Knowledge of Electromyography (EMG) among Sub-Saharan African Patients - A Pilot Survey
2 Blossom Medical Centre/WFNR Centre for Neuro-rehabilitation, Nigeria, Email: philipab8@yahoo.com
3 Benjamin Carson (Snr) Schools of Medicine, Babcock University, Ilishan-Remo, Nigeria
4 Monitor Healthcare Limited, Nigeria
5 Department of Medicine, University of Ibadan/University College Hospital,Ibadan, Nigeria
Citation: Adebayo PB, et al. Knowledge of Electromyography (EMG) among Sub-Saharan African Patients - A Pilot Survey. Ann Med Health Sci Res. 2018; 8: 69-73
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Electromyography (EMG) is one of the common diagnostic procedure in neurology but still scarce in sub-Saharan Africa. Objective: This cross-sectional study evaluated the knowledge of EMG among patients undergoing this procedure, considering the type, quality and reliability of the information they have. Methodology: Consecutive patients who underwent EMG for the first time between 2014 and 2016, at the WFNR/Blossom Medical Centre Ibadan, Nigeria were interviewed prior to their test. Data on patient’s demography, type of referring physicians were collated. Knowledge of EMG was also assessed. A patient was considered “informed” if she/he knew, at least, that the EMG is a test that uses an electric current or a needle, that it may be painful or cause discomfort, and that it is used to study the function of muscles and nerves. Descriptive and inferential statistics were performed to know the determinants of EMG knowledge. Result: 55 patients. 32 males and 23 females (mean ages 48.69± 18.32 and 43.30±14.88 respectively) were interviewed. Twenty-three (41.8%) patients were adjudged informed about the nature of EMG while 32 (58.2%) were uninformed about the procedure. Twenty one (38.2%) were informed about the procedure by their doctors while 4 (7.3%) got information from friends and relatives and 4 (7.3%) from the internet. Level of education was associated with being informed (p=0.039) Multivariate logistic regression analysis revealed no significant predictor or EMG knowledge. Conclusion: Knowledge of EMG is poor and could be improved upon. More patient education needs to be done to prepare the patients, and allay their fears about the procedure.
Keywords
Disease outbreaks; Water quality; Epidemiology; Public health surveillance; Preventive medicine
Introduction
Electrodiagnostic (EDx) studies assist medical providers in treating peripheral nerves and neuromuscular disorders [1] and they are considered generally safe and well tolerated. Albeit, needle electromyography (EMG) being an invasive procedure, can sometimes be associated with iatrogenic complications such as bleeding, infection, nerve injury, pneumothorax, and local trauma. Similarly, certain precautions are required during nerve conduction studies (NCS) in patients with pacemakers and other similar cardiac devices; particularly, because of the risk of stray leakage currents. [2] Available literatures have highlighted the gaps in patient’s perception of the procedure especially with regards to pain. Patients perceive EMG as a painful examination even though the pain that may be encountered is not materially different from that of a venipuncture. [3] While studies have reported that patients perceive EMG (especially with concentric bipolar needle) to be more painful than NCS, [4,5] other authors have found the exact opposite. [6] It is speculated that patient’s expectation regarding the test may reflect generalized anxiety regarding testing procedures or misinformation regarding the nature of the test. [7] It is paramount therefore that patient should be informed and knowledgeable about the procedure as this may make the procedure more comfortable for them. [6]
The need for more accurate diagnosis and evidenced-based therapeutic measures for neurological disorders has driven the demand for neurological services in our environment. [8] Empirical evidence suggests that neuro-electrodiagnostic services are steadily becoming available and accessible in Nigeria. For example, there are at least three (3) additional EMG laboratories in southwestern Nigeria in the last 2 years; one of which is the EMG service being run by Monitor Healthcare Limited-Blossom Medical Centre (BMC) / World Federation of Neurorehabilitation (WFNR) center. Electromyography referrals have trickled in to this laboratory since its inception in April, 2014. Just like in other EDX practice outside Nigeria, we have observed that patients are often not informed about how EMG is performed or about its real utility. [9-11] We hypothesized that the knowledge of the patients referred for EMG in our center would equally be poor. We also hypothesized that a relationship would exist between the patient’s knowledge of EMG and their demographic characteristics as well as the source of referral. We therefore aimed at ascertaining the knowledge of EMG among patients undergoing this examination for the first time at the BMC/ WFNR Centre, Ibadan, Nigeria; considering the type, quality and source of the information they have. Our secondary aim was to look for associations between this information and the demographic characteristics of the patients as well as the types of referring physician.
