Learning from Health Care Workers’ Opinions for Improving Quality of neonatal Health Care in Kilimanjaro region, northeast Tanzania
- *Corresponding Author:
- Dr. Bernard Mbwele, Kilimanjaro
Clinical Research Institute, Kilimanjaro Christian Medical Center, P.O. Box 2236, KCMC, Moshi, Tanzania.
E-mail: benmbwele@gmail.com
Abstract
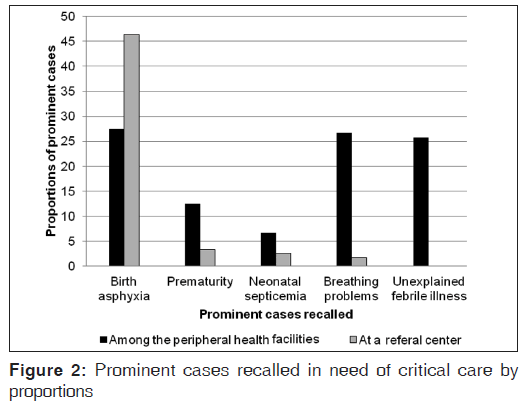
Background: There is a higher neonatal mortality rate while the adherence to the existing guidelines is rarely studied in Tanzania. Aim: The aim of this study is to assess the performance of health workers for neonatal health‑care. Materials and Methods: Settings ‑ Peripheral health facilities (regional referral, district hospitals and health centers) and a tertiary referral hospital of Kilimanjaro region, Tanzania. Fourteen hospital facilities within all seven districts of the Kilimanjaro region wer involved in this cross‑sectional descriptive study. Data were collected for 5 months from 26th November, 2010 to 25th April, 2011. We analyzed our quantitative data by using STATA v10 (StataCorp, TX, USA) for statistical comparison using Chi‑square test to test the difference between the categories and odds ratio (OR) for association between independent and dependent variables. Results: Birth asphyxia was the most recalled health problem requiring critical care, reported by 27.5% (33/120) of health‑care workers (HCWs) at peripheral hospitals and at 46.4% (13/28) in a tertiary referral centers. Majority of HCWs commented on their own performance 47.5% (67/140). In the periphery (40), first comment was on management and follow‑up of neonatal cases 47.5% (19/40), second on a need of skills 45% (18/40) and third on timely referrals 7.5% (18/40). Shortage of proper equipment was reported at 26.4% (37/140), shortage of staff was reported at 12.0% (17/140), lack of organization of care 11.4% (16/140) and poor hygiene at 2.9% (4/140). It was hard to judge the impact of training on the sufficiency of knowledge (OR: 2.1; 95% confidence interval: [0.9 ‑ 4.8]; P = 0.08) although levels of knowledge for critical neonatal care were higher at the tertiary referral hospital (Pearson χ2 [2] = 53.8; P < 0.001). Conclusion: Performance of HCWs in early neonatal care is suboptimal and requires frequent systematic evaluation.
Keywords
Health care workers, Kilimanjaro, Knowledge, Neonatal, Northern Tanzania, Performance, Peripheral hospitals, Quality of care
Introduction
World-wide, neonatal deaths account for four-tenth of under five deaths and play a barrier for the achievement of the Millennium Development Goal number 4.[1,2] A large proportion of these deaths are from sub-Saharan Africa.[3-5] Most of the causes of these deaths are preventable through appropriate health-care workers’ (HCWs) interventions.[6,7]
Distance, cost of health-care and performance of HCWs are the contributing barriers.[8,9] However, facility-based births are increasing in many resources limited countries and therefore a call for improving the performance of HCW at these hospital settings is vital.[10-14]
Tanzania is a sub-Saharan African country with an infant mortality rate of 65.74 deaths/1000 live births and a neonatal mortality rate of 26 deaths/1000 live births in 2012.[15] From 2000 to 2010 perinatal mortality at a tertiary referral hospital in the Kilimanjaro region was 57.7/1000 (1958 out of 33,929), of which 1219 (35.9/1000) were stillbirths and 739 (21.8/1000) were early neonatal deaths.[16] Neonatal deaths remain higher in rural settings compared with urban settings.[17-19] Several studies have demonstrated poor adherence to existing guidelines[20-22] as a cause for a large proportion of neonatal deaths and training focused on maternal-child health has been shown to result in improvement.[23] However, monitoring and maintenance of training remain suboptimal[22,24,25] in terms of adherence to guidelines[26] and other service-related factors.[22,27,28]
There are growing concerns regarding the performance of rural HCWs in Tanzania.[20] Further evidence shows that there are challenges related to lack of motivation and evidence based guidelines.[18,20] Qualitative approaches have rarely been made to synthesize and describe the neonatal care in Kilimanjaro region. HCW, offers the central part of the quality of neonatal health-care in Tanzania.[29] The aim of this study was to assess the performance of HCW in providing neonatal health-care in the hospitals Kilimanjaro, Tanzania.
Materials and Methods
Study design, setting, purpose and ethics
The overall research design was a cross-sectional study using qualitative and quantitative approaches for the assessment of the performance of HCWs in 14 hospital facilities within all seven districts of the Kilimanjaro region.
The study was approved by the Kilimanjaro Christian Medical University Ethical Committee and written approval for data collection was also received from the Kilimanjaro Regional Medical Officer that interviews and pictures might be taken and results published. Before conducting interviews for health workers, written consents were obtained from all HCWs approached for discussions.
Data were collected for 5 months from 26th November, 2010 to 25th April, 2011 in all districts of the Kilimanjaro region. From 15th to 19th November 2010, questionnaires were tested for validity and reliability at the regional hospital as a pilot. A revised questionnaire approved by the supervisor was developed through paraphrasing the questions with qualitative checks. All interviewers were trained in a structured system so as to standardize their interpretation of management and minimizing information bias such as interview bias and reporting bias.
