Knowledge and Practices Regarding Nosocomial Infection among Nurses in Hospitals of Islamabad
2 Department of Health Services Academy Islamabad, Quaide Azam University, Islamabad, Pakistan, Email: muhmmad.abdullah2@scholar.aku.edu
3 Department of Health services, Shifa Tameer e Millat University Islamabad, Pakistan
4 Shifa International hospital Islamabad, Pakistan Shifa Tameer E Millat University Islamabad, Pakistan
Received: 13-Jul-2021 Accepted Date: Jul 20, 2021 ; Published: 10-Aug-2021
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Title: Knowledge and practices regarding Nosocomial infection among nurses in hospitals of Islamabad. Objectives: Objectives of the study were to determine the level of knowledge and practices regarding Nosocomial infection among nurses working in public and private hospitals of Islamabad and to determine the factors associated with knowledge and practices among these nurses. Design: A cross sectional study based on self-administered questionnaire was ducted. Setting: Study was carried out in public and private tertiary teaching hospitals in Islamabad. Study Participants: A sample of 356 nurses including 185 from public hospital and 171 from private hospital through stratified random sampling proportion to size for collecting information regarding knowledge and practices about Nosocomial infection was selected. Main outcome measures of the study were good and bad knowledge and practices regarding Nosocomial infection. Results: A total sample size was 356 participants was studied where 185(51%) nurses from public hospital and 171(48%) from private hospitals were included. Most of the participants, 212 (59.6%) were of age between 20-29 years. Among the participants 221(62.1%) were females and 135 (37.9%) were male staff. Regarding knowledge level, 194(54.5%) participants had good knowledge about Nosocomial infection and as far as practice is concerned, 204(45.5%) of the participants had good practices regarding Nosocomial infection. Conclusion: Overall, the knowledge and practices of the nursing staff was good. Based on facility, knowledge of the private hospital was better as compare to knowledge of the participants of public hospital however, practice of the participants from public hospital was better as compare to the practice of the participants from private hospital.
Backgorund
With the increase in number of health problems, there is increase in number of healthcare facilities both public and private.
Medical staff working in hospitals is at greater risk of hospital- acquired infections as they frequently provide medical care to the patients with certain infections.
Even though there is development in the health care system, the risk to Hospital-Acquired Infections (HAIs) still persist.[1]
HAIs infections are one of the main preventable health related issue [2] both for patient safety and medical staff. Approximately, 2 million each year in United States are infected by HAIs which leads to 80,000-90,000 death. However, there is no figure available for HAIs’ impact on the health care staff.
There are three main types of infection which account for 80% of all the HAIs in the Intensive Care Unit (ICU). These infections are urinary tract infection, bloodstream infection and pneumonia.
There are multiple types of Nosocomial infections, the most common of them are:
Urinary tract infections are those hospital acquired infections in which an indwelling urinary catheter (Foley Catheter) was in place for more than two calendar days when all elements of the UTI infection criterion were first present together, with day of device placement being on Day 1,and an indwelling urinary catheter was in place on the date of event or the day before. [3] A surgical site infection is an infection that occurs after surgery in the part of the body where the surgery took place. Surgical site infections can sometimes be superficial infections involving the skin only. Other surgical site infections are more serious and can involve tissues under the skin, organs, or implanted material.
While in case of pneumonia where the patient is on mechanical ventilation for more than two calendar days when all elements of the Pneumonia infection criterion were first present together, with day of ventilator placement being day 1, and the ventilator was in place on the date of event or the day before. If the patient is admitted or transferred into a facility on a ventilator, the day of admission is considered day 1. [3] Blood Stream Infections (BSI) are considered among the most important
Nosocomial infections in human patients because of the resulting prolongation of hospital stay and increased mortality. Although a 46% decrease in Central Line Associated Blood Stream Infection (CLABSIs) has occurred in hospitals across the US from 2008-2013, an estimated 30,100 Central Line-Associated Blood Stream Infections (CLABSI) still occur in intensive care units and wards of US acute care facilities each year. CLABSIs are serious infections typically causing a prolongation of hospital stay and increased cost and risk of mortality.
It is vital for the care of hospitalized and critically ill patients, as they provide reliable venous access for clinical activities such as blood sampling, infusion of medications, and hemodynamic measurement. However, Central Venous Catheter (CVCs) is also the leading cause of healthcare- associated Bloodstream Infections (BSIs) and is frequently implicated in life-threatening illnesses (CDC, 2016). [4]
The microorganisms transmitted through direct or indirect contact. Direct is the transfer of organisms by contact with contaminated hands. Indirect is the transfer or organisms through fomites. Certain pathogenic organisms such as MRSA, Clostridium difficile, and Vancomycin-resistant enterococci can be transmitted directly through contact with infected or colonized patients, or indirectly through contact with potentially contaminated items or surfaces. Isolation of the patient is essential and can limit the transmission of organisms. In addition protective clothing, including gloves and aprons, should be worn by health staff. [3]
Blood borne is transmitted through sexual transmission, injury or inoculation. The main concerns in healthcare settings are the transmission of HIV, Hepatitis B and C through sharp injuries or blood splashes. The other route of transmission of microorganisms via inhalation of small particles that remain suspended in the air for long periods of time and can be widely dispersed by air currents. Since organisms transmissible through the air can be widely dispersed, specific air ventilation is required to manage their dispersion. Techniques include the use of monitored negative airflow ventilation with at least six air changes per hour and filtration of direct exhaust to the outside. The cost and inconvenience of treating cases of cross infection is much higher. Droplet is also a type of mode transmission of microorganisms during close contact with infected persons who may be sneezing, coughing, talking, or undergoing airway procedures such as intubation or bronchoscopy. Its particles are larger and therefore do not remain suspended in the air. The Organisms transmitted by droplet require close contact. Measures to limit cross infection include placing the patient in a single room or having at least three feet between patients; wearing of surgical masks by staff coming within three feet of the patient, and the wearing of a mask by the patient, when they leave their designated area.