Methodology
In this prospective, cross-sectional study, consecutive patients referred for EMG for the first time at the BMC/WFNR center, Ibadan, Nigeria from April 2014-December 2016 were interviewed. The interviews were before the commencement of the procedure after history taking. Verbal informed consent was obtained from the patients. Exclusion criteria included previous EMG (whether in our laboratory or elsewhere) and unwillingness to participate in the survey. Using a pre-designed questionnaire containing the patient’s bio-data (Appendix 1), we asked the patients whether they knew what EMG is, how and why EMG is performed and whether they think that it is a painful procedure. We also asked for the source of referrals. Following previous study, [9] a patient was considered “informed” if she/ he knew, at least, that the EMG is a test that uses an electric current or a needle, that it may be painful or cause discomfort, and that it is used to study the function of muscles and nerves. (Mondelli et al.)We also asked how the patient obtained his/her information: from referring physicians or in other ways (from friends or relatives or through websites, books, newspapers or magazines. This study complied with the 2013 update of the Declaration of Helsinki.
Data collection
The following data were entered into a spreadsheet: age, sex, level of education, occupation and type of referring physicians (neurologist, orthopaedics surgeon, /other specialist or general practitioners), patient knowledge of the manner of execution and purpose of EMG. All the patients gave their verbal informed consent to the study.
Statistical analysis
Descriptive statistics were expressed as mean values and standard deviation, frequencies and percentages. Differences, between “informed” and “not informed” patients, in demographic characteristics and type of referring physician were analyzed using ?2 tests. We also performed a multivariate logistic regression analysis calculating odds ratios and 95% confidence intervals to assess the strength of the associations between 2 dependent variables, evaluated separately (1-information on the manner of execution of EMG and 2-information on whether EMG is painful: incorrect/absent=0; present and correct=1), and a series of independent variables, namely age (age = 60=0; age> 60 years =1), gender (female=0, male=1), level of education (no formal education/primary-secondary education=0, tertiary/ postgraduate=1), currently employed (unemployed/student and retiree =0, civil servant, private workers, traders/business owners=1; type of referring physician (non-neurologist=0, neurologist=1). All statistical analyses were performed using SPSS version 20.0 (SPSS, Chicago, IL, USA). A p value < 0.05 was considered to be statistically signi?cant.
Results
Demography
Of the 59 patients examined during this period, 4 (6.8%) were not recruited because they were not first time examinee. Fiftyfive (55) subjects, consisting of 32 males and 23 females with mean age (SD) of 48.68 (18.32) and 43.30 (14.87) respectively were interviewed.
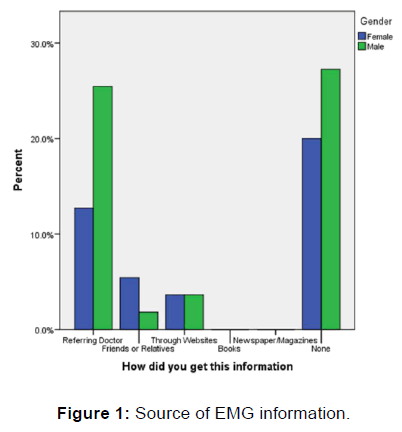
With regards to the nature and purpose of EMG, 23 (41.8%) were informed while the rest either had an incorrect information or had no information at all. Twenty (36.4%) patients had a correct knowledge on the execution of the EMG while 34 (61.2%) think that the procedure is painful. The source of information regarding the procedure was from the referring physician in 21 (38.2%) individuals, while 4 (7.3%) got information from the web/online materials and 4 (7.3%) from friends and relatives. Thirty nine (70.9%) of the referrals were from neurology specialists. Tables 1 and 2 show the participant’s demography and the types of referring physician in all the patients, and in the patients divided into “informed” and “not informed” groups, as well as the differences between the two groups. Higher level of education is significantly associated with being informed of the nature of the procedure (p=0.039) [Table 1] but not the execution of the procedure (p=0.349) [Table 2]. No other demographic variable is associated with being “informed” or “not informed”. Furthermore, significant proportion of those who were informed about the nature and execution of EMG were informed by the referring physician (p= 0.001). There was no gender difference with regards to the source of information on EMG. [Figure 1].
