Ketamine Versus Standard Opioid Treatment for Acute Pain in the Emergency Department: A Systematic Review and Meta-analysis
General Practitioner, Sabya General Hospital, Jazan City, Saudi Arabia
2 Medical Intern, King Faisal University, Al-Ahsa City, Saudi Arabia
3 Medical Intern, Imam Abdulrahman Bin Faisal University, Al-Khobar City, Saudi Arabia
Published: 30-Dec-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Keywords
Ketamine; Opioid; Acute Pain; ER
Introduction
Acute pain is one of the most common reasons for emergency department (ED) shows with up to 78% of visits including pain as a presenting complaint. Timely, powerful, and compassionate pain management is a critical element of patient care, and opioids are one well-accepted, simply to be had, and the time-tested option to deal with pain in the ED. despite increasing reliance upon opioids for acute analgesia within the ED, oligoanalgesia continues to be commonplace, especially in African people and ladies in addition to the young and the very old. [1]
Acute pain management is an important difficulty in the context of symptomatic care of patients within the emergency department (ED). These days, opioids such as hydro morphine and remifentanil had been used to deal with sufferers with acute ache. Certainly, opioids are the primary life of acute pain management, together with non-steroidal drugs, acetaminophen, gabapentin, and regional remedies. Nonetheless, it isn’t always applicable to administer opioids time and again to patients with acute ache, as they will result in seriously adverse consequences consisting of hypotension and hypoxemia. [2]
Ketamine’s analgesic properties in acute pain likely derive from its reversible antagonism of the N-methyl-D-aspartate receptor, although it exerts consequences on μ-opioid receptors, muscarinic receptors, monoaminergic receptors, γ-aminobutyric acid receptors, and several others. It’s been efficiently used to deal with acute pain in such various situations as sickle cell crises, renal colic, and trauma. Because principal sensitization and impaired descending inhibitory structures do not play as distinguished a position in acute traumatic pain in comparison with persistent pain conditions, the mechanisms for ache relief stem from ketamine’s profound analgesic properties. [3]
Ketamine is presently only U.S. meals and Drug Administration (FDA) approved to be used as an anesthetic agent, both as monotherapy or as an induction agent before using different fashionable anesthetics (FDA, 2017). However, numerous offlabel uses for ketamine have been studied since its discovery inside the Sixties. Recent literature shows that there can be a function for ketamine in managing depression, bipolar disorder, posttraumatic stress sickness, suicidal ideation, refractory continual headache, reputation epilepticus, and acute agitation in the ED. [4]
This work aims to determine the efficacy and safety of Ketamine versus standard Opioid treatment for acute pain patients in the emergency setting.
Literature Review
Our review came following the (PRISMA) statement guidelines. [5]
Study eligibility
The included studies should be in English, a journal published article, and a human study describing acute pain patients. The excluded studies were non-English, or animal studies, or describing acute pain patients in the outpatient setting.
Study identification
Basic searching was done over the PubMed, Cochrane library, and Google scholar using the following keywords: Ketamine, Opioid, Acute Pain, ER.
Data extraction and synthesis
RCTs, clinical trials, and comparative studies, which studied the outcome of the Ketamine group versus Opioid group of acute pain patients, will be reviewed. Outcome measures included the numeric rating scale (NRS score), as a primary efficacy outcome, and on serious adverse effects (SAE rate), as a secondary safety outcome.
Study selection
We found 140 records, 99 excluded based on title and abstract review; 41 articles are searched for eligibility by full-text review; 20 articles cannot be accessed; 9 studies were reviews and case reports; the desired drug not used in 4 studies leaving 8 studies that met all inclusion criteria.
Statistical analysis
After the pooling of data, Odds ratios (OR), Standard Mean Differences (SMDs), with 95% confidence intervals (CI) were calculated, using MedCalc statistical software (Belgium). After the Q test of heterogeneity, the I2-statistics (either the fixedeffects model or the random-effects model) were done within the meta-analysis process.
Results
The included studies were published between 2014 and 2019 [Table 1]. [6-13]
| N | Author | Follow-up duration (min) |
Number of patients | Age (average years) |
||
|---|---|---|---|---|---|---|
| Total | Ketamine group | Opioid group | ||||
| 1 | Beaudoin et al. [6] | 120 | 40 | 20 | 20 | 37.5 |
| 2 | Majidinejad et al. [7] | 15 | 126 | 63 | 63 | 44.3 |
| 3 | Miller et al. [8] | 120 | 45 | 24 | 21 | 30 |
| 4 | Motov et al. [9] | 120 | 90 | 45 | 45 | 35.5 |
| 5 | Bowers et al. [10] | 120 | 116 | 53 | 63 | 42.4 |
| 6 | Mahshidfar et al. [11] | 60 | 300 | 150 | 150 | 34.3 |
| 7 | Takieddine et al. [12] | -- | 20 | 10 | 10 | 32.5 |
| 8 | Motov et al. [13] | 120 | 59 | 29 | 30 | 77.2 |
| #Studies arranged via publication year. | ||||||
Table 1: Patients and study characteristics.
