Knowledge, Attitudes, and Practice of Medical Students Regarding Occupational Risks of Hepatitis B Virus in College of Medicine, Aljouf University
- *Corresponding Author:
- Dr. Ahmad H Al-Hazmi
Department of Family Medicine, College of Medicine, AlJouf University, P.O. Box 2014, Sakaka 75741, Saudi Arabia.
E-mail: ahhazmi@hotmail.com
Abstract
Background: Medical students represent a population that is at high‑risk group for acquiring and spreading hepatitis B infection (HBV). Aim: This study was designed to evaluate the knowledge and attitudes among male student regarding occupational risks of HBV infection. Subjects and Methods: During March 2013, a descriptive cross‑sectional study was conducted on medical students of AlJouf University College of Medicine. Structured questionnaires of 16 different statements concerning knowledge base of HBV, attitudes as well as practices toward occupational risks of hepatitis B were distributed to 120 students. Results: Response rate of 76.7% (92/120) yielded 92 questionnaires for analysis. Majority of the students surveyed 62.0% (57/92) perceived that they are at high risk of contracting and spreading HBV. The rate of this perception among students who had a history of training on universal precautions was more than that found among those who did not have (70.8% vs. 58.8%; P < 0.01). Most of the students surveyed 63.0% (58/92) considered vaccine is safe and more than half 52.2% (48/92) were vaccinated against HBV. There were a very strong agreement about needlestick 92.4% (85/92) and blood 87.0% (80/92) as efficient modes of HBV transmission. Seventy‑two percent of the participants did not have any knowledge about post‑exposure prophylaxis for hepatitis B. A significant relationship was found between students who had a history of training on universal precautions and knowledge about post needlestick injury (P < 0.01). Conclusion: Infectious occupational risk of hepatitis B remains a challenge for medical students and the foundations of the medical institutes. Students must complete an infection control training before they start their clinical education.
Keywords
Attitudes, Hepatitis B, Knowledge, Medical students, Saudi Arabia
Introduction
Hepatitis B virus (HBV) is one of the major diseases of mankind.[1] Globally, over 2 billion people have been infected with HBV, and there are over 350 million carriers.[1,2] HBV is one of the most common infectious diseases without seasonal distribution.[2] The virus is transmitted in the blood and fluids, which can be diagnosed during acute and chronic phases.[2,3] Acute infection may cause nonspecific symptoms or fulminant hepatitis that may die or requires urgent liver transplantation.[1-3] Chronic infection causes death associated with cirrhosis, liver failure, or hepatocellular carcinoma.[3] HBV ranks second, after tobacco, on the list of known carcinogenic agents affecting humans.[4] Furthermore, infection with HBV constitutes the first etiology of hepatocellular carcinoma and the tenth leading cause of death globally.[4]
Medical students are a group of health care workers (HCWs) that are at high risk to get and spread HBV because their activities involve contact with patients or blood or other body fluids in healthcare, laboratories or public-safety settings.[5-7] The risk varies during their career, but it is often the highest during their professional training.[5,6] It was assumed that medical students studying in AlJouf University College of medicine are lacking the important knowledge about and the appropriate practice toward infectious, occupational risks of HBV. Although many studies in different countries have been conducted, there have been very few attempts to evaluate the knowledge, attitudes and practice of undergraduates studying in Saudi Arabia regarding occupational risks of HBV.[5,6,8] Therefore, this study had the objective of evaluating knowledge base, attitudes and practice of undergraduates regarding occupational risks of HBV.