| Variables | All patients 55 (100%) |
Not Informed 32 (58.2%) |
Informed 23 (41.8%) |
Informed vs. Not informed |
|---|---|---|---|---|
| Age (years) | 46.44 ± 17.03 | 47.52 ± 17.78 | 45.23 ± 16.42 | t= 0.494, p=0.624 |
| Gender | ||||
| Male | 32 (58.2) | 18 (55.2) | 14 (60.9) | ?2 = 0.117, p=0.787 |
| Female | 23 (41.8) | 14 (48.3) | 9 (39.1) | |
| Level of Education | ||||
| None | 1 (1.8) | 1 (3.1) | 0 (0.0) | ?2 = 10.07, p=0.039* |
| Primary | 2 (3.6) | 2 (6.2) | 0 (0.0) | |
| Secondary | 14 (25.5) | 10 (31.2) | 4 (17.4) | |
| Tertiary | 30 (54.5) | 18 (56.2) | 12 (52.2) | |
| Postgraduate | 8 (14.5) | 1 (3.1) | 7 (30.4) | |
| Occupation | ||||
| Student | 10 (18.2) | 5 (15.6) | 5 (21.7) | ?2 = 1.549, p=0.907 |
| Civil Servant | 9 (16.4) | 5 (15.6) | 4 (17.4) | |
| Private | 16 (29.1) | 9 (28.1) | 7 (30.4) | |
| Business/Trading | 7 (12.7) | 5 (15.6) | 2 (8.7) | |
| Retired | 12 (21.8) | 7 (21.9) | 5 (21.7) | |
| Unemployed | 1 (1.8) | 1 (3.1) | 0 (0.0) | |
| Marital Status | ||||
| Not currently married | 17 (30.9) | 10 (31.2) | 7 (30.4) | ?2 = 0.004, p=0.949 |
| Currently married | 38 (69.1) | 22 (68.8) | 16 (69.6) | |
| Source of Referral | ||||
| Neurologist | 39 (70.9) | 22 (68.8) | 17 (73.9) | ?2 = 1.200, p=0.549 |
| Orthopaedics | 8 (14.5) | 4 (12.5) | 4 (17.4) | |
| Other specialist | 8 (14.5) | 6 (18.8) | 2 (8.7) | |
| How did you get the information | ||||
| Referring Doctor | 21 (38.2) | 6 (18.8) | 15 (65.2) | ?2 = 37.38, p=0.001 |
| Friends and Relatives | 4 (7.3) | 0 (0.0) | 4 (17.4) | |
| Websites | 4 (7.3) | 0 (0.0) | 4 (17.4 | |
| None | 26 (47.3) | 26 (81.2) | 0 (0.0) |
Table 1: Data in the whole sample and in the patients who were “informed” and “not informed” about the nature of the EMG procedure
| Variables | All patients 55 (100%) |
Not Informed 35 (47.3%) |
Informed 20 (52.7%) |
Informed vs. Not informed |
|---|---|---|---|---|
| Age (years) | 46.44 ± 17.03 | 46.77 ± 17.83 | 45.85 ± 15.98 | t= -0.191, p=0.849 |
| Gender | ||||
| Male | 32 (58.2) | 16 (45.7) | 7 (35.0) | ?2 = 0.600, p=0.438 |
| Female | 23 (41.8) | 19 (54.3) | 13 (65.0) | |
| Level of Education | ||||
| None | 1 (1.8) | 1 (2.9) | 0 (0.0) | ?2 = 4.44, p=0.349 |
| Primary | 2 (3.6) | 2 (5.7) | 0 (0.0) | |
| Secondary | 14 (25.5) | 10 (28.6) | 4 (20.0) | |
| Tertiary | 30 (54.5) | 19 (54.3) | 11 (55.0) | |
| Postgraduate | 8 (14.5) | 3 (8.6) | 5 (25.0) | |
| Occupation | ||||
| Student | 10 (18.2) | 6 (17.1) | 4 (20.0) | ?2 = 1.12, p=0.952 |
| Civil Servant | 9 (16.4) | 5 (14.3) | 4 (20.0) | |
| Private | 16 (29.1) | 10 (28.6) | 6 (30.0) | |
| Business/Trading | 7 (12.7) | 5 (14.3) | 2 (10.0) | |
| Retired | 12 (21.8) | 8 (22.9) | 4 (20,0) | |
| Unemployed | 1 (1.8) | 1 (2.9) | 0 (0.0) | |
| Marital Status | ||||
| Not currently married | 17 (30.9) | 11 (31.4) | 6 (30.0) | ?2 = 0.01, p=0.912 |
| Currently married | 38 (69.1) | 24 (68.6) | 14 (70.0) | |
| Source of Referral | ||||
| Neurologist | 39 (70.9) | 22 (62.9) | 17 (85.0) | ?2 = 3.29, p=0.193 |
| Orthopaedics | 8 (14.5) | 6 (17.1) | 2 (10.0) | |
| Other specialist | 8 (14.5) | 7 (20.0) | 1 (5.0) | |
| Do you think it is Painful | ?2=50.88 , p= <0.001 | |||
| Yes | 21 (38.2) | 1 (2.9) | 20 (100) | |
| No/I don’t know | 34 (61.8) | 34 (97.1) | 0 (0.0) |
Table 2: Data in the whole sample and in the patients who were “informed” and “not informed” about the execution of EMG.
