Live Birth Following a Term Pregnancy in a Non‑communicating Rudimentary Horn of a Unicornuate Uterus
- *Corresponding Author:
- Dr. Chukwuemeka Anthony Iyoke
Department of Obstetrics and Gynecology, University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu, Nigeria.
E-mail: caiyoke@yahoo.co.uk
Abstract
A case report of a live birth following a term pregnancy located in a non‑communicating rudimentary horn of a unicornuate uterus in a rural hospital in Nigeria is presented. A 32‑year‑old primiparous woman registered for antenatal care at a rural missionary hospital at 28 weeks gestation. She had intermittent unexplained vaginal bleeding prior to booking and multiple ultrasound scans in different centers affirmed a viable intrauterine pregnancy. She had an elective cesarean section at 38 weeks gestational age on account of a persistent oblique breech presentation and “low lying placenta.” Intra‑operatively, the pregnancy was found in a non‑communicating pouch continuous with the left fallopian tube and separate from the uterine cavity. A female baby weighing 2.2 kg with no gross deformity was delivered. Resection of the rudimentary horn and repair were done. The possibility of a uterine anomaly should be considered by clinicians and sonographers in unexplained intermittent early pregnancy bleeding.
Keywords
Live birth, Rudimentary horn, Term pregnancy, Unicornuate uterus
Introduction
Unicornuate uterus with a rudimentary horn is a very rare type of Mullerian duct anomaly and in up to 80% of cases there is no communication between the unicornuate uterus and the rudimentary horn.[1] Rudimentary horn pregnancy reaching term with live birth is also rare with only 13 fetal survivals reported in four decades from 1960.[1,2] Diagnosis of rudimentary horn pregnancy is challenging.[1,3,4] Clinical symptoms of rudimentary horn pregnancy include vaginal bleeding, lower abdominal pain: In situations where rupture had occurred, there may be dizziness, faintness and collapse. In only 29% of cases are diagnosis made prior to surgery.[1] Only few reports of rudimentary horn pregnancy emanate from Africa with no live births so far reported.[5,6] This case report highlights an unruptured term rudimentary horn pregnancy resulting in an intra-operative diagnosis and a live birth.
Case Report
Mrs. J.O. was a 32-year old secondigravida who had one previous vaginal delivery of a set of twins. She booked for antenatal care in the index pregnancy at a Catholic Mission Hospital in Cross River State Nigeria at a gestational age of 28+2 weeks. Prior to booking however, the pregnancy had been complicated by intermittent vaginal bleeding, abdominal pain and anemia for which she received care in several private hospitals from the 10th week of gestation to about the 24th week of gestation when the bleeding ceased spontaneously. Ultrasound scans performed in the course of her evaluation for the bleeding revealed different findings from the absence of intra-uterine gestational sac to single intrauterine gestation of compatible gestational age. One scan suggested hemoperitoneum and the possibility of a heterotopic pregnancy. All scans were performed outside the mission hospital.
At booking, she had no complaints. General physical examination was normal and the uterine fundal height was compatible with her gestational age with an indeterminate fetal lie. Fetal heart tones were normal. Her packed cell volume was 30.9 L/L and other routine investigations were normal. During her antenatal care subsequently, she only complained of occasional non-specific generalized abdominal discomfort.