Hospital and health workers selection
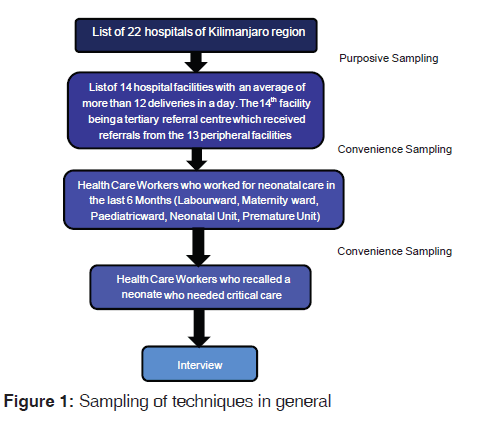
By a purposive sampling method, all facilities have an average of more than 12 deliveries in a day and allowed to refer sick neonates to the tertiary referral hospital in the region.
Within each selected hospital, HCWs who had neonatal care responsibilities in the past 6 months (main criterion) were selected by convenience sampling. They were then asked to recall a sick neonate needed critical care in past 6 months (second criterion) before approached for a possible interview [Figure 1] recalling neonatal deaths in the last 12 month was additional. Visits to hospitals were unannounced.
Data collection
Hospitals were visited without prior notification and all HCW with the criteria to be interviewed were contacted. After consenting in written permission, HCWs were interviewed individually in English. HCW were then asked if they had received any training related to neonatal health-care.
First, HCWs were asked to rate their own level of knowledge. Second, through indirect assessment, HCWs were inquired to recall one neonate who needed critical care. Interviews that allowed in-depth description were used to probe their management on reaching the diagnosis, investigations used and treatments. Then HCW were asked to state what went well, what went wrong and what she/he would wish to do. When the explanations were ambiguous, the embedded guide of in-depth interview was used to catch the responses in details. Detailed discussions were written in the notebooks while the digital recorders were left on recording the discussions. The narratives were then entered in a Microsoft Access 2007 database.
Data analysis
We analyzed our quantitative data by using STATA v10 (StataCorp, TX, USA) for statistical comparison using Chi-square test to test the difference between the categories and odds ratio (OR) for association between independent and dependent variables. Microsoft Excel 2007 software was used for graphical presentations from the STATA results.
The taped interviews were transcribed verbatim. Qualitative variables from the narratives were coded into different themes using colors and the themes were counted so as to generate the final picture of the discussions. Narrative given by health workers are labeled by academic qualifications, age and the facility they are from.
A pre-prepared consensus list (World Health Organization [WHO] emergency triage assessment and treatment (ETAT) Manual and Kilimanjaro Christian Medical Center Pediatric management manual) for the management of anticipated conditions, including birth asphyxia, extreme prematurity, meconium aspiration, general respiratory distress, congenital cardiac disease, complex congenital malformations. This was compiled with the additional guide for triaging sick neonates who needs critical care based on the WHO-ETAT manual for justifying mistakes. The mistakes were counted on justifying diagnosis from complaints mentioned, what investigations were necessary and what medications were required. The numbers of mistakes were used to estimate the level of knowledge. One wrong answer on a clinical problem or no wrong answer was taken as satisfactory; two wrong answers of any type were moderate and three or more wrong answers were considered as a low level of knowledge.
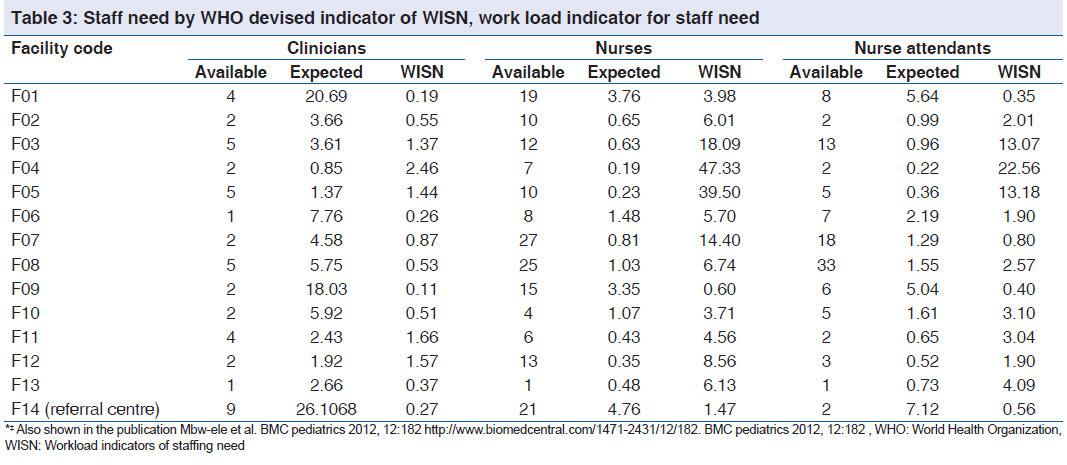
A head count of actual staff present during the visits were recorded from the health management information system or Mfumo wa Taarifa za Uendeshaji Huduma za Afya booklets and duty roasters for work shifts. We calculated the WHO devised workload indicator for staffing need (WISN)[30,31] by using the WHO Manual for Implementation[32] for duties of each cadre of health workers in the district hospitals. The WHO’s Workforce/WISN method is used to calculate and estimate the number of health workers required to achieve the neonatal health “service guarantees”. We measured the ratio between current staffing levels and the ideal expected number. We calculated the expected numbers of health workers by using the amount of hours available for work in a year per one health worker compared with the total duration of time in hours in 1 year required to serve hospital based on neonates available. The WISN ratio was given by the number of health workers available divided by the number of health workers expected.