The microorganisms are transmitted through food, water, drugs, blood or other solutions. Common vehicle transmission can be prevented by utilizing aseptic, sterile or clean techniques whenever fluids or medications are being made up or given to patients, and by utilizing good principles of food hygiene.
Nosocomial infections are spread via negligence of health care workers or by not following the safety protocols. Nosocomial infections are usually caused by transmission of pathogens from one patient to another by means of health care workers who do not wash their hands while checking between patients or those who do not follow the infection control measure such as use of gloves, hand disinfectants. Studies show that hand washing is a useful technique in reducing the incidence rate of Nosocomial infections. However, the healthcare worker does not comply with the safety practice, which put both patients and workers themselves at the risk of acquiring the infections. Health care workers compliance with the hand washing and the use of disinfectants remain low, and this is true especially in the care of Pakistan. Pakistan is one of the developing countries and health care personal’s attitudes and knowledge toward the safety measure is not encouraging.
Low compliance is linked with lack of awareness or health related knowledge among health care personnel. Other factors which impact the practices include logistics measures, budgeting and organizational environment. Organizational or personal failure to implement the correct practices are one of the main reasons in increasing incidence rate of Nosocomial infections both among patients and health care workers. There are multiple reasons for non-compliance such as drying of skin because of usage disinfectant, overloaded with work, and wards being patient full and understaffing. Lack of knowledge regarding safety practices and infection control among health care workers decrease compliance of those safety practices. [5]
Lower level knowledge and unsafe practices lead to health and economic problem for the patients as well as their families. It can also put health care staff at risk. Pakistan is one of the developing countries where health care personnel’s knowledge and practices towards the safety measures are not encouraging. Results of the study will be useful for policy makers and healthcare authorities to make and implement future health innovations.
The objectives of the study were, to determine the level of knowledge and practices regarding Nosocomial infection among nurses working in public and private hospitals of Islamabad. To determine the factors associated with knowledge and practices among these nurses working in public and private hospitals in Islamabad.
Hospitals are considered to be safe places for diagnosis and treatment of all types of diseases however, paradoxically, they are transformed into centers for creation and transmission of various infections. [6] With the advancement of technology and environmental changes the infections have also been increasing. Nosocomial infections are one of the common infections around the globe. Nosocomial infections are also known as hospital acquired infections. [7] According to World Health Organization (WHO) guide on prevention of hospital-acquired infections, Nosocomial infections are defined as“An infection acquired in hospital by a patient who was admitted for a reason other than that infection. An infection occurring in a patient in a hospital or other healthcare facility in whom the infection was not present or incubating at the time of admission. This includes infections acquired in the hospital but appearing after discharge and also occupational infections among staff of the facility”. Nosocomial infections are result of complications of patient care within the hospital. [8] At first the ideas of Nosocomial infection arise in fourteenth century when in Europe the first hospital was inaugurated. Infections which occur after 48-72 hour are usually classified as Nosocomial infections. If any infection occurs less than 48 hours after hospitalization, there is the probability that the patient might have been in the incubation period of the infection. [6] Nosocomial infections occur globally and affect the population both in developed and developing world. Globally, Nosocomial infections occur among 7%-12% of the hospitalized patients with more than 1.4 million people suffering from the infectious complications acquired in the hospital. [7,8] The risk for acquiring the infection raise from 7%-12% to 15%-20% for the patient who are present in Intensive Care Units (ICU). Prevalence survey regarding Nosocomial infections under the sponsorships of WHO in 55 hospitals of 14 countries representing 4 WHO Regions (Europe, Eastern Mediterranean, South-East Asia and Western Pacific) was carried out. According to this study, it was reported that the highest frequencies of Nosocomial infections were reported from hospitals which were located in Eastern Mediterranean and South-East Asia regions with the prevalence of 11.8% and 10.0% respectively.
Impact of nosocomial infections
Hospital acquired infections not only affect the physical health of the patient but also lead to functional disability and emotional stress of the patients; may also lead to poor quality of life. Nosocomial infections are one of the leading causes of death. With advances in health care system, threat to Nosocomial infections still remains as they continuously affect hospitalized patients and which ultimately results into high morbidity and mortality rates, and also additional costs for long hospital stay, [6,8] increased hospital stay, longer diagnostic procedure and therapeutic interventions. The increased length of stay of infected patient is related to increase in the cost of the and overall excess utilization of resources. Additionally, prolonged stay in hospitals not only increases the direct cost such as hospital expenses but also indirect cost which occur because of unproductive or loss of work. These infections pose healthcare system problems globally specifically in the developing world.