Multivariate binary logistic regression analysis shows that being informed of the nature of EMG is not predicted by any demographic variable. In fact, the association with level of education that was noted on univariate analysis was washed off in the simultaneous context of other variables in the model [Table 3]. No variable is also predictive of the perception that EMG is painful [Table 4].
| Independent Variables | B | OR | SE | P value | 95% CI |
|---|---|---|---|---|---|
| Age (>60 years) | 0.184 | 0.065 | 0.725 | 0.799 | 0.29-4.99 |
| Gender (Male) | -0.295 | 0.24 | 0.604 | 0.625 | 0.23-2.43 |
| Level of Education (High) | -1.242 | 3.397 | 0.674 | 0.065 | 0.08-1.08 |
| Occupation (currently employed) | 0.427 | 0.437 | 0.646 | 0.509 | 0.43-5.44 |
| Source of Referral (Neurologist) | -0.323 | 0.256 | 0.639 | 0.613 | 0.21-2.53 |
Table 3: Multivariate logistic regression analysis with correct information on the nature of the EMG procedure as the dependent variable.
| Independent Variables | B | OR | SE | P-value | 95% CI |
|---|---|---|---|---|---|
| Age (>60 years) | 0.435 | 0.335 | 0.751 | 0.563 | 0.35-6.73 |
| Gender (Male) | -0.433 | 0.486 | 0.621 | 0.486 | 0.19-2.19 |
| Level of Education (High) | -1.038 | 2.287 | 0.686 | 0.13 | 0.09-1.36 |
| Occupation (Currently employed) | 0.512 | 0.6 | 0.661 | 0.438 | 0.46-6.09 |
| Source of Referral (Neurologist) | -0.938 | 1.854 | 0.689 | 0.173 | 0.10-1.51 |
Table 4: Multivariate logistic regression analysis with perception that “EMG procedure is painful” as the dependent variable.
Discussion
EDx services are still scarce in sub-Saharan African settings hence, there is paucity of data driven information regarding the practice, its availability and patient’s perception of its utility. Our findings indicate that less than half of patients undergoing EMG in our center are knowledgeable about the procedure before being examined. More than half of the patients were either incorrectly informed or had no information at all. This finding mirrors that of Mondelli et al. where less than half of the patients were knowledgeable about the EMG procedure even though that study was larger, and conducted in a tertiary EMG laboratory in a cosmopolitan setting. In addition to level of education, Mondelli et al. found that referral by a specialist as well as provision of a referral diagnosis were associated with being correctly informed about EMG. In this study however, we found no association between the type of referring physician and possession of correct information about EMG. The level of education was the only significant factor that was associated with being informed.
Generally, higher level of education has been associated with health knowledge and behaviors, employment status, insurance status, and a range of other psychosocial factors. With regards to health information seeking behaviors, patients with higher educational attainment tend to have higher health literacy levels, which enable them to better access, understand, and communicate actionable health information. [12,13] It is not clear from this study whether the more educated patients requested for EMG information from the physician or it was volunteered by the physicians unsolicited since we did not ask for this information. We also noticed that less than half of those referred by neurologist were correctly informed about the nature and execution of EMG. While we do not have a ready explanation for this outlook, we cannot completely rule out issues with recall of information on the part of the patients.
Twenty one (38%) patients, most of whom were less than 60 years of age, got the information on EMG from the referring physician while 7% got it from friends/relatives and another 7% got the information from websites. All the patients who got information from websites and from friends/relatives were correctly informed. In contrast to our findings, more than two-third of the cohort who accessed the internet for EMG information in the study by Mondelli et al. [14] were not correctly informed. Our study therefore iterates the fact that online sources, or information from first hand sources maybe correct; although in certain instances, they have the tendency to under-inform, or misinform the public since some of the websites are created by non-doctors for commercial purposes and this cuts across many medical topics. [14] Although health care providers, pharmacists, friends and relatives, retirement community staff, newspapers, the Internet, television, and the radio still remain trusted (in that order, highest to lowest) sources of health information, it has been found that older adults, have a greater amount of trust in a person with whom they are able to actively discuss their health as opposed to a nonliving source, which they have to access or manipulate, such as the Internet. [15]
Less than half of our patients feel that EMG is a painful procedure while others did not know what to expect. The perception that the procedure is painful is not associated with any demographic variables. Although the pain and discomfort due to NCS/EMG is a minor one, the American Association of Electrodiagnostic Medicine (AAEM), has advised physicians to make every effort to ensure that patients are adequately prepared for planned EDx procedures and that they are made as comfortable as possible during the examination. Additionally, physicians should be attentive to signs of patient discomfort and safety concerns and resolve them before proceeding. In fact, the physicians may decide whether to admit family members or significant others into the examination room during testing to provide support. [16] All our patients were counseled and prepared about what to expect from the procedure after we have assessed their background knowledge. In some instances, there were significant others to provide support during the procedure.