Quantitative results
A total of 148 HCWs responsible for providing neonatal care were interviewed; nearly 81.1% (120/148) were from peripheral hospitals (2 health centers, 10 District Hospital and 1 Regional Hospital) and 18.9% (28/148) were from the northern zone referral hospital in the Kilimanjaro region. In general, 4.1% of all HCWs (6/148) were unable to recall a sick neonate and as such their data were not assessed, leaving 142 who recalled treating or attending to a sick neonate for further interviews and analysis. The HCW’s demographic information for the difference between the peripheral hospitals and tertiary referral center with the levels of significance are shown in Table 1.
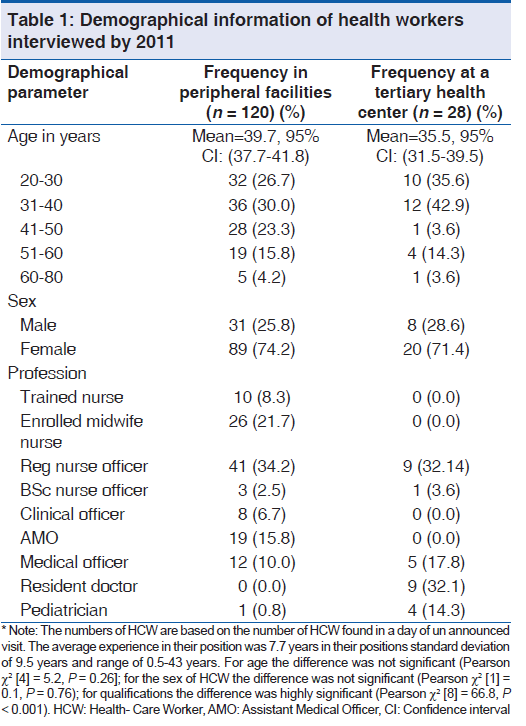
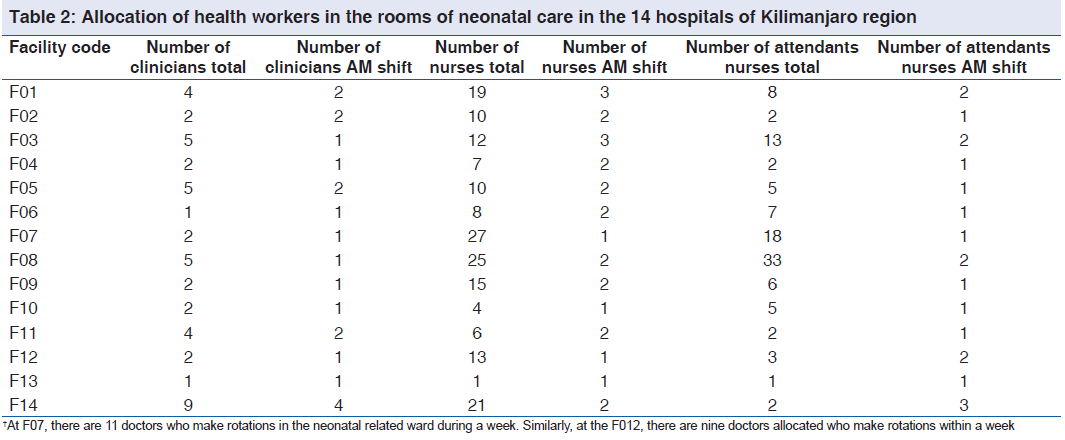
The staffing levels by shifts are shown in Table 2 and the respective WISN levels are shown in Table 3 for the implication of work load indication. Common diagnoses of neonates as recalled by HCW are shown in Table 4.
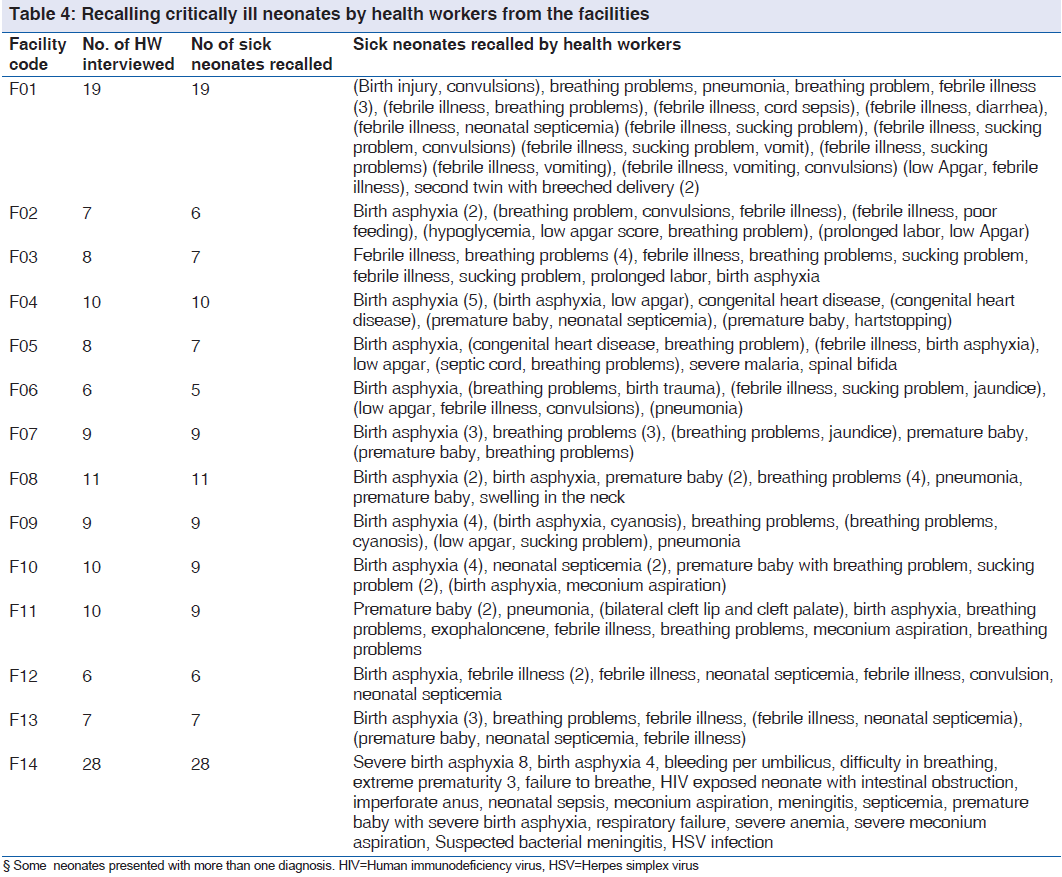
At the referral hospital, half of the referred cases are presented with a complicated picture of the illness as shown in Figure 2 and Table 4. More than half of the complicated conditions in the periphery were referred to the tertiary level.