Risk factors
There are various other factors, which increase the risk of acquiring the infection. These factors are age (neonates and geriatrics are most at risk), patients who have undergone surgery, those with immune system problems, chronic illness such as diabetes, cancers, renal failures, hepatitis cirrhosis.
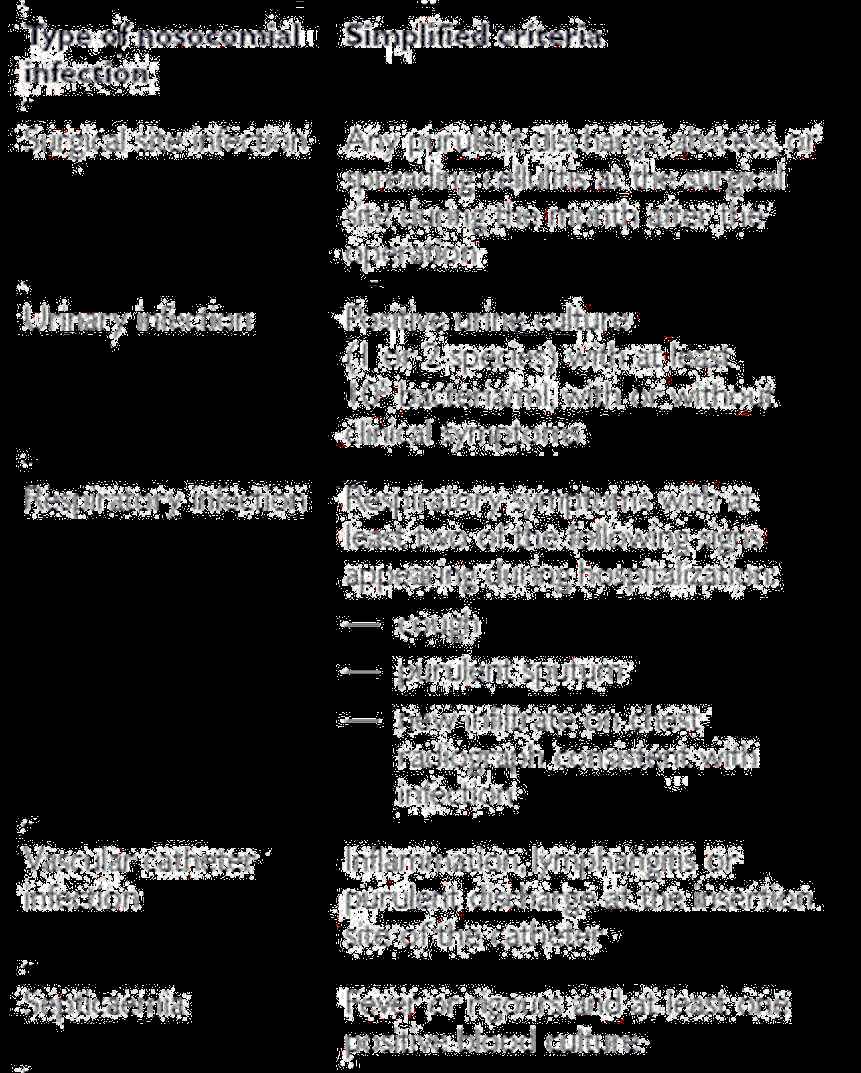
Nosocomial infections can be endemic or epidemic. There are various types of Nosocomial infections. The following figure 1 provides types of most common Nosocomial infections and their definitions.
The most common Nosocomial infection is urinary tract infection. Urinary tract infections are associated with less morbidity but it can sometimes lead to bacteremia and death. Other most common Nosocomial infections are surgical site infections which occur mostly during operations or other surgical treatments. The incidence rate for surgical site infections ranges from 0.5% to 15%. Following Pie Chart 1 is for the distribution of most common Nosocomial infected sites which was created according to 1996 French national prevalence survey.
Methodology
A cross sectional study was conducted in Islamabad, capital of Pakistan. The study population was staff nurses of the public and private tertiary care hospitals of Islamabad.
• Diploma holding and graduate nurses who have at least 6 months post qualification-working experience.
• Public and private Tertiary care hospitals working in more than 500 patients’ bedded hospital.
Exclusion criteria
• Nurses working at Armed Forces hospitals
• Tehsil Head Quarter hospitals nurses (THQ)
• Rural Health Unit nurses (RHU) will be excluded from study
• Outpatient department
• Obs/gyne
Sampling unit was a staff nurse working in tertiary care hospitals of Islamabad.
Sampling frame
Lists of all staff nurses working in a public and a private hospital in Islamabad.
Study was carried out in one public sector and one private sector hospital in Islamabad. Islamabad had an estimated population of around 1.67 million in 2011, which according to the estimate of population census organization will rise to around 2 million in 2020.