Subjects and Methods
During through 27th March 2013 “a cross-sectional descriptive study was carried out among students of AlJouf University College of Medicine, which was established in 2008 and has admitted students annually into a 7-year degree course in medicine” There were around 120 medical undergraduates of first to final year studying in this college all of them are males. One hundred and twenty newly designed self-administered anonymous, confidential questionnaires with explanatory letters were distributed to students. All students selected and evaluated for the present study. The study protocol was discussed and approved by the research and ethical committee in AlJouf University College of Medicine. The questionnaire comprised of 24 “closed-ended questions.” The first part covered demographic characteristics of students (age, years in college, family history of HBV, etc.). The second part contained 16 with variable items 2-15 focusing on students’ knowledge base, attitudes, and the most important points regarding the occupational risks of HBV. The well-structured questionnaire was developed to assess the KAP of male students regarding infectious, occupational risks of HBV. The study questions and the characteristics of participants were based on previous surveys and articles with similar objectives.[5-10] For validating the questionnaire, specific experts in standardizing questionnaire, microbiologists, community medicine, gastroenterologists, hepatologists, and biostatistics, confirmed the introduction and validity contents of the primary questionnaire. Some questions were omitted according to their advice. The questionnaire comprised of 24 “closed-ended questions.” The first part covered demographic characteristics of students (age, years in college, family history of HBV, etc.). The second part contained 16 with variable items 2-15 focusing on students’ knowledge base, attitudes, and the most important points regarding the occupational risks of HBV.[1,7]
On 3-7 January 2013, a questionnaire was pre-tested during a pilot study that was conducted among 35 students. This was done to ensure clarity, relevance, and determine the amount of time needed to answer all items. The results of the pre-test were evaluated critically, and some modifications were accordingly made. The average time needed to fill all items in the questionnaire was about 15 min. Results of a pilot study were not included in the final analysis.
Data analysis
Data were analyzed using SPSS packed version 17.0 (IBM SPSS Inc., Chicago, IL, USA). P <0.05 was considered as significant; Chi-square test was applied for analysis of categorical data. Mean standard deviation (SD) and proportions were used to describe continuous and dichotomous data, respectively.
Results
Of 120 questionnaires distributed, 92 (76.7% response rate) were collected and analyzed. The general characteristics of students surveyed are shown in Table 1. The entire study group was males (no female students in this college), and the majority 77.2% (71/92) were in the pre-clinical stage. The pre-clinical to clinical ratio in this study was found to be 3.38, with mean (SD) age was 22.2 (2.24) years, range 17-27 years. Family history of HBV was positive in 10.9% (10/92) of the students and 26.1% (24/92) of them received training about infection control, and 17.4% (16/92) had history of needlesticks.
| Variable | n | Percentage |
|---|---|---|
| Age groups (years) | ||
| 17-20 | 6 | 6.5 |
| >20-23 | 59 | 64.1 |
| >23-26 | 26 | 28.3 |
| >26 | 1 | 1.1 |
| Stage of training | ||
| Preclinical | 71 | 77.2 |
| Clinical | 21 | 22.8 |
| Having a family member infected with HBV | ||
| Yes | 10 | 10.9 |
| No | 82 | 89.1 |
| Having a complete vaccination against | ||
| hepatitis B (3 doses) | ||
| Yes | 48 | 52.2 |
| No | 10 | 10.9 |
| Not sure | 34 | 37.0 |
| HBV: Hepatitis B virus |
Table 1: Basic data regarding the study group (male students)
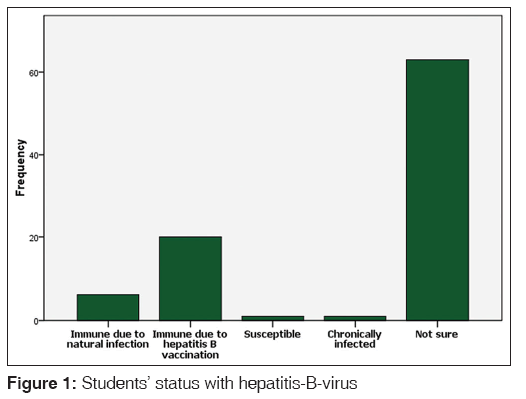
Majority of the students surveyed 62.0% (57/92) believed that they were at high risk of contracting and spreading HBV. Fifty-eight 63.0% considered HB vaccine is safe for all ages, and 52.2% (48/92) were vaccinated. When asked about their own HBV status. It is found only 30.4% (28/92) students knew their own HBV status. Immune due to HB vaccination ranked first among 21.7% (20/92) followed by 6.5% (6/92) immune due to natural infection. Whereas, one (1.1%) student was chronically infected and one (1.1%) was susceptible to infection with HBV [Figure 1].