One-third of HCWs, 34.1% (41/120) from the periphery and two-thirds of HCW 60.7% (17/28) from the tertiary referral center received various training for Neonatal care recommended by the Ministry of health (Pearson χ2 [1] = 6.7; P = 0.01). Half of the HCWs who received various training in neonatal care were trained in 1 week or less.
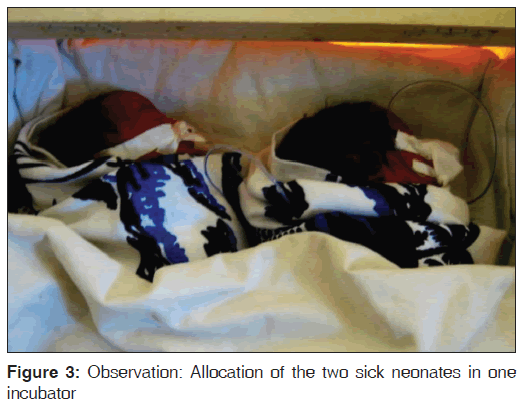
Among 70 HCWs who reported the presence of incubators in their facilities, only 21.4% (15/70) had training on proper uses of incubators while the remaining 78.6% (55/70) did not (Figure 3 showing two neonates in one incubator by our observation).
When asked to self-grade on the level of skills required, 44.7% HCWs in peripheral hospitals (51/114) declared competency compared to 82.1% HCWs at the tertiary referral center (23/28) (Pearson χ2 [2] = 12.1; P < 0.01).
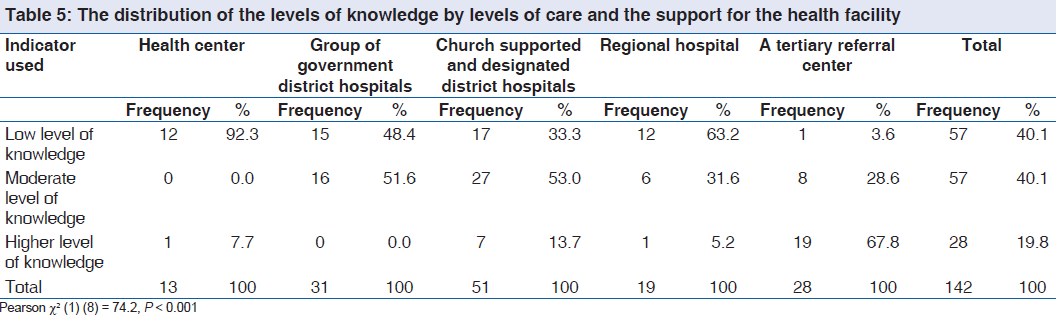
By counting mistakes, highest level of knowledge (0-1 mistakes) was found in 7.7% of HCW at the health centers (1/13), 0% in a group of government district hospitals (0/31), 13.7% church based and church based designated district hospitals (7/51), 5.3% at a regional hospital (1/19%) and 67.9% at a tertiary referral center (19/28) (Pearson χ2 [6] = 74.2; P < 0.001). i.e., Highest levels of knowledge for critical neonatal care were at 7.9% (9/114) in the periphery and 67.9% (19/28) at the tertiary referral hospital (Pearson χ2 [2] = 53.8; P < 0.001). The distribution moderate and lowest levels of knowledge of HCW are shown in Table 5.
On assessing the impact of training, 53.7% (15/56) had higher levels of knowledge compared to 46.4% (13/86) who did not receive training and 28.1% (15/56) had the lowest level of knowledge among trained compared to 71.9% (41/86) with the lowest level of knowledge among nontrained (Pearson χ2 [2] = 5.9; P = 0.05). Further studying of the impact of training on insufficiency of knowledge (lowest and moderate levels) and sufficiency of knowledge (highest level) showed the association was insignificant (Pearson χ2 [1] = 0.1; [OR: 2.1; 95% confidence interval: 0.9-4.8]; P = 0.08).
