontic treatments. Detailed record of the intraoral region is very much important for fabrication of prostheses. Early diagnosis and prompt treatment renders excellent function and esthetics. Dental arch with size, shape, teeth in relation to the position, residual ridge are most important factors in the prostheses. Restricted mouth opening is a factor for prostheses fabrication. Cast and stocked trays play a vital role in prosthodontics rehabilitation. Wellfitted anatomical configuration is essential in final esthetics and function. Stock impression trays and sectional impression trays can be used. Recently, flexible impression trays and digital intraoral scanner are used as trendy methods. Heavy and light body silicone impression metals can be used. In addition, silicone putty and modeling plastic impression combo are also used. Polyether and vinyl ploysiloxane remain the best impression materials in elastic nature due to their self-adherent characteristic feature. Medium or light viscosity elastomeric impression material can be used for the final impression. Materials used in case of flexible impression trays are reversible and irreversible hydrocolloids, border molding materials such as plastic modeling, vinyl polysiloxane, polyethers and elastomeric impression materials. Cobalt-chromium framework is witnessed in swing-lock denture for prosthetic rehabilitation. The above mentioned material has advantages such as structural durability, support, retention and patient friendly. Excellent esthetics can be maintained by sectional complete dentures with a little compromise in tongue movement. Graft stabilizing clips can be used as an oral stent. Easy fabrication, contact makes graft stabilizing clips as an excellent material which can be worn and removed by the patient. Oral physiotherapy also involves wooden spatulas and mouth gags. In addition to custom-made occlusal splints, dentures with extra grooves are used. Elasticity of buccal mucosa can be increased by using the mouth exercising device.
Conclusion
Paucity in literature in relation to prosthodontics rehabilitation is evident. Whatever the prosthodontics rehabilitation is done, it should be in conjunction with cessation of patient’s habits, salivary substitutes used, diet rich in proteins and minerals, vitamin B complex supplements, oral physiotherapy, short wave and microwave diathermy. Recently, digital intraoral scanners might play a pivotal role in recording the accuracy of intraoral region in case of prosthodontics rehabilitation. In order to keep prostheses stable and functionally good, easy use by the patient, three main factors are followed such as periodic follow-up, maintenance of the prosthodontics area and further innovations in related to prosthodontics rehabilitation.
References
- Hoad-Reddick G. Oral pathology and prostheses-are they related? Investigations in an elderly population. J Oral Rehabil. 1989;16:75-87.
[Crossref] [Google Scholar] [PubMed]
- Patil S, Sarode SC, Sarode GS, Bhandi S, Awan KH, et al. Prosthetic rehabilitation of oral submucous fibrosis patients: A systematic review of published case reports and case series. PLoS One. 2017 6;12:e0184041.
[Crossref] [Google Scholar] [PubMed]
- Sharma A, Arora P, Wazir SS. Hinged and sectional complete dentures for restricted mouth opening: A case report and review. Contemp Clin Dent. 2013;4:74-7
[Crossref] [Google Scholar] [PubMed]
- Malik, Poonam, Rathee, Manu. Restricted mouth opening-impressions making. Scholars Journal of Dental Sciences. 2015; 2:24-29.
- Kaira LS, Bharathi SS, Sudhapalii S, Chopra D, Srivastava V. Management of a patient with oral submucous fibrosis having restricted mouth opening: A case report. International Journal of Clinical Dental Science. 2011; 2: 29-35.
- Sonune S, Dange S. Oral submucous fibrosis recuperated with prosthodontics approach approach-A case report. IOSR Journal of Dental and Medical Sciences. 2012; 3: 19-21.
- Oswal C, Gandhi P, Sabane A. Prosthodontic management of surgically treated oral submucous fibrosis using the oral screen prosthesis. IOSR Journal of Dental and Medical Sciences. 2013;1:33-36.
- Gajwani S, Prasad K, Hegde C, Shetty NS, Shetty M, et al. Prosthodontic rehabilitation of an edentulous patient affected with oral submucous fibrosis. J Indian Prosthodont Soc. 2008;8:228-230.
- Saraf V, Shetty V, Anandakrishna GN, Ravindran S, Gangadhar SA. Modified sectional impression technique-clinical report and review. Pravara Medical Review. 2014;6:4-7.
- Prasad DA, Prasad DK, Hegde C. Prosthodontic rehabilitation of a patient with oral submucous fibrosis and microstomia: A case report. NITTE University Journal of Health Science. 2012;2:68-71.
- Kumar S, Krishna P, Nariman R. A sectional impression tray technique for an oral submucous fibrosis patient with limited mouth opening. Journal of Oral Research and Review.2014;6:65-67.
- Hashibe M, Sankaranarayanan R, Thomas G, Kuruvilla B, Mathew B, et al. Body mass index, tobacco chewing, alcohol drinking and the risk of oral submucous fibrosis in Kerala, India. Cancer Causes Control. 2002;13: 55–64.
[Crossref] [Google Scholar] [PubMed]
- Mahajan AD, Tatu RJ, Shenoy NA, Sharma VS. Surgical management of oral submucous fibrosis in an edentulous patient: A procedural challenge. Natl J Maxillofac Surg. 2010;1: 161–163.
[Crossref] [Google Scholar] [PubMed]
- Vastani A, Maria A, Chourasia N, Gupta AS. A simple postoperative oral physiotherapy aid for edentulous patients with oral submucous fibrosis. Plast Aesthet Res. 2015;2: 299–300.
- Le PV, Gornitsky M, Domanowski G. Oral stent as treatment adjunct for oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81: 148–150.
[Crossref] [Google Scholar] [PubMed]
- Warnakulasuriya S, Tilakaratna WM. Oral medicine & pathology: A guide to diagnosis and management. 1st edition. Jaypee Brothers Medical Publishers. 2015. [Crossref] [Google Scholar] [PubMed]
- Fernandes AS, Mascarenhas K, Aras MA. Custom sectional impression trays with interlocking type handle for microstomia patients. Indian J Dent Res. 2009;20:370–373.
[Crossref] [Google Scholar] [PubMed]
- Trivedy C, Warnakulasuriya KAAS, Johnson NW, Peters TJ. Copper content in areca catechu products and oral submucous fibrosis. Lancet 1997;340:1447.
[Crossref] [Google Scholar] [PubMed]
- Haque MF, Meghji S, Khitab U, Harris M. Oral submucous fibrosis patients have altered levels of cytokine production. J Oral Pathol Med 2000;29:123–8.
[Crossref] [Google Scholar] [PubMed]
- Auluck A, Rosin MP, Zhang L Sumanth KN. Oral submucous fibrosis, a clinically benign but potentially malignant disease: Report of 3 cases and review of the literature. JCDA. 2008;74:735–40.
[Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.