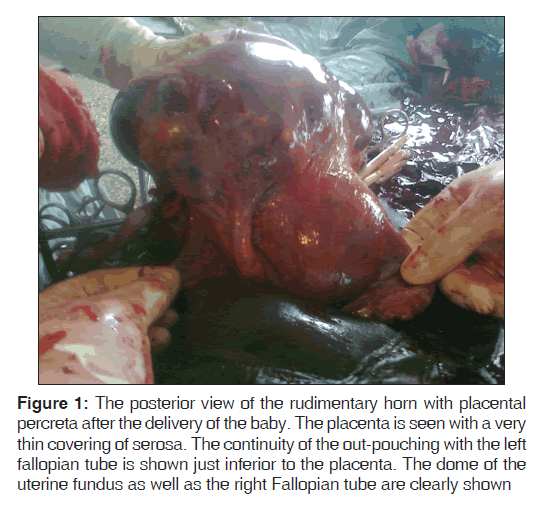
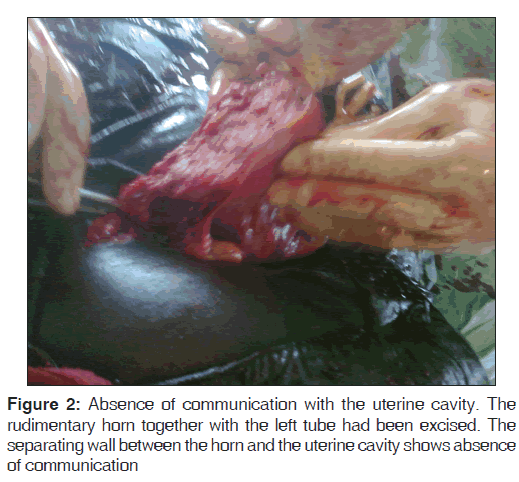
She had an elective cesarean section at 37 weeks gestation for a persistent oblique breech presentation and a “low lying placenta.” The abdominal cavity was entered through a Pfannenstiel incision. The baby was delivered through a low transverse uterine incision. Difficulty with delivery of the placenta resulted in heavy bleeding and prompted exteriorization of the uterus with the placenta. This revealed a morbidly adherent placenta in a non-communicating compartment in the left uterine cornu. The compartment was continuous with the left fallopian [Figures 1 and 2]. Further hemorrhage was controlled by the application of a size 18 G Foley’s catheter as a tourniquet at the level of the uterine isthmus such that both uterine arteries and the right infundibulopelvic ligament were compressed. Following this, the rudimentary horn, placenta and membranes were resected en-bloc with the left fallopian tube while preserving the left ovary. The uterine wall was repaired in two layers with No. 1 chromicised catgut. Two units of cross-matched and screened whole blood were transfused intra-operatively. The baby was female and weighed 2.2 kg. She had no obvious anomaly. Post-operative packed cell volume was 30.3 L/L. Mother and baby were discharged on the 6th post-operative day. Post-natal clinic visit at 6 weeks was unremarkable. Histology of the excised tissue showed “oedematous thin smooth muscle layer enclosing dense eosinophilic areas containing a mixture of blood clots, decidual cells and few chorionic villi. Tubal epithelium also appeared oedematous.”
Figure 1: The posterior view of the rudimentary horn with placental percreta after the delivery of the baby. The placenta is seen with a very thin covering of serosa. The continuity of the out-pouching with the left fallopian tube is shown just inferior to the placenta. The dome of the uterine fundus as well as the right Fallopian tube are clearly shown
Discussion
This is a rare case of a live birth following a term pregnancy in a non-communicating rudimentary horn of a unicornuate uterus (class IIb Mullerian duct anomaly based on the classifications of the American Society of Reproductive Medicine 1988).[7] The case highlights the challenges posed to accurate prenatal diagnosis and intra-partum surgical management of gestations associated with Mullerian duct anomalies. This was a case of missed prenatal diagnosis. The differential diagnoses included pregnancy in one horn of a complete bicornuate uterus, or a gestation in a complete septated uterus. In both of these situations, the gestational cavity should have had continuity with the cervix which was not the case here.
Rudimentary horn pregnancy is a very rare condition. Previous reports suggest that it was first described in 1669 by Mauriceau and Vassal.[1] It is approximately 10-fold less common than abdominal pregnancy.[1] The incidence of rudimentary horn pregnancy is quoted as 1:76000-1:140000.[1,8] Between 1960 and 2003, Jayasinghe and co documented 156 cases,[1] whereas Nahum documented 558 cases between 1900 and 1999.[9] Rudimentary horn is non-communicating in 80% of cases and may occur without a unicornuate uterus.[1,10] The attachment of the rudimentary horn may vary from a fibro-muscular band (separated variety) to an extensive fusion between the two horns where there is no external separation between them.[1,5] This was a case with an extensive fusion between the two horns.
Tsafrir and co-workers have suggested ultrasound criteria for prenatal diagnosis of rudimentary horn pregnancy. These include pregnancy sac surrounded by myometrium by the side of a normal empty uterus; non-communication of the gestational sac with the endometrial cavity and cervix and pseudo pattern of an