Regarding patients’ characteristics, the total number of patients in all the included studies was 796 patients, with 394 patients in the Ketamine group, and 402 patients in the Opioid group, while their average follow-up time was (65) minutes [Table 1]. The mean age of all patients was (41.7 years) [Table 1].
A meta-analysis study was done on 8 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=796) [Table 2]. [6-13]
| N | Author | Primary outcomes | Secondary outcomes | ||||
|---|---|---|---|---|---|---|---|
| NRS score | SAE rate | ||||||
| Ketamine group | SD | Opioid group | SD | Ketamine group | Opioid group | ||
| 1 | Beaudoin et al. [6] | 4.5 | 3 | 2.5 | 3.3 | 9 | 2 |
| 2 | Majidinejad et al. [7] | 2.7 | 1.8 | 2.4 | 1.5 | 6 | 0 |
| 3 | Miller et al. [8] | 2.67 | 2.07 | 1.71 | 2.21 | 14 | 12 |
| 4 | Motov et al. [9] | 3.9 | 2.9 | 3.7 | 2.9 | 16 | 15 |
| 5 | Bowers et al. [10] | 4.5 | 3.5 | 6.5 | 2.5 | 27 | 12 |
| 6 | Mahshidfar et al. [11] | 4.9 | 3.3 | 3.2 | 2.9 | 51 | 54 |
| 7 | Takieddine et al. [12] | 7 | 2 | 3.5 | 3 | 5 | 6 |
| 8 | Motov et al. [13] | 3.2 | 2.5 | 3.3 | 3 | 9 | 10 |
Table 2: Summary of outcome measures in all studies.
Each outcome was measured by:
Standard Mean Difference (SMD)
• For average NRS score.
Odds Ratio (OR)
• For SAE rate.
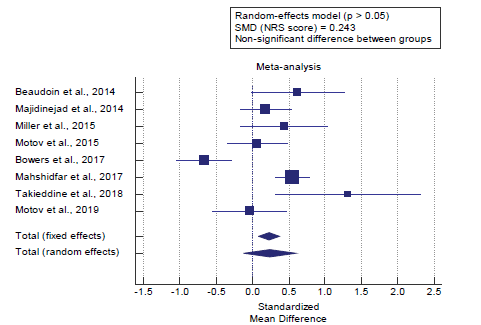
Concerning the primary outcome measure, we found 8 studies that reported NRS scores with a total number of patients (N=796). I2 (inconsistency) was 81.7% with a highly significant Q test for heterogeneity (p<0.001), so random-effects model was carried out; with overall SMD= 0.243 (95% CI=-0.115 to 0.602). Using the random-effects model, the meta-analysis process revealed a non-significant difference in the mean NRS score in the Ketamine group compared to the Opioid group (p>0.05) [Figure 1].
Concerning the secondary outcome measure, we found 8 studies reported SAE rate with a total number of patients (N=796). I2 (inconsistency) was 62% with a highly significant Q test for heterogeneity (p=0.01), so random-effects model was carried out; with overall OR= 1.6 (95% CI=0.863 to 2.996).
Using the random-effects model, the meta-analysis process revealed a non-significant difference in SAE rate in the Ketamine group compared to the Opioid group (p>0.05) [Figure 2]. Our results indicating that ketamine can be considered as an alternative to opioids for short-term pain control.
Discussion
This work aims to determine the efficacy and safety of Ketamine versus standard Opioid treatment for acute pain patients in the emergency setting.
The included studies were published between 2014 and 2019. Regarding patients’ characteristics, the total number of patients in all the included studies was 796 patients, with 394 patients in the Ketamine group, and 402 patients in the Opioid group, while their average follow-up time was (65) minutes.
The mean age of all patients was (41.7 years). A meta-analysis study was done on 8 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=796) [Table 2].
Concerning the primary outcome measure, we found 8 studies reported NRS scores with a total number of patients (N=796).