Health care institutions in Pakistan are not sufficient to meet the requirements of the increasing number of patients, most of the people dependent on private and public hospitals. in public facilities are insufficient due to increasing number of population day by day according to planning and development division at present there are 149201 registered doctors in the country which means for each 1206 people there is just one doctor and there are only 76244 registered nurses and only 1665 people there is one patient bed in the hospital [Figure 2].
For the purpose of data collection, two tertiary healthcare facilities were targeted.
• Pakistan Institute of Medical Sciences (PIMS)
• Shifa international hospital
Pakistan Institute of Medical Sciences (PIMS)
PIMS is the largest tertiary public teaching hospital in Islamabad. PIMS functions as a national reference center and provides specialized diagnostic and curative services. The hospital has 30 major medical departments. PIMS is divided into five administrative branches. Islamabad hospital is the major component with a 592-bed facility and 22 medical and surgical specialties. The main objective of the hospital is to provide medical coverage to community of Islamabad and Rawalpindi region as well as in pocket areas including Gilgit Baltistan, Azad Kashmir, Khyber Pukhtonkhwa (KPK) and North Punjab region. Another objective is to facilitate research in the health sector, more than 1200 out patients are registered daily and among them average 60 daily admissions the number of patients in emergency is more than 200. Children hospital is also component of this hospital where daily attendance of outpatients is more than 400, daily admissions is 30 and more than 100 patients avail emergency treatment on daily basis. Maternal and child health is also important component objective of MCH is to reduce maternal mortality rate by promoting safe motherhood in targeted areas. It also offers different teaching programs for medical students including doctors, nurses, technicians, and different research etc.
Shifa international hospital
In private sector, Shifa is one of the best private tertiary care teaching hospitals in Islamabad. It offers quality care and provides leadership, teaching and research. There are 19 different CPSP approved postgraduate programs, where 227 consultants 224 PGs, more than 600 paramedical and nursing staff are working. There are more than 35 different departments i.e. neurology, Neurosurgery, plastic surgery, General surgery, immunology, orthopedics, medicine, surgery, aperitif, dermatology ENT and emergency etc.
Nursing division is committed to high quality patient care it extend nursing services to 560 beds including 32 Neonatal intensive units, 65 adult intensive care units 20 beds for day care chemotherapy and 17 for day care surgery.
In 2015 annual report 6 million patients were registered more than 200 liver transplant surgeries has been done total 176000 surgeries performed and total new births 24000 were reported.
Under the umbrella of Shifa international hospital external service department there are 2 more hospitals are working.
• Shifa international hospital G10/4 is the first post stroke rehabilitation unit in Pakistan and this hospital is also performing urology surgeries that are sponsored by Pakistan kidney institute. This hospital is providing free of cost all medical, surgical and dialysis facilities to needy people which includes in and out patients.
• Shifa international hospital Faisalabad is the first hospital which introduced 64 slides Toshiba CT scan for patients.
Shifa provides holistic care and many patients get treatment free of cost with the support of Shifa foundation.
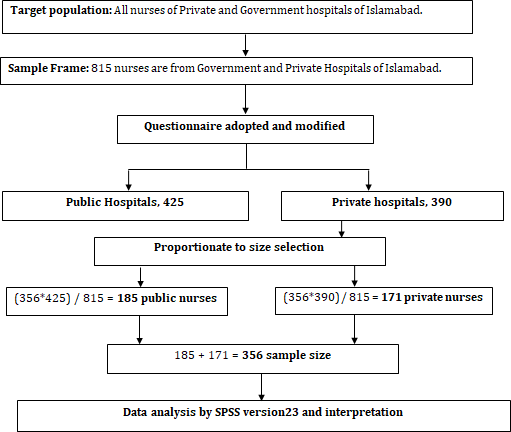
Sampling strategy stratified random sampling technique was used for this study. At first two tertiary care hospitals, one from public and other from private sector were selected.
From each hospital, a sampling frame of the nursing staff of different departments meeting the inclusion criteria of the study was developed.
For this purpose, list of nurses was obtained from nursing director office of the PIMS (Pakistan Institute of Medical Sciences) and Shifa international hospital.
Then proportion to size stratified based on type of facility, stratified random sample as per the calculated size was selected using computer generated random numbers shown in Figure 3.
Operational definition
For this study, Nosocomial infection was defined as Infection acquired after 48 hours of admission and the patient is free of it at the time of admission
Sample size was calculated by using WHO software for sample size determination in health studies, using the formula for sample size in the case of a population proportion with absolute precision.
Sample size calculation was calculated based on the assumption that 50% of the staff nurses had knowledge regarding Nosocomial infection with 95% Confidence level and with 5% absolute precision.
The total sample size was 356 comprising of 185 nurses from public hospital and 171 from private hospital on the basis of proportion to size selection
Data was collected within two months duration, from May to June 2016. A self-administered questionnaire in English was used to collect information. Informed consent was taken from all the selected participants.
An orientation regarding purpose of study and filling up of the questionnaire was given and thereafter questionnaire was distributed to the participants and the participants filled the questionnaire. The questionnaire developed in English and it was anonymous.
This tool was adapted from the research study conducted in India and permission and most of items in the questionnaire were included from practice guide lines of World Health Organization (WHO) 2nd edition. [9]
The final form of questionnaire was based on three different sections in which each question followed by different kind of distracters.