This is a single center, small sampled study; hence, the findings cannot be generalized to the population of patients undergoing EDx evaluation in Nigeria. The findings from this pilot survey however, can provide a basis for drawing up locally relevant protocols, especially with regards to patient’s information and preparation when requesting for EDx procedure.
Conclusion
The level and quality of EMG knowledge among the patients is poor. The referring physician can bridge this gap by engaging in more patient education. This will prepare the patients and assuage their fears about the procedure.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Bergquist ER, Hammert WC. Timing and appropriate use of electrodiagnostic studies. Hand Clinics, 2013; 29: 363-370.
- Al-Shekhlee A, Shapiro BE, Preston DC. Iatrogenic complications and risks of nerve conduction studies and needle electromyography. Muscle & Nerve, 2003; 27: 517-526.
- Alshaikh NM, Martinez JP, Pitt MC. Perception of pain during electromyography in children: A prospective study. Muscle & Nerve, 2016; 54: 422-426.
- Wee AS, Boyne RL, Abernathy SD, Nick TG. Pain perception to nerve conduction and needle electromyographic procedures. Journal of the Mississippi State Medical Association, 2004; 45: 327-323.
- Richardson JK, Evans JE, Warner JH. Information effect on the perception of pain during electromyography. Archives of Physical Medicine and Rehabilitation, 1994; 75: 671-675.
- Jerath NU, Strader SB, Reddy CG, Swenson A, Kimura J, Aul E. Factors influencing aversion to specific electrodiagnostic studies. Brain and Behavior, 2014; 4: 698-702.
- Jan MM, Schwartz M, Benstead TJ. EMG related anxiety and pain: A prospective study. The Canadian journal of neurological sciences. Le journal canadien des sciences neurologiques, 1999; 26: 294-297.
- Philip AB, Akolade I, Ahmed W, Abayomi OS. Pattern and influence of in-patient neurological consultations in a Nigerian Tertiary Health Institution: A brief survey. ISSN, 2012; 1: 2277-2879.
- Mondelli M, Aretini A, Greco G. Knowledge of electromyography (EMG) in patients undergoing EMG examinations. Functional Neurology, 2014; 29: 195-200.
- Podnar S. Critical reappraisal of referrals to electromyography and nerve conduction studies. European Journal of Neurology, 2005; 12: 150-155.
- Cocito D, Tavella A, Ciaramitaro P, Costa P, Poglio F, Paolasso I, et al. A further critical evaluation of requests for electrodiagnostic examinations. Neurological Sciences, 2006; 26: 419-422.
- Feinberg I, Frijters J, Johnson-Lawrence V, Greenberg D, Nightingale E, Moodie C. Examining Associations between Health Information Seeking Behavior and Adult Education Status in the U.S.: An Analysis of the 2012 PIAAC Data. PloS One, 2016; 11: e0148751.
- Bennett JA, Cameron LD, Whitehead LC, Porter D. Differences between older and younger cancer survivors in seeking cancer information and using complementary/alternative medicine. Journal of General Internal Medicine, 2009; 24: 1089-1094.
- Beredjiklian PK, Bozentka DJ, Steinberg DR, Bernstein J. Evaluating the source and content of orthopaedic information on the Internet. The case of carpal tunnel syndrome. The Journal of Bone and Joint Surgery. American Volume, 2000; 82: 1540-1543.
- Chaudhuri S, Le T, White C, Thompson H, Demiris G. Examining health information-seeking behaviors of older adults. Computers, Informatics, Nursing?: CIN, 2013; 31: 547-553.
- Leonard Jr JA, Abel N, Cochrane T, Denys E, Musick DW, Simpson D, et al. Guidelines for ethical behavior relating to clinical practice issues in neuromuscular and electrodiagnostic medicine. Muscle & Nerve, 2015; 52: 1122-1129.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.