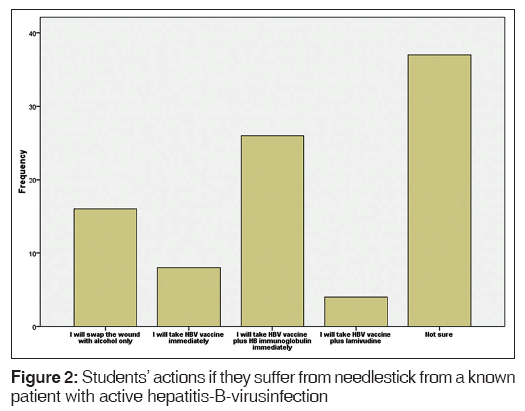
Table 2 shows students’ correct answer rates on knowledge about HBV distributed by their training stage (clinical and pre-clinical). Overall, only 41.0% of the answers were correct. HBV is resistant to alcohol, and some detergents were recognized by minority of the students 28.3% (26/92) and HBV is 100 times transmissible than HIV was recognized by 34.8% (32/92) of the same sample. Whereas only 37.0% (34/92) students knew that HBV could be infectious outside the body (e.g. in the environment). On the bases of their stage of training, students in the clinical stage have better knowledge than students studying in the preclinical stage regarding HBV transmission that is 100 times transmissible than HIV P < 0.01. Furthermore, students in the clinical stage have better knowledge about site of HBV replication than students studying in the preclinical stage P < 0.01. When inquired about what should they do if they suffer from needlestick from a known patient with active HBV infection. It is found, only 28.3% (26/92) of the students responded that they will take HBV vaccine with HBV immunoglobulin immediately, 17.4% (16/92) will swap the wound with alcohol only, 8.7% (8/92) will take hepatitis B vaccine immediately and 4.3% (4/92) will take vaccine plus lamivudine. While, 40.2% (37/92) students were not sure about their action [Figure 2]. A significant relationship was found between students who had a history of training about universal precautions and their appropriate actions after an accidental needlestick injury from a patient with known active HBV infection (50% vs. 20.9%; P < 0.01).
| Question item: (Correct answer) | Correct;n=92 (%) | Stage of training | P | χ2 | |
|---|---|---|---|---|---|
| Preclinical n=71 | Clinical n=21 | ||||
| HBV is 100 times transmissible than HIV (T) | 34.8 | 28.2 | 57.1 | <0.01 | 5.625 |
| Hepatitis B is resistant to alcohol and some detergents (T) | 28.3 | 25.4 | 38.1 | 0.45 | 1.481 |
| HBV could be an infectious outside the body (e.g., in the environment) (T) | 37.0 | 37.0 | 39.4 | 0.39 | 0.988 |
| Acute infection may cause nonspecific symptoms (T) | 45.7 | 42.3 | 57.1 | 0.81 | 3.99 |
| HBV replicates (in the liver) | 42.4 | 40.9 | 47.6 | <0.01 | 8.636 |
| The consequences of infection with viral hepatitis B could be (all of the above) | 57.6 | 54.9 | 66.7 | 0.34 | 3.008 |
HBV: Hepatitis B virus
Table 2: Correct answer rate on the basis of knowledge of students about HBV
Students’ responses on different aspects of measures that might help to prevent hepatitis B transmission are shown in Table 3. Wearing disposable medical gloves ranked first suggested by majority of the participants 79.3% (73/92); followed by vaccination against HBV among 73.9% (68/92). Whereas sterilization (e.g. surgical instruments) considered by 72.8% (67/92). There were no statistical significant differences found between the students’ responses on different aspects of measures that might help to prevent hepatitis B transmission and their clinical stages (P > 0.05).
| Measures that might help to preventhepatitis B transmission | Agreen=92; (%) | Stage of training (%) | P | χ2 | |
|---|---|---|---|---|---|
| Preclinical n=71 | Clinical n=21 | ||||
| The existence of a vaccine for HBV | 68 (73.9) | 50 (54.3) | 18 (19.6) | 0.13 | 4.044 |
| Sterilization (e.g., surgical instruments) | 67 (72.8) | 50 (54.3) | 17 (18.5) | 0.56 | 1.1501 |
| Routine blood screening for HBsAg | 66 (71.7) | 47 (51.1) | 19 (20.7) | 0.05 | 5.9569 |
| Wearing disposable medical gloves | 73 (79.3) | 56 (60.9) | 17 (18.5) | 0.92 | 0.169 |
| Condom use | 52 (56.5) | 35 (38.0) | 17 (18.5) | 0.09 | 6.569 |
| Not share toothbrushes or razors | 57 (62.0) | 42 (45.7) | 15 (16.3) | 0.08 | 4.951 |
| Ensuring of safe injection practices | 66 (71.7) | 48 (52.8) | 18 (19.6) | 0.23 | 2.907 |
| Clean blood spills with detergent | 64 (69.6) | 48 (52.8) | 17 (18.5) | 0.07 | 7.213 |
HBV: Hepatitis B virus, HBsAg: Hepatitis B surface antigen
Table 3: Knowledge of students regarding preventive measures about HBV
Regarding the possible modes for HBV transmission [Table 4], 92.4% (85/92) reported through NSIs, 87.0% (80/92) through blood, 70.7% (65/92) during delivery from the infected mothers to their infants, 52.2% (48/92) sexual contact, 43.5% (40/92) through saliva followed by breast milk 41.3% (38/92). About drinking from the same cup used by an infected person, only 34.8% (32/92) of the students think it could transmit the infection. While, 42.4% (39/92) of the students considered sharing the same toilet with an infected person is safe. In this study, the overall knowledge of modes of HBV transmission was only (57.1%). Significant difference on knowledge between students who had training on universal precautions and those who did not have was observed regarding transmission of HBV through blood (P < 0.01).