For instance, first section of Knowledge Practices Assessment Questionnaire (KPAQ) provides information of staff demographics, second section of KPAQ represents items about knowledge for Nosocomial infection and third section represents items regarding practices of Nosocomial infection.
In the questionnaire, some of the questions (stem) were connected with different number of distracters and some of the questions were further divided into yes and no questions. Following Table 1, represent the division of each question according to their domains.
| Domain 1 | Items: |
| Demographics | 1-8, 10 |
| Domain 2 | Items: |
| Knowledge | 9, 12-24, 26-28 |
| Domain 3 | Items: |
| Practices | 11, 25, 29-44 |
Table 1: Domains of the Knowledge Practices Assessment Questionnaire (KPAQ)
A codebook was formulated for the questionnaire to be a reference for analysis. Data entry and data analysis was done using Statistical Package for the Social Sciences (SPSS) version 23.0. Coding and data entry was done at the end of each day. In case of any missing values, discrepancies or errors, respondents were contacted and missing information was corrected. After completing the data entry, the data was double checked for consistency, completeness, and errors. The variables were re-categorized where necessary.
Statistical analysis
All the data was entered and analyzed using SPSS 23.0. Validity and quality of the data was cross checked using range and frequency tables in order to look for foul-entered or missing data. For categorical data, cross tabs were used to check for potential errors. If there was an error, the questionnaire was rechecked for corrections. Knowledge regarding nosocomial infection was measured using 17 items scale. The knowledge was further developed into new variable, which is knowledge score. The score was calculated after adding up each item. The score ranged from 1-26 where 1 was the lowest score and 26 was the highest score. Knowledge score was further categorized into poor knowledge and good knowledge based on median score. The median was 13.5 of knowledge score (1-26) so the score 14 or above was categorized in good knowledge and score below 14 was categorized into poor knowledge.
Practices regarding Nosocomial infection were measured using 18 items scale. The practices were further developed into new variable which is practice score. The score was calculated after adding up each item within this scale. The score ranged from 27-39 where 27 was the lowest score and 39 was the highest score. Practice score was further categorized into poor practices and good practices based on median score. The median was 33 so the score 33 or above was categorized in good practices and score below 33 was categorized into poor practices. The data was analyzed in 2 phases. In first phase, descriptive analysis was carried out for all the background/demographic characteristics of the study population. For analysis of the categorical data like gender, education, and designation frequencies and percentages were used. Second phase of the analyses was on inferential statistics. To know whether there is a statistically significant difference or not in categorical variables by age, gender and type of facility, Chi square test was used. A significance level of p=0.05 was used for all the statistical analysis, unless specifically mentioned.
Trustworthiness of the study
Face and content validity of the study was ensured to increase the trustworthiness of the study. The reliability of the study was ensured using test-retest technique during pilot study by collecting information at two different times by the same respondents. Protocol of the study was followed in order to get the best results. [10] In order to enhance content validity of items of Knowledge Practices Assessment Questionnaire (KPAQ), it was requested to four infection control content experts and three research experts to give their feedback in refining the items, formatting and appropriate use of language in order to make Knowledge Practices Assessment Questionnaire (KPAQ) simple and understandable for nursing staff. All reviewers are well qualified and well experienced and in the light of their feedback items in the Knowledge Practices Assessment Questionnaire (KPAQ) were finalized. [11]
In ethical consideration Institutional Review Board (IRB) of Al-Shifa school of public health, Al-Shifa trust Rawalpindi, approved the study protocol. Permission was obtained from the administration/ Director of the respective hospital. Before collection of data, Informed consent was taken from all the participants. An orientation of the selected participants was conducted to explain the objectives of the study and what they have to do as participants. All the participants were informed about their right to withdraw from the study at any point. In addition to that participants could refuse to answer any question they think would create problem for them. Confidentiality of the data was ensured. No one except the researcher and supervisor had the access to the questionnaire or any data related to the study. The data was saved in password-protected files. This study did not involve any kind of psychological or physical harm to the participants. However, at any point, if the participant experience emotional disturbance or unpleasant recall, data collection was stopped at the moment to provide the emotional support. The data collection was resumed later when convenient. The participants of the study have right of access to their results of the study. [12]
Results
A Total 356 participants out of them 185(51%) from public hospital and 171(48%) from private hospital Islamabad, participated in the study. Among those, 221(62.1%) were females and participants 212(59%) were of age between 20-29 years. 240(67.4%) out of 356(100%) who had diploma in nursing and working as nursing staff were 304(85.4%). Most of the participants 152(42.7%) were working in critical areas out of 356(100%) majority of the participants 264(74.2%) had total post qualification experience less than 5 years and current experience of 264(74.2%) was less than 5 years . Most of the staff 226(63.5%) were assigned 10 to 20 beds [Table 2].