Using the random-effects model, the meta-analysis process revealed a non-significant difference in the mean NRS score in the Ketamine group compared to the Opioid group (p>0.05). Which came in agreement with, Beaudoin et al., [6] Karlow et al., [1] Bowers et al., [10] Heitz et al., [14] Mahshidfar et al., [11] Miller et al., [8] Motov et al., [15] and Pourmand et al., [16]
Beaudoin et al. reported that sixty patients had been enrolled (n=20 in each group). There had been no differences among study businesses concerning age, sex, race, ethnicity, preenrollment analgesia, or baseline NRS. Over the two- hour submit study medicinal drug administration duration, the pain scores have been better (more pain relief) for the ketamine study groups than the control group (standard care 4.0; group 1 7.0; and group 2 7.8; p<0.02). [6]
Karlow et al. reported that they had been able to use affected person-level data or suggested values to calculate the same old errors inside the exchange of pain scales. This allowed them to directly calculate the standard errors of exchange in NRS pain ratings for those trials. None of the pains established a clinically sizeable difference among reductions in pain scores among ketamine. Absolutely the value of the exchange in the morphine arm changed into subtracted from the absolute price of the change in the ketamine arm. The precise effect estimates and standard errors of the change from baseline to publish intervention NRS rankings for all protected trials are not clinically notably distinctive in any trial; it became 63 in each group and morphine. [1]
Bowers et al. reported that clinically significant variations in NRS scale scoring vary along the scale; smaller changes in suggested values are correlated with scientific importance on the low (nearer to 0) end of the size in preference to the excessive (closer to 10) stop of the scale. Therefore, it is tough in this context to assign scientific importance to the difference in suggested ache scores among agencies, previous statistical evaluation of the NRS scale indicates that these variations are more likely to be clinically significant over time, as reported pain scores decrease. [10]
Heitz et al. reported that there have been 261 sufferers covered from three researches. All research used similar dosing of ketamine, and all use the same dosing of morphine. Ketamine was found to be non-inferior to morphine for acute pain. Primary outcome Numerical rating scale (NRS) or visual analog scale (VAS) within 60 mins: A pooled estimate of the difference between ketamine and morphine equivalents was 0.42. [14]
Mahshidfar et al. reported that, a great decrease was found in pain scores as compared to the baseline scores (P=0.01). At 15 min, pain scores were comparable between both groups (P=0.23). The pain scores until 60 min in the morphine group was better than the ketamine group (P<0.001, respectively). [11]
Miller et al. reported that forty-five subjects were enrolled. Demographic variables and baseline NRS scores (7.1 vs 7.1) were similar. Ketamine was not superior to morphine in the maximum change of NRS pain scores, morphine =5 and ketamine =4.9. [8]
Motov et al. reported that low-dose ketamine did not produce a significantly more reduction in numeric rating scale pain ratings as compared to morphine, but the time to acquire maximum analgesic effect was five min in the ketamine institution compared to one hundred min for the morphine group. Adult patients with an intense ache in a city health center ED established a profound ache reduction in patients who acquired IV. ketamine (15 mg) and 0.5 mg IV. Hydromorphone, the mean and median discount in a 10-point numeric rating scale reduction being 6.0 and 7.5, respectively. [15]
Pourmand et al., reported that Ketamine did not produce a greater reduction in NRS pain scores compared with morphine for acute pain in the ED. However, Ketamine induced a significant analgesic effect within 5 minutes and provided a moderate reduction in pain for 2 hours. [16]
Concerning the secondary outcome measure, we found 8 studies reported SAE rate with a total number of patients (N=796). Using the random-effects model, the meta-analysis process revealed a non-significant difference in SAE rate in the Ketamine group compared to the Opioid group (p>0.05). Which came in agreement with Davis et al., [4] Karlow et al., [1] and Beaudoin et al. [6]
Davis et al., reported that non-dissociative doses of ketamine appear to have a low incidence of unfavorable events, bring about high-quality pain control, and might reduce the need for opioid use inside the ED. Even though the overview affords evidence that ketamine may be useful inside the ED, the authors concluded that greater rigorous investigations and studies are needed to both support or refute the use of no dissociative ketamine for acute pain control in the ED but this difference was non-significant. [4]
Karlow et al. reported that, pain scores analysis revealed that, ketamine was not inferior to morphine (relative reduction=0.42). No SAEs were reported. [1] Beaudoin et al. reported that, as with any other drug, the use of low-dose ketamine for the remedy of pain must be balanced against the ability for adverse activities.
They didn’t discover any severe detrimental occasions that could restrict the use of ketamine in generally healthy adult patients. [6] Our result came in disagreement with Duhaime & Wolfson. Duhaime & Wolfson, reported that, because of heterogeneity in the strategies and timing of pain evaluation and event assessment, adverse occasions have been reported as raw information. Ketamine changed into associated with a higher rate of adverse events than morphine in all the individual studies. Prices of neuropsychological destructive activities of 15.4% within the ketamine institution and 4.4% in the opioid group (relative risk=3.44 absolute risk difference [ARD]=11%, number needed to harm [NNH]=9). [17]
Conclusion
To conclude, Ketamine is non-inferior to morphine for the control of acute pain, indicating that ketamine can be considered as an alternative to opioids for ED short-term pain control.