| Statement | Number (%) | ||||
|---|---|---|---|---|---|
| Agree | Disagree | Not sure | |||
| Modes of hepatitis B transmission | |||||
| Needlestick injuries | 85 (92.4) | 2(2.2) | 4(4.4) | ||
| Could be transmitted in the blood | 80 (87.0) | 6(6.5) | 5(5.4) | ||
| Semen and vaginal secretions are modes of transmission | 48 (52.2) | 23(25.0) | 19(20.7) | ||
| Infected mothers during delivery to their infants | 65 (70.7) | 14(15.2) | 12(13.0) | ||
| An infected mother may transmit HBV to her new born baby through breast milk | 38 (41.3) | 26(28.3) | 27(29.3) | ||
| You may get HBV by drinking from the same cup used by an infected person | 32 (34.8) | 36(39.1) | 23(25.0) | ||
| HBV could be transmitted in saliva | 40 (43.5) | 32(34.8) | 19(20.7) | ||
| You may get HBV by sitting on a toilet seat used by an infected person | 32 (34.8) | 39(42.4) | 20(21.7) | ||
| Hepatitis B vaccine | |||||
| Is safe for people of all ages | 58 (63.0) | 6(6.5) | 26(28.3) | ||
| The duration of protection is at least 15 years and based on current scientific evidence, lifelong | 35 (38.0) | 17(18.5) | 38(41.3) | ||
| The complete vaccine series induces protective antibody levels in >95% of infants, children | 64 (69.6) | 4(4.3) | 21(22.8) | ||
| and young adults | |||||
| Hepatitis B vaccine can be given safely together with any other vaccine, and vice versa | 42 (45.7) | 12(13.0) | 36(39.1) | ||
| Pregnancy is a contraindication for use of this vaccine | 26 (28.3) | 14(15.2) | 50(54.3) | ||
| Attitude items | |||||
| Do you accept hepatitis B infected student or colleague in the same work place or classroom? | 52 (56.5) | 21(22.8) | 18(19.6) | ||
| I have concern in shaking hands or hugging a person infected with HBV infection | 26 (28.3) | 44(47.8) | 21(22.8) | ||
| Caring for a patient with hepatitis B would make me feel uncomfortable | 45 (48.9) | 33(35.9) | 12(13.0) | ||
| I would not mind eating from the same plate with a person with hepatitis B | 32 (34.8) | 41(44.6) | 18(19.6) | ||
| Chronic infection with HBV is shameful | 18 (19.6) | 48(52.2) | 25(27.2) | ||
| More attention should be offered to the occupational risk of HBV | 55 (59.8) | 16(17.4) | 20(21.7) | ||
| Training programs about occupational risk of HBV should be offered to all medical students | 68 (73.9) | 8(8.7) | 15(16.3) | ||
| Health care professionals should receive hepatitis B vaccination | 61 (66.3) | 12(13.0) | 17(18.5) | ||
HBV: Hepatitis B virus
Table 4: Knowledge of students about transmission, vaccination and their attitudes about HBV
Students’ responses on different aspects of attitudes toward HBV are shown in Table 4. Majority of the students surveyed 73.9% (68/92); believed that training programs regarding occupational hazards of HBV are very important to all medical students. Sixty-one 66.3% suggested that, all HCWs should receive hepatitis B vaccination. Whereas, eating from the same plate with a person infected by HBV was agreed by only 34.8% (32/92). Of the participants, having a colleague or student in the same classroom or working place was accepted by 56.5% (52/92) of the students.