| Variable | Public | Private | Total | |
|---|---|---|---|---|
| n=185(51%) | n=171(48%) | N=356(100%) | ||
| Gender | Female | 125(67.6%) | 96(56.1%) | 221(62.1%) |
| Male | 60(32.4%) | 75(43.9%) | 135(37.9%) | |
| Age (in years ) | 20-29 | 71(38.4%) | 141(82.5%) | 212(59.6%) |
| 30-39 | 80(43.2%) | 26(15.2%) | 106(29.8%) | |
| 40-49 | 28(15.1%) | 3(1.8%) | 31(8.7%) | |
| 50-59 | 6(3.2%) | 1(0.6%) | 7(8.7%) | |
| Qualification | Diploma in | 119(64.3%) | 121(70.8%) | 240(67.4%) |
| nursing | ||||
| Post-graduation | 66(35.7%) | 50(29.2%) | 116(32.6%) | |
| Designation | Management | 22(11.9%) | 30(17.5) | 52(14.6%) |
| Non-management | 163(88.1%) | 141(82.5%) | 304(85.4%) | |
| Department/ward | Critical care unit | 71(38.4%) | 81(47.4%) | 152 (42.7) |
| Medical unit | 64(34.6%) | 3822.2%) | 102(28.7%) | |
| Surgical unit | 25(13.5%) | 24(14.0%) | 49(13.8%) | |
| Emergency | 25(13.5%) | 28(16.3) | 53(14.88) | |
| Total post Qualification Experience |
Below 5 years | 79(42.7%) | 142(83.0%) | 221(62.1%) |
| Above 5 years | 106(57.7) | 29(17.0%) | 135(37.9%) | |
| Current hospital experience | Below 5 years | 110(59.5%) | 154(90.1) | 264(74.2%) |
| Above 5 years | 75(40.5) | 17(9.9%) | 92(25.8%) | |
| Total patient beds | 10-20 beds | 115(62.2%) | 111(64.9%) | 226(63.5%) |
| 21-50 beds | 70(37.8%) | 60(35.1%) | 130(36.5%) | |
Table 2: Demographic characteristics of the study participants n=356.
Over all distribution of knowledge and practices of nursing staff
A total 356(100%) participants including males and females participated in the study. Among them 194(54.5%) had good knowledge regarding nosocomial infection and 164(45.5%) had good practices [Table 3].
| Characteristics | Frequency | Total | |
|---|---|---|---|
| N=356(% age) | N= 356 | ||
| Knowledge | Good knowledge | 194(54.5%) | 356(100%) |
| Bad knowledge | 162(45.5%) | ||
| Practice | Good practice | 204(57.3%) | 356(100%) |
| Bad practice | 152(42.7%) | ||
Table 3: Distribution by knowledge and practices of nursing staff.
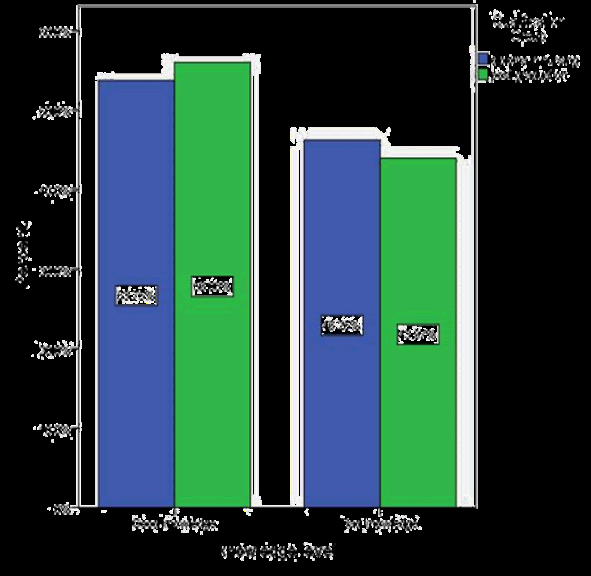
Distribution of knowledge and practice with respect to type of facility
A total 356 participants from public and private hospital participated in the study and out of them, 95(51.4%) had good knowledge while 129(67.7%) participants from private hospital had good practice regarding nosocomial infection. Statistically, there is no significant difference between good and bad knowledge of the participants of public and private hospitals [Table 4].
| Characteristic | Public | Private | Total | P value | |
|---|---|---|---|---|---|
| n=185 | n=171 | N=356 | α=0.05 | ||
| Knowledge | Good knowledge | 95(51.4%) | 99(57.5%) | 194(54.50%) | 0.258 |
| Bad knowledge | 90(48.6%) | 72(42.1%) | 162(45.5%) | ||
| Practices | Good practice | 129(69.7%) | 75(43.9%) | 204(57.3%) | 0 |
| Bad practices | 56(30.3%) | 96(56.1%) | 152(42.7%) | ||
Table 4: Knowledge and practices by type of facility.
Distribution of knowledge and practices by Gender
A total male participants 135(37.92%) among them 75 (55.6%) had good knowledge and 80(59.3%) had good knowledge regarding Nosocomial infection. Statistically, there is no significant difference between good and bad knowledge and good and bad practices of the participants of public and private hospitals [Table 5].
| Characteristic | Female | Male | Total | P value | |
| n=221 | n= 135 | N=356 | α=0.05 | ||
| 62.02% | 37.92% | 100% | |||
| Knowledge | Good knowledge | 119(53.5%) | 75(55.6%) | 194(54.5%) | 0.838 |
| Bad knowledge | 102(46.2%) | 60(44.4%) | 162(45.5%) | ||
| Practices | Good practice | 124(56.1%) | 80(59.3%) | 204(57.3%) | 0.636 |
| Bad practices | 97(43.9%) | 55(40.7%) | 152(42.7%) | ||
Table 5:Distribution of knowledge and practices by gender.