Quality of records
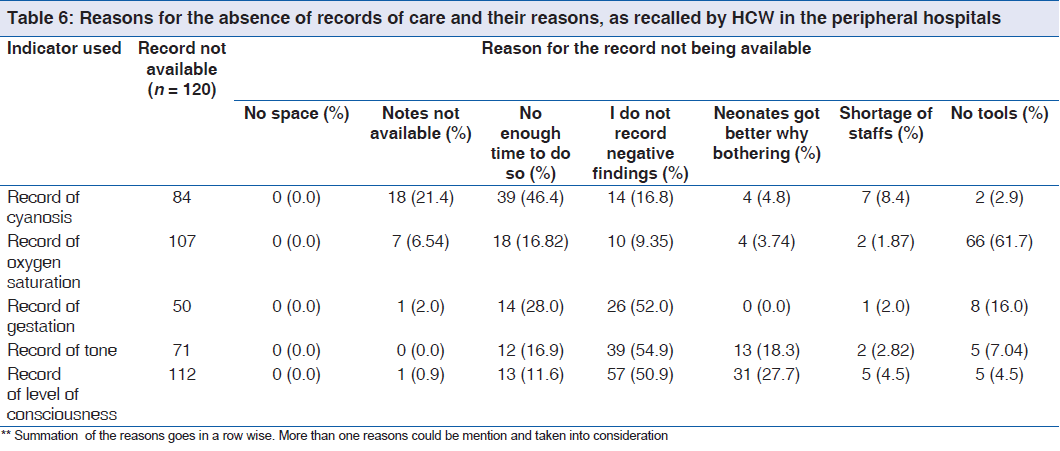
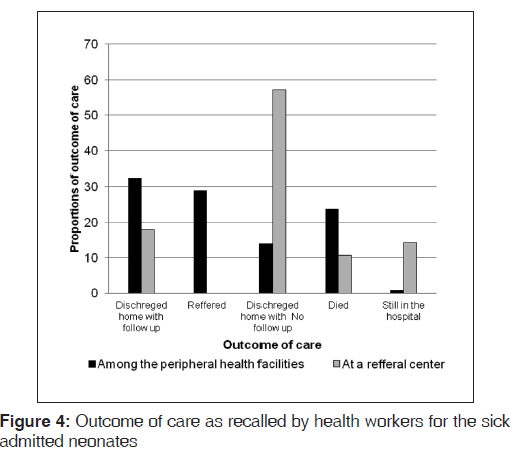
The invariable reasons for the absence of records are shown in Table 6 for the peripheral facilities. Outcome of care in both settings is shown in Figure 4.
Qualitative results
What could have been done better? (Qualitative findings)
There were 173 opinions of health workers gathered, 140 of which were from the peripheral hospitals. The leading opinion from the periphery was on performance of health workers themselves 28.6%, (40/140). Where three themes were found on performance, first on appropriate management, monitoring and follow-up of neonatal cases 47.5%, (19/40). For example, Assistant Medical Officer (AMO) F3, 46 years old HCW, has seen a need to “monitor the baby, do faster reporting and make special follow-up care for neonates, especially those who have been resuscitated, will really improve the outcome of these babies.”
Second theme was on a need of skills 45%, (18/40). Nurse Officer (NO) F4, 55 years old explained that, “I think training of health workers on follow-up of neonatal care is necessary because resuscitation has remained to be challenging and difficult.”
Third theme was on the theme was on lack of timely referrals to the regional or referral hospitals 7.5% (18/40). Enrolled midwife nurse F7, 38-year-old observed while considering a specific case, “We should have referred the baby; the condition was very bad, and we did not have anything to do here that could help the baby.”
At the zonal referral hospital, the performance of health workers was reported at 39.4% (13/33). NO F14, 25 years old recalled a baby with Birth asphyxia and she explained that “Birth asphyxia is the main problem here. If labor and delivery were appropriately monitored, there would be less cases of birth asphyxia.”
In general there was a 26.4% shortage of proper equipment at the periphery centers (37/140). AMO F11, 36-year-old who recalled a baby with febrile illness and breathing problems explained, “If we could have a ventilation machine and pulse oximeter we could serve many babies here.” Drug supplies was complained at 7.9% (11/140) and 1 comment from the referral hospital) reported fluctuations of drug supply in the facility.
Shortage of staff was reported at 12.0% (17/140). For example, NO F9, 28 years old, complained “we needed more skilled staff to treat the critically ill baby, again not only skills nut number of doctors here is not satisfying, one doctor and one nurse is not enough. We miss some techniques and team work here.”
Inappropriate organization of care in the peripheral facilities was reported by 11.4% (16/140) (all from the periphery, none from the zonal referral hospital). MO F12, 47 years old HCW, told the interviewers that “if we had a neonatal unit, we could do more monitoring and more supportive neonatal care. I think we have some tools to start with, but we only miss the arrangement.”
The concern of proper hygiene was reported at 2.9% (4/140) all from the periphery, none from the tertiary referral hospital.
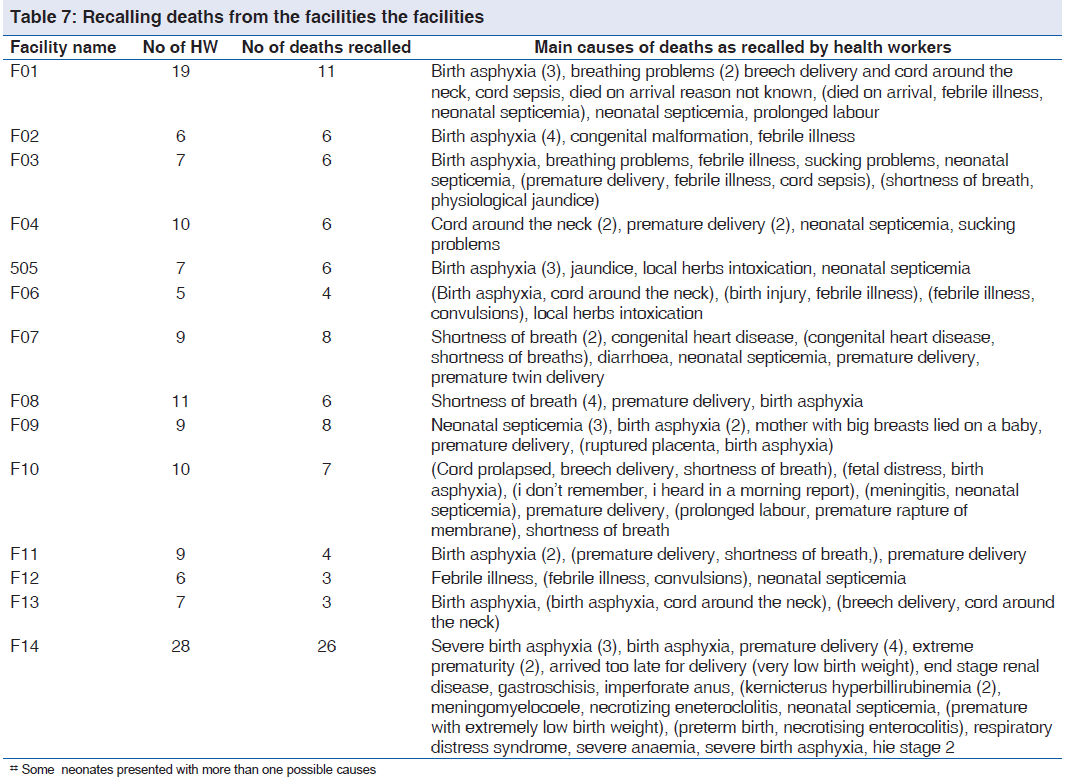
Neonatal deaths recalled
There were 68.4% HCW (78/114) from peripheral hospitals and 92.9% HCW (26/28) at the tertiary referral hospital who recalled deaths in their facility [Table 7]. Among HCWs who recalled cases of neonatal deaths, 60.6% (63/104) were at the District hospitals and Health Centers, 8.6% (9/104) at the Regional hospital and 16.3% HCWs at the tertiary referral hospital (17/104) reported that these deaths could have been avoided.