Discussion
HBV is a major cause of dreadful liver diseases.[1] Fortunately, infection with this virus is not only treatable but also preventable.[1,3] Medical students can play an important role in the safety from the occupational infections like HBV.[6,9] They can raise their awareness and improve skills to prevent infectious, occupational risk due to HBV.[9] The current study is, to the best of the author’s knowledge, the first comprehensive College setting-based study carried out in Saudi Arabia (AlJouf province) to obtain data on knowledge, attitudes, and practice of the undergraduates towards occupational risk of HBV. We believe that our sample was representative of the students and accounted for more than three-fourths of all students studying in college of medicine at AlJouf University.
This study, clearly, proves that majority of medical students were aware of the existence of an infectious, occupational risk due to HBV. It was found most of the participants 57 (62.0%) believed that they were at high risk of contracting and spreading HBV. Fifty-five (59.8%) claimed that more attention should be offered to the occupational risk of HBV and 68 (73.9%) suggested establishing “training programs about occupational hazards of HBV for all medical students”. Our findings are in agreement with, and support, those internationally that revealed; firstly, the infected students may not only go through immense sufferings because of this, but may also act as a potential source of infection to patients handled by them.[5] Second, the need to train students in preventive practices regarding infectious risk of HBV, universal precautions to handle the needles or cutting objects, and to protect oneself against secretions, should be taught and emphasized.[6,8] Our study has shown that, the overall knowledge of medical students toward infectious, occupational risks of HBV was inadequate. Attributable reasons could be inadequate training programs on prevention and control of HBV. In this study only 37.0% students knew that HBV could be infectious outside the body (e.g. in the environment), and only 34.8% of the same sample knew that HBV is 50-100 times transmissible than HIV.[7,11] These findings highlight lack of knowledge that persists among the students in these aspects, because HBV is highly infectious and easily transmissible pathogen and can survive in dried blood for up to a week.[7,8,11] Of all the participants, only 28.3% recognized that HBV is resistant to alcohol and some detergents indicating more confusion and lack of knowledge among the majority of medical students in this aspect.[11] Our findings are in agreement with those internationally that revealed firstly; HCWs such as medical students receive incomplete and variable training in infection control.[12] Second, 90.9% of medical University students reported that their education about standard precautions was insufficient and expressed their desire for more training.[10,11] Thirdly, of greater concern is the lack of proper education and awareness on HBV among all health care providers, including doctors.[13] Fourthly, the mean knowledge levels of the medical students are partially toward HBV infection.[9]
It is well-documented that medical students sustain needlestick injuries at a rate comparable with other hospital personnel.[14] They are at greater risk of needlestick injuries because they have less experience and expertise in medical procedures.[8,15] Our findings indicate that the majority of our students appeared unaware of the proper action after needlestick injury.[7] We found; only 26 (28.3%) students surveyed will take HBV vaccine with HBV immunoglobulin immediately after needlestick injury from patient who is known with active HBV infection.[7,12] Our findings are not dissimilar to a survey recently conducted among medical students of Karachi, Pakistan.[15] The referred study revealed that 76% of participating medical students did not have any knowledge about the post-exposure prophylaxis for hepatitis B and C.