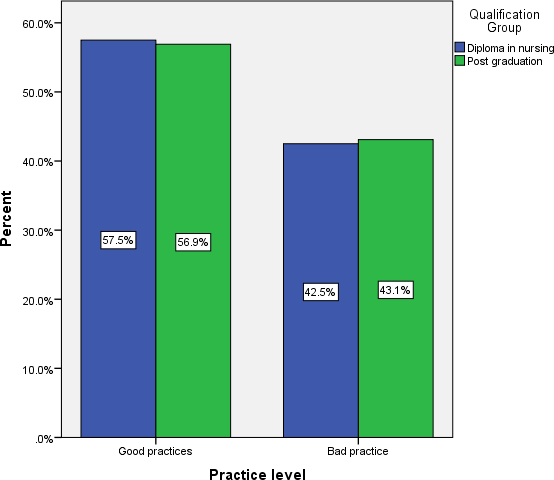
Those participants who had diploma in nursing, 53.75% had good knowledge while 56.03% of the participants who had bachelor’s degree had better knowledge [Graph 1].
Among those who had diploma in nursing 57.5% had good practices as compare those who had bachelor’s degree in nursing [Graph 2].
Those participants who had more than 5 years’ experience (68.15%) had good practice as compare to those who had experience less than 5 years [Graph 3].
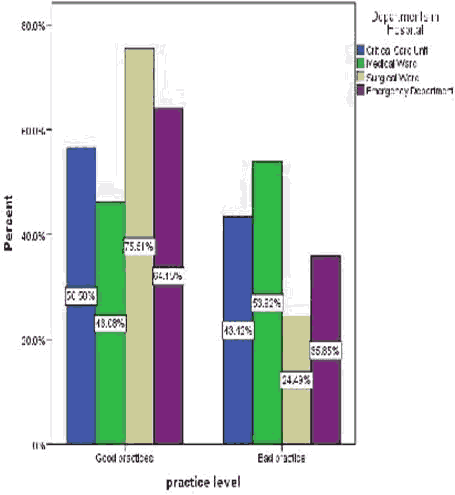
Regarding practices, (75.51%) who were working in surgical department had good practice than those working in other departments. Moreover, 53.92% participants from medical unit had bad practices regarding Nosocomial infection [Graph 4].
A total of participants 356 among those who had less than 5 years of experience of nursing had good knowledge (54.3%) and 54.8% of the participants who had more than 5 years of experience had good knowledge level [Graph 5].
Discussion
The study was aimed to determine the level of knowledge and practices regarding nosocomial infections among nurses working in public and private hospitals in Pakistan. The main findings of the study were that 1) 54.5% of the nurses reported to have good knowledge regarding nosocomial infections 2) 57.3% of the nurses were following good practices to cater nosocomial infections. Overall we did not observe major difference in the knowledge and practices of nursing staff working in a hospital setting.
Regarding knowledge, we observed that 54% had good knowledge. The observed proportion of knowledge level was higher as compared to proportion reported in other studies. For instance, a study from India reported that only 50% nurses had good knowledge.
Among study participants, the majority of participants (59%) were aged between 20 and 29 years which is similar to the percentage of participants in a study conducted in Ethiopia and in India. And 51% participants were from public sector hospital and rest was from private sector hospital. Most of the participants (85.4%) were diploma holders and 42.7% of the participants were working in critical care units. Majority of the participants (74%) had post qualification experience of less than 5 years which is different from the percentage of participants in a study conducted in Khartoom in 2009 which is 44%. And among the participants, 63.5% were assigned on average 15 beds per shift of duty.
According my study most of the participants (42.4%) were of the opinion that urinary tract infection is the most common type of nosocomial infection. My results are different from a study conducted in India, which reported that according to 61.4% UTI is the most common Nosocomial infection. According to another study in India 98.8% participants reported that respiratory tract infection was the most common type of nosocomial infection.
In my study the 8.1% of the participants reported that air born is the most common mode of transmission while the study which was conducted in India reported that 88% participants revealed that nosocomial is spread because of air born. According my study 58.4% participants reported that nosocomial is high-risk problem in our society but my results are different from the study, which was carried out in India. Study reveals that 86.8% of the participants reported that they can get infection from the patients and my results are different from the study conducted in India which states that 56.2% participants reported that they can acquire infection from patients. According to my study 64.9% of the nurses participated in activities of infection control committee and these results are similar to study conducted in Ethiopia where 65.6% of the participants were involved in different activities of infection control committee. In my study 99.2% of the participants took precautionary measures before starting any procedure and these results are very high compared to the study carried out in Ethiopia where 26.6% participated regularly use precautionary measures. Among 356(100%) 97.5% of the participants follow universal precaution to prevent Nosocomial infection which is higher than the percentages reported in the study conducted in Ethiopia,where 42% staff use universal precaution. According to my study 97.5% staff washes hands after removal of glove a study conducted in Africa shows similar results.