What could be done to avert neonatal deaths? (Qualitative findings)
We had 81 opinions on avoiding deaths from the 78 HCWs in the periphery. From these, 43.2% (35/81), reflected a concern regarding the quality of skills required during birth. NO F1, 28 years old HCW recalled a case fatality involving a breeched delivery in the night shift with the umbilical cord around the neck. The worker commented, “the diagnosis of the breech was known before delivery, but cesarean-section was not performed. We had a difficult time resuscitating the baby.”
From the periphery 23.5% (19/81), of HCWs complained on the lack of mother’s education and delay of care. NO F4, 47 years old HCW explained the need to “educate the mothers not to take herbs and to come to the hospital with any signs of a problem.”
A lack of equipment was mentioned by 13.6% of HCW’s (11/81) among peripheral hospitals. From the tertiary referral hospital, 36.8% (7/19) reported a lack of sufficient equipment. Resident Master of Medicine in Pediatrics F14 37 years old HCW recalled a fatality involving Kernicterus and Bilirubin cephalopathy. She emphasized, “we needed systematic blood transfusions, logistics, more tools, and phototherapy, as in many occasions babies need to share tools here. Lastly I would like to comment on exchange blood transfusion as an important way to save this baby.”
Discussions
The Kilimanjaro region is generally characterised by the suboptimal performance of health workers in critical neonatal care from peripheral facilities. The main reasons are low levels of knowledge that affect management, monitoring, follow-up skills and referral and staffing levels can affect documentation and evaluation process. Although the tendency to refer neonates to tertiary centers is high, a majority of neonates die in the process of referral or immediately after a referral to a tertiary center.[29]
Our qualitative findings from the perceptions of HCW could explain our quantitative findings and some global findings in neonatal deaths[1,33] that were justified by large surveys from Tanzania[34] on health workers’ performance attributes.[16]
The HCW felt there is a huge gap between skills available and skills required for neonatal health- care. This is shown in our qualitative finding that there were unnecessary referrals from the periphery. Furthermore, most of the diagnoses found quantitatively were manageable in the periphery. These challenges can that can be solved by building the capacity of HCWs qualified at the levels certificates and diplomas peripheral facilities.
Qualitatively, HCW showed supplies of equipment and drugs are crucial barriers of the performance, but not the core of the problem as reported previously.[23] Review of diagnoses dealt, triaging and monitoring came first to be reported and then followed by supplies of equipment and drugs as it can be shown in rapid assessments.[29]
Poor organization of care and poor hygiene (least commented) is found to be in line with the high workload in a provision of acceptable quality care areas as previously reported.[31] We could find that frequent WISN calculations will be useful in estimating staffing need in neonatal care[30-32] and staff recruitment. In this case, our study reflects the need for intervening the staff levels required in night shift.
The lack of updated science based guidelines on health-care, staffs supports and mothers awareness and involvement[35] are the constraints constraint for evidence based practice in developing countries.[36] Our study emphasises the need for the development of the standards for staff duties by cadres, level of education and motivation of HCW.[29]
Apart from the Ministry of health recommended training, on job facility based designed practical trainings are not normally practiced in the facilities. These findings are similar in both rural Asia and southern America.[6,37] However, the responsible governments in sub-Saharan Africa including Tanzania delay in setting strategies to educate the health workers.[20,38]
Our quantitative findings in knowledge assessment gave borderline 95% significance level of association between the previous trainings on neonatal resuscitation, integrated management of childhood illnesses, and the use of kangaroo methods and the three levels of knowledge, reflect a need of training.[25,39] However, a detailed study through the OR assessment showed an opposite finding with a confusing theme. This might be caused by the recall bias and type a case recalled during the interview and the lack of specific training assessment. There is an evidence that neonatal care in the 24 hours of life needs to be evaluated and promoted[36] with the practical trainings.[40,41] Furthermore, motivation and aftertraining performance evaluations need to be set into routine practice.[12,42] Other stake holders of health-care services[43] can assist the exercise especially where there is a challenge of finance[44] and supplies.[38] Reputable and recognized academic institutions may play a role in motivation[12] toward improving HCW performance.
Study limitations and strengths
Our study design used one interviewer to one HCW and could not solve all issues of systemic error like interobservers variation. Recalling the sick neonates exposed the data to recall bias. Information based on one case for assessing the knowledge affected our findings and conclusions. The study design was cross-sectional with a limited sample size; hence, it failed to generate temporal relationships between training and knowledge and then quality-of-care and outcome.
It was hard to draw a line between the knowledge to be assessed and knowledge required for giving comments for the quality improvements. However, to avoid a Hawthorn Effect (observation bias), visits were made in a short period to all facilities at once without prior information.
The strength of this study comes from gathering a combination of data collection techniques at the different levels of health-care.[45]
Conclusion
Performance of HCWs in early neonatal care is suboptimal in the management, monitoring and follow-up. Frequent evaluation in the peripheral facilities is Important.