Scientific knowledge regarding modes of HBV transmission is of great value for medical students to optimize prevention.[9,11,14,15] Our findings have revealed that majority of the responses indicate adequate knowledge regarding some modes of HBV transmission for example (needlestick injuries 92.4%, blood 87.0%).[11,12] For specific modes of transmission for example (saliva 43.5%, breast milk 41.3%, sexual 52.2%) there were inadequate awareness among the majority of the students.[3,12,15] Misconceptions and confusion regarding HBV transmission that persist among the participants may hinder with their safety and might lead to harmful events for their patients and families because HBV has unique virulent infectious characteristics.[7,11,13]
In the area of vaccination against HBV, it was encouraging to find the majority (63.0%) of medical students considered HBV vaccine is safe for people of all ages.[5,8,11] Also, more than 2/3rd (69.6%) of the same sample knew that the complete vaccine series induces protective antibody levels in ≥90% of infants, children and young adults.[5,8,11] It is well-underscored that the need for HBV vaccination among all medical students should be a priority.[5,6,8] In our study, we found only 52.1% medical students have been vaccinated and 37% were not sure. Whereas 10.9% reported that they had never received HBV vaccine. The finding of 52.1% vaccination in our undergraduates was inadequate and less than a study done in Brazil 59.3%,[8] but higher than the study done in Sweden 40%,[16] Bangladesh (40.7%),[5] Faculty of Medicine in Belgrade 24.1%,[17] Nigeria 2.6%.,[6] Regarding those (n = 34; 37%) who were not sure about their previous vaccination. This finding is supporting and in agreement with a recently conducted study at the University of New South Wales, Sydney that examined self-reported vaccination among medical students. The referred study revealed that students had poor specific knowledge of their previous vaccinations.[14] Those (n = 10; 10.9%) who have never received HBV vaccine they should be protected and should receive 3 doses of the HBV vaccine.[6,7,13,18]
Upon admission to the school of medicine, history of vaccination against HBV and serological markers of HBV infection (HBsAg, anti-HBs and anti-HBc) should be determined.[6,8,19] In our study, we have found only 28 (30.4%) students surveyed knew their own HBV status; immune due to hepatitis B vaccination ranked first among 20 (21.7%) students, followed by 6 (6.5%) immune due to natural infection. Fortunately, it was found only one (1.1%) student was chronically infected and (1.1%) one was susceptible to infection with HBV. The finding that, 1.1% of students had chronic hepatitis B infection was very important and that student should be considered infective.[14] Also, determination of post-vaccination serum anti-HBs on a regular basis should not be neglected.[6]
It is very important that, medical students should be encouraged and supported to take all precautions necessary to control and prevent infectious, occupational risks of HBV.[20,21] These include vaccination and use of universal precautions for infection control.[21] It was encouraging to find most of the responses have revealed a suitable awareness about methods of HBV prevention among majority of the students surveyed. It was found a strong agreement about wearing disposable medical gloves 79.3% followed by vaccination against HBV 73.9%. As such, it is well-documented that, the most effective measure for the prevention of HBV infection and its consequences is vaccination against hepatitis B.[1,3,9] Regarding use of disposal medical gloves appears to reduce the risk to HCWs by protecting against incidence of blood-borne infections.[22,23] This study has shown ambivalent attitudes among undergraduates toward HBV. Almost half (n = 45; 48.9%) reported that caring for a patient infected with hepatitis B would make them feel uncomfortable. Eighteen (19.6%) believed with stigma that attached with HBV patients, and more than 1/4th (n = 26; 28.3%) of the same sample reported that they have a concern in shaking hands or hugging a person infected with HBV infection. The proportion of positive believes toward HBV among students in the clinical stages are more than that found among those in the preclinical stages in most items of attitudes, but, all of them are not reaching statistical significance. Our findings could be explained by lack of knowledge about HBV could influence attitudes towards HBV. These findings are in agreement with a recently conducted study in Guilan University (Medical Sciences), Rasht, Iran.[9] The referred study revealed that, students’ attitudes toward HBV and HCV was positively correlated with their mean knowledge level; however, the higher knowledge is associated with a better attitude.
Strengths of the current study included is the first comprehensive College setting-based study carried out in Saudi Arabia (AlJouf province) to obtain data on knowledge, attitudes, and practice of the undergraduates toward occupational risk of HBV. Also, it refers to a common health problem and targets high risk group which can have a significant influence on a serious health concern. Moreover, it is the first local estimates of coverage the level of HBV vaccination among medical students studying in this part of Saudi Arabia. In spite of our findings in this study, we acknowledge its limitations; actually, this is a relatively small scale study among medical students covering one medical college (containing no females). Also, all the information that we got are reported, which do not necessarily reflect the actual state of clinical decision among the participants. In conclusion, those responsible for health care policy in Saudi Arabia need to establish more effective strategies to decrease the infectious, occupational risks of HBV among medical students. Such students should be screened for seromarkers of HBV, trained better in the control and prevention of HBV infection and prophylactic vaccinations against HBV should be compulsory for them.
Acknowledgments
I am grateful to all medical students in AlJouf province of Saudi Arabia who participated in the study and special thanks for Professor Ibrahim Tahir and Professor Tariq Metwally for their help in structuring the questionnaire.
References
- Schillie S, Murphy TV, Sawyer M, Ly K, Hughes E, Jiles R, et al. CDC guidance for evaluating health-care personnel forhepatitis B virus protection and for administering postexposure management. MMWR Recomm Rep 2013;62:1-19.