According my study 39.6% staff recapped syringes after use, which is lower than the percentage reported in another study, conducted in 2015, which indicated 62.5% staff recapped syringes after use. According my study 74.4% of the staff disposed sharps needles in the sharp container. Results of my study are similar to a study conducted earlier in, where 79.2% disposed sharps in safety box. In my study 71.6% staff follows guidelines for hand washing.
Among the participants, 54.5% had good knowledge regarding nosocomial infections. The percentage of nurses with good knowledge in my study is greater than that of a study carried out in India. My study indicates that 45.5% of the participants had good practices regarding nosocomial infection control. This percentage of the participants with good practices is lower than reported in a study in 2015.
There was statistically no significant difference between public sector and private sector nurses regarding good and bad knowledge about nosocomial infections. It is important to note that in our study, the participants from public sector hospital had good practices regarding nosocomial infections than those from private sector hospital. This is because the nurses in public hospitals are more exposed to variety of patients and are bound to follow preset guidelines and proper protocol devised by the government authorities. Secondly, they have numerous opportunities to participate in seminars, walks, and other activities regarding nosocomial infections. Regarding gender of the participants, there was no statistically significant difference among male and female participants regarding good and bad knowledge, and good and bad practices. These results might be due to the similar demographic characteristics and similar working environment of the participants.
In so as the qualification of the participants is concerned, the participants with post graduate qualification, (56.03%) had overall good knowledge regarding Nosocomial infection than the diploma holder participants. This is because the participants with higher qualification are more aware of the facts and figures about nosocomial infections, their epidemiology, route of transmission, prevention etc. As for as the practice of the participants regarding nosocomial infections is concerned, the post graduate nurses had less percentage of bad practices and this is due to better knowledge of the post graduate participants.
The study is unique because of the following features:
• Both Public and private teaching hospitals were included in the study.
• Almost all the departments of tertiary care hospitals were included in the study.
• Simple random sampling technique was used.
Limitations
Despite various strengths, there were certain limitations in the study:
• Study was conducted for short time period.
• Only tertiary care hospitals were included.
• Limited only one region of Pakistan.
Recommendation
• Regular inspection and follow up from the stakeholders regarding infection control practices.
• Regular training sessions should be conducted for nursing staff.
• Additional concerns should be given to the availability and quality of personnel protective equipment.
• Further studies are essential in the evaluation of the situation of infection in different areas of hospitals.
• Sessions should be conducted regarding infection control for the nurses.
Conclusion
The overall knowledge and practices of the nursing staff was good among them knowledge of the private hospital was better as compare to knowledge of the participants of public hospital while practice of the participants from public hospital was better as compare to the practice of the participants from private hospital.
Funding
Self-funding student project.
Conflict of Interest
No conflict of interest was declared.
REFERENCES
- Suchitra JB, Devi NL. Impact of education on knowledge, attitudes and practices among various categories of health care workers on nosocomial infections. Indian J Med Microbiol. 2007;25(3),181.
- Safdar N, Abad C. Educational interventions for prevention of healthcare-associated infection: A systematic review. Crit Care Med. 2008;36(3), 933-940.
- World Health Organization (WHO). Weekly epidemiological record, hepatitis c-Global prevalence. 2001;75(3):18-20.
- Centers for Disease Control and Prevention (CDC). National and state healthcare associated infections progress report. Atlanta. GA: Centers for Disease Control and Prevention. 2014
- Sodhi K, Shrivastava A, Arya M, Kumar M. Knowledge of infection control practices among intensive care nurses in a tertiary care hospital. J Infect Public Health.2013;6(4):269-275.
- Faraji R, Mirzaei S, Eftekhari A, Lahiji AP, Bamakan MHM, Rad, HK. A study of nurses’ observance rate of hygienic principles and nosocomial infections control. Int J Res Med Sci. 2016;4(4):1163–1166.
- Ducel G, Fabry J, Nicolle L. (2002). Prevention of hospital acquired infections: A practical guide. Prevention of hospital acquired infections: A practical guide (2nd Edn). World Health Organization (WHO). 2002
- Sheth AM, Jani DS, Rangoonwala MM, Kadri AM. Assessing the awareness and practice of Hospital Acquired Infections (HAIs) among nursing staff of Civil Hospital, Rajkot, Gujarat, India. Int J Res Med Sci. 2015;3(8):1844-1850.
- WHO. Removing obstacles to healthy development: report on infectious diseases. World Health Organization. 1999.
- Tavolacci MP, Ladner J, Bailly L, Merle V, Pitrou I, Czernichow P. Prevention of nosocomial infection and standard precautions: Knowledge and source of information among healthcare students. Prevention. 2008;29(7), 642-647.
- Sax H, Perneger T, Hugonnet S, Herrault P, Chraïti MN, Pittet D. Knowledge of standard and isolation precautions in a large teaching hospital. Infect Control Hosp Epidemiol. 2005;26(3):298-304.
- Motamed N, Baba Mahmoodi F, Khalilian A, Peykanheirati M, Nozari M. Knowledge and practices of health care workers and medical students towards universal precautions in hospitals in Mazandaran Province. East Mediterr Health J. 2006;12(5):653-661.






 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.