Competing Interests
The authors declare that they have no competing interests. All the listed authors contributed significantly to the conception and design of study, acquisition, analysis, and interpretation of data and drafting of the manuscript, to justify authorship.
REFERENCES
- Karlow N, Schlaepfer CH, Stoll CR, Doering M, Carpenter CR, Colditz GA, et al. A systematic review and meta-analysis of ketamine as an alternative to opioids for acute pain in the emergency department. Acad Emerg Med. 2018;25:1086-1097.
- Lee EN, Lee JH. The effects of low-dose ketamine on acute pain in an emergency setting: a systematic review and meta-analysis. PloS One 2016;11:e0165461.
- Schwenk ES, Viscusi ER, Buvanendran A, Hurley RW, Wasan AD, Narouze S, et al. Consensus guidelines on the use of intravenous ketamine infusions for acute pain management from the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018;43:456-466.
- Davis WD, Davis KA, Hooper K. The use of ketamine for the management of acute pain in the emergency department. Adv Emerg Nurs J. 2019;41:111-121.
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. Bmj 2009;339.
- Beaudoin FL, Lin C, Guan W, Merchant RC. Low-dose ketamine improves pain relief in patients receiving intravenous opioids for acute pain in the emergency department: results of a randomized, double-blind, clinical trial. Acad Emerg Med. 2014;21:1193-1202.
- Majidinejad S, Esmailian M, Emadi M. Comparison of intravenous ketamine with morphine in pain relief of long bones fractures: a double blind randomized clinical trial. Emergency 2014;2:77.
- Miller JP, Schauer SG, Ganem VJ, Bebarta VS. Low-dose ketamine vs morphine for acute pain in the ED: a randomized controlled trial. Am J Emerg Med. 2015;33:402-408.
- Motov S, Rockoff B, Cohen V, Pushkar I, Likourezos A, McKay C, et al. Intravenous subdissociative-dose ketamine versus morphine for analgesia in the emergency department: a randomized controlled trial. Ann Emerg Med. 2015;66:222-229.
- Bowers KJ, McAllister KB, Ray M, Heitz C. Ketamine as an adjunct to opioids for acute pain in the emergency department: a randomized controlled trial. Acad Emerg Med. 2017;24:676-685.
- Mahshidfar B, Mofidi M, Fattahi M, Farsi D, Moghadam PH, Abbasi S, et al. Acute pain management in emergency department, low dose ketamine versus morphine, a randomized clinical trial. Anesth Pain Med. 2017;7.
- Takieddine SC, Droege CA, Ernst N, Droege ME, Webb M, Branson RD, et al. Ketamine versus hydromorphone patient-controlled analgesia for acute pain in trauma patients. J Surg Res. 2018;225:6-14.
- Motov S, Mann S, Drapkin J, Butt M, Likourezos A, Yetter E, et al. Intravenous subdissociative-dose ketamine versus morphine for acute geriatric pain in the Emergency Department: A randomized controlled trial. Am J Emerg Med. 2019;37:220-227.
- Beaudoin FL, Lin C, Guan W, Merchant RC. Low-dose ketamine improves pain relief in patients receiving intravenous opioids for acute pain in the emergency department: results of a randomized, double-blind, clinical trial. Acad Emerg Med. 2014;21:1193-1202.
- Bowers KJ, McAllister KB, Ray M, Heitz C. Ketamine as an adjunct to opioids for acute pain in the emergency department: a randomized controlled trial. Acad Emerg Med. 2017;24:676-685.
- Heitz C, Morgenstern J, Bond C, Milne WK. Hot Off the Press: A Systematic Review And Meta-analysis of Ketamine as an Alternative to Opioids for Acute Pain in the Emergency Department. Acad Emerg Med. 2019;26:946-948.
- Mahshidfar B, Mofidi M, Fattahi M, Farsi D, Moghadam PH, Abbasi S, et al. Acute pain management in emergency department, low dose ketamine versus morphine, a randomized clinical trial. Anesth Pain Med. 2017;7.
- Miller JP, Schauer SG, Ganem VJ, Bebarta VS. Low-dose ketamine vs morphine for acute pain in the ED: a randomized controlled trial. Am J Emerg Med. 2015;33:402-408.
- Motov S, Rosenbaum S, Vilke GM, Nakajima Y. Is there a role for intravenous subdissociative-dose ketamine administered as an adjunct to opioids or as a single agent for acute pain management in the emergency department? J Emerg Med. 2016;51:752-757.
- Pourmand A, Mazer-Amirshahi M, Royall C, Alhawas R, Shesser R. Low dose ketamine use in the emergency department, a new direction in pain management. Am J Emerg Med. 2017;35:918-921.
- Duhaime MJ, Wolfson AB. Ketamine Versus Opioids for Acute Pain in the Emergency Department. Acad Emerg Med. 2020.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.