- Abedi F, Madani H, Asadi A, Nejatizadeh A. Significance of blood-related high-risk behaviors and horizontal transmission of hepatitis B virus in Iran. Arch Virol 2011;156:629-35.
- Wilkins T, Zimmerman D, Schade RR. Hepatitis B: Diagnosis and treatment. Am Fam Physician 2010;81:965-72.
- Causse X, Delaunet A, Si Ahmed SN. Anaes practice guidelines for vaccination against hepatitis B virus: Impact on general practitioners. Gastroenterol Clin Biol 2009;33:1166-70.
- Ahmed MS, Chowdhury OA, Chowdhury AR, Khatoon M. Seroprevalence of HBs antibody among the newly admitted medical students in Bangladesh and seroconversion one year after vaccination. Bangladesh Med Res Counc Bull 2010;36:41-2.
- Odusanya OO, Meurice FP, Hoet B. Nigerian medical students are at risk for hepatitis B infection. Trans R Soc Trop Med Hyg 2007;101:465-8.
- Singhal V, Bora D, Singh S. Hepatitis B in health care workers: Indian scenario. J Lab Physicians 2009;1:41-8.
- Oliveira LC, Pontes JP. Frequency of hepatitis B immunity and occupational exposures to body fluids among Brazilian medical students at a public university. Rev Inst Med Trop Sao Paulo 2010;52:247-52.
- Mansour-Ghanaei R, Joukar F, Souti F, Atrkar-Roushan Z. Knowledge and attitude of medical science students toward hepatitis B and C infections. Int J Clin Exp Med 2013;6:197-205.
- Askarian M, Memish ZA, Khan AA. Knowledge, practice, and attitude among Iranian nurses, midwives, and students regarding standard isolation precautions. Infect Control Hosp Epidemiol 2007;28:241-4.
- Kordi R, Wallace WA. Blood borne infections in sport: Isks of transmission, methods of prevention, and recommendations for hepatitis B vaccination. Br J Sports Med 2004;38:678-84.
- Askarian M, Yadollahi M, Kuochak F, Danaei M, Vakili V, Momeni M. Precautions for health care workers to avoid hepatitis B and C virus infection. Int J Occup Environ Med 2011;2:191-8.
- Nwokediuko SC. Chronic hepatitis B: Management challenges in resource-poor countries. Hepat Mon 2011;11:786-93.
- Torda AJ. Vaccination and screening of medical students: Results of a student health initiative. Med J Aust 2008;189:484-6.
- Khan N, Ahmed SM, Khalid MM, Siddiqui SH, Merchant AA. Effect of gender and age on the knowledge, attitude and practice regarding hepatitis B and C and vaccination status of hepatitis B among medical students of Karachi, Pakistan. J Pak Med Assoc 2010;60:450-5.
- Dannetun E, Tegnell A, Torner A, Giesecke J. Coverage of hepatitis B vaccination in Swedish healthcare workers. J Hosp Infect 2006;63:201-4.
- Denic LM, Ostric I, Pavlovic A, Dimitra KO. Knowledge and occupational exposure to blood and body fluids among health care workers and medical students. Acta Chir Iugosl 2012;59:71-5.
- Alavian SM, Izadi M, Zare AA, Lankarani MM, Assari S, Vardi MM. Survey of the level of anti-HBs antibody titer in vaccinated Iranian general dentists. Spec Care Dentist 2008;28:265-70.
- Fernandes L, Burnett RJ, François G, Mphahlele MJ, Van Sprundel M, De Schryver A. Need for a comprehensive, consistently applied national hepatitis B vaccination policy for healthcare workers in higher educational institutions: A case study from South Africa. J Hosp Infect 2013;83: 226-31.
- Reis JM, Lamounier Filho A, Rampinelli CA, Soares EC, Prado Rda S, Pedroso ER. Training-related accidents during teacher-student-assistance activities of medical students. Rev Soc Bras Med Trop 2004;37:405-8.
- Maroof KA, Bansal R, Parashar P, Sartaj A. Do the medical, dental and nursing students of first year know about hepatits B? A study from a university of North India. J Pak Med Assoc 2012;62:25-7.
- Pido B, Kagimu M. Prevalence of hepatitis B virus (HBV) infection among Makerere University medical students. Afr Health Sci 2005;5:93-8.
- Ciorlia LA, Zanetta DM. Hepatitis B in healthcare workers: Prevalence, vaccination and relation to occupational factors. Braz J Infect Dis 2005;9:384-9.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.