Recommendations
Guided Practical Specific neonatal health-care trainings among HCWs educated at diploma level are required. The use of training of trainer expansion and “on job after-training monitoring system” is required in Tanzania. Clinical trial and systematic reviews of the impact of training in neonatal care are needed.
Acknowledgments
We acknowledge the Ministry of health and social welfare, the government of Tanzania for funding the study for MSC Training and then to the family of Mr. Asumwisye Mbwele for additional funding of this study. We appreciate for technical assistance in neonatology given by Professor Raimos Olomi (KCMC) and Elizabeth Reddy (Duke University-KCMC Collaboration). Special acknowledgment is directed to Prof. Bernard C. J. Hammel from Radboud University/KCMUCo, for the technical support. We further acknowledge the support from volunteers, Laurens Maarten Moeliker, Robert Gerard Leicher from Netharlands, Anne Eckleof from Stockholm Sweden for volunteering in data collection and entry, Patric Toalson, Sung Bo Yung, Tamara Russel, Lauara Thorpe, Elke Wasdovich from Lilly pharmaceutical company and Ibptisam Shaabal from Malysia for volunteering in data collection and data entry. Again appreciation for edits of the database by medical students of KCMUCo shall go to Johari Katanga, Daniel Joseph, Said Msuya, Kelvin Msuya, Godwin Msuya and Flavian Alutu Masokoto from Uru Mawela Parish of Moshi, Tanzania for extensive support in translations where needed.
Source of Support
Ministry of Health funding for MSc Clinical Research.
Conflict of Interest
None declared.
References
- Lozano R, Wang H, Foreman KJ, Rajaratnam JK, Naghavi M, Marcus JR, et al. Progress towards Millennium Development Goals 4 and 5 on maternal and child mortality: An updated systematic analysis. Lancet 2011;378:1139-65.
- Bahl R, Martines J, Bhandari N, Biloglav Z, Edmond K, Iyengar S, et al. Setting research priorities to reduce global mortality from preterm birth and low birth weight by 2015. J Glob Health 2012;2:10403.
- Lawn JE, Cousens S, Bhutta ZA, Darmstadt GL, Martines J, Paul V, et al. Why are 4 million newborn babies dying each year? Lancet 2004;364:399-401.
- Lawn JE, Kinney MV, Black RE, Pitt C, Cousens S, Kerber K, et al. Newborn survival: A multi-country analysis of a decadeof change. Health Policy Plan 2012;27 Suppl 3:iii6-28.
- Lam JO, Amsalu R, Kerber K, Lawn JE, Tomczyk B, Cornier N, et al. Neonatal survival interventions in humanitarian emergencies: A survey of current practices and programs. Confl Health 2012;6:2.
- Ariff S, Soofi SB, Sadiq K, Feroze AB, Khan S, Jafarey SN, et al. Evaluation of health workforce competence in maternaland neonatal issues in public health sector of Pakistan: An Assessment of their training needs. BMC Health Serv Res 2010;10:319.
- Duysburgh E, Zhang WH, Ye M, Williams A, Massawe S, Sié A, et al. Quality of antenatal and childbirth care in selected rural health facilities in Burkina Faso, Ghana and Tanzania: Similar finding. Trop Med Int Health 2013;18:534-47.
- Bang AT, Bang RA, Stoll BJ, Baitule SB, Reddy HM, Deshmukh MD. Is home-based diagnosis and treatment of neonatal sepsis feasible and effective? Seven years of intervention in the Gadchiroli field trial (1996 to 2003). J Perinatol 2005;25 Suppl 1:S62-71.
- Bang AT, Bang RA, Reddy HM, Deshmukh MD, Baitule SB. Reduced incidence of neonatal morbidities: Effect of home- based neonatal care in rural Gadchiroli, India. J Perinatol 2005;25 Suppl 1:S51-61.
- Grey M. Perspectives: The education of advanced practice nurses. Conn Med 2012;76:115-6.
- Greysen SR, Schiliro D, Curry L, Bradley EH, Horwitz LI. “Learning by doing” – Resident perspectives on developing competency in high-quality discharge care. J Gen Intern Med 2012;27:1188-94.
- Gill CJ, Phiri-Mazala G, Guerina NG, Kasimba J, Mulenga C, MacLeod WB, et al. Effect of training traditional birth attendants on neonatal mortality (Lufwanyama Neonatal Survival Project): Randomised controlled study. BMJ 2011;342:d346.
- Jayasuriya R, Whittaker M, Halim G, Matineau T. Rural health workers and their work environment: The role of inter-personal factors on job satisfaction of nurses in rural Papua New Guinea. BMC Health Serv Res 2012;12:156.
- Razee H, Whittaker M, Jayasuriya R, Yap L, Brentnall L. Listening to the rural health workers in Papua New Guinea- The social factors that influence their motivation to work. Soc Sci Med 2012;75:828-35.
- Index Mundi; Tanzania infant mortality rate. World Bank Indicators. Dar es Salaam, [Accessed on 13th July, 2012]: <http://www.indexmundi.com/facts/tanzania/ mortality-rate.>
- Mmbaga BT, Lie RT, Olomi R, Mahande MJ, Olola O, Daltveit AK. Causes of perinatal death at a tertiary care hospital in Northern Tanzania 2000-2010: A registry based study. BMC Pregnancy Childbirth 2012;12:139.
- Hinderaker SG, Olsen BE, Bergsjø PB, Gasheka P, Lie RT, Kvåle G. Perinatal mortality in northern rural Tanzania. J Health Popul Nutr 2003;21:8-17.
- Zinnen V, Paul E, Mwisongo A, Nyato D, Robert A. Motivation of human resources for health: A case study at rural district level in Tanzania. Int J Health Plann Manage 2012;27:327-47.
- Schmiegelow C, Minja D, Oesterholt M, Pehrson C, Suhrs HE, Boström S, et al. Factors associated with and causes of perinatal mortality in northeastern Tanzania. Acta Obstet Gynecol Scand 2012;91:1061-8.
- Kahabuka C, Moland KM, Kvåle G, Hinderaker SG. Unfulfilled expectations to services offered at primary health care facilities: Experiences of caretakers of underfive children in rural Tanzania. BMC Health Serv Res 2012;12:158.
- Kidanto HL, Massawe SN, Nystrom L, Lindmark G. Analysis of perinatal mortality at a teaching hospital in Dar es Salaam, Tanzania, 1999-2003. Afr J Reprod Health 2006;10:72-80.
- Kidanto HL, Mogren I, van Roosmalen J, Thomas AN, Massawe SN, Nystrom L, et al. Introduction of a qualitative perinatal audit at Muhimbili National Hospital, Dar es Salaam, Tanzania. BMC Pregnancy Childbirth 2009;9:45.
- Newton O, English M. Newborn resuscitation: Defining best practice for low-income settings. Trans R Soc Trop Med Hyg 2006;100:899-908.
- Nyamtema AS, Urassa DP, Massawe S, Massawe A, Lindmark G, van Roosmalen J. Partogram use in the Dar es Salaam perinatal care study. Int J Gynaecol Obstet 2008;100:37-40.
- Kumar D, Aggarwal AK, Kumar R. The effect of interrupted 5-day training on Integrated Management of Neonatal and Childhood Illness on the knowledge and skills of primary health care workers. Health Policy Plan 2009;24:94-100.
- Gathara D, Opiyo N, Wagai J, Ntoburi S, Ayieko P, Opondo C, et al. Quality of hospital care for sick newborns and severelymalnourished children in Kenya: A two-year descriptive study in 8 hospitals. BMC Health Serv Res 2011;11:307.
- Pattinson R, Kerber K, Waiswa P, Day LT, Mussell F, Asiruddin SK, et al. Perinatal mortality audit: Counting, accountability, and overcoming challenges in scaling up in low- and middle-income countries. Int J Gynaecol Obstet 2009;107 Suppl 1:S113-21, S121.
- Pattinson RC. Challenges in saving babies – Avoidable factors, missed opportunities and substandard care in perinatal deaths in South Africa. S Afr Med J 2003;93:450-5.
- Mbwele B, Reddy E, Reyburn H. A rapid assessment of the quality of neonatal healthcare in Kilimanjaro region, northeast Tanzania. BMC Pediatr 2012;12:182.
- World Health Organization. Workload Indicators of Staffing Need. Users Manual.WHO Press, World Health Organization, Geneva, Switzerland, 2010.
- Nyamtema AS, Urassa DP, Massawe S, Massawe A, LindmarkG, Van Roosmalen J. Staffing needs for quality perinatal care in Tanzania. Afr J Reprod Health 2008;12:113-24.
- Shipp P. Workload Indicators of Staffing Need (WISN): A Manual for Implementation. WHO Press, World Health Organization, Geneva, Switzerland, 1998.
- Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: A systematic analysis. Lancet 2010;375:1969-87.
- Masanja H, de Savigny D, Smithson P, Schellenberg J, John T, Mbuya C, et al. Child survival gains in Tanzania: Analysis of data from demographic and health surveys. Lancet 2008;371:1276-83.
- Mbwele B, Ide NL, Reddy E, Ward SA, Melnick JA, Masokoto FA, et al. Quality of neonatal healthcare in Kilimanjaro region, northeast Tanzania: Learning from mothers’ experiences. BMC Pediatr 2013;13:68.
- Opondo C, Ntoburi S, Wagai J, Wafula J, Wasunna A, Were F, et al. Are hospitals prepared to support newborn survival? -An evaluation of eight first-referral level hospitals in Kenya. Trop Med Int Health 2009;14:1165-72.
- Bowblis JR, Meng H, Hyer K. The urban-rural disparity in nursing home quality indicators: The case of facility-acquired contractures. Health Serv Res 2013;48:47-69.
- English M, Ntoburi S, Wagai J, Mbindyo P, Opiyo N, Ayieko P, et al. An intervention to improve paediatric and newborncare in Kenyan district hospitals: Understanding the context. Implement Sci 2009;4:42.
- Venkatachalam J, Kumar D, Gupta M, Aggarwal AK. Knowledge and skills of primary health care workers trained on integrated management of neonatal and childhood illness: Follow-up assessment 3 years after the training. Indian Public Health 2011;55:298-302.
- English M, Nzinga J, Mbindyo P, Ayieko P, Irimu G, MbaabuExplaining the effects of a multifaceted intervention to improve inpatient care in rural Kenyan hospitals – Interpretation based on retrospective examination of data from participant observation, quantitative and qualitative studies. Implement Sci 2011;6:124.
- Msemo G, Massawe A, Mmbando D, Rusibamayila N, Manji K, Kidanto HL, et al. Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training. Pediatrics 2013;131:e353-60.
- Yedidia MJ, Gillespie CC, Kachur E, Schwartz MD, Ockene J, Chepaitis AE, et al. Effect of communications training on medical student performance. JAMA 2003;290:1157-65.
- Goosby E, Dybul M, Fauci AS, Fu J, Walsh T, Needle R, et al. The United States President’s Emergency Plan for AIDS Relief: story of partnerships and smart investments to turn the tide of the global AIDS pandemic. J Acquir Immune Defic Syndr 2012;60 Suppl 3:S51-6.
- Evjen-Olsen B, Olsen OE, Kvåle G. Achieving progress in maternal and neonatal health through integrated and comprehensive healthcare services-Experiences from a programme in northern Tanzania. Int J Equity Health 2009;8:27.
- Acolet D. Quality of neonatal care and outcome. Arch Dis Child Fetal Neonatal Ed 2008;93:F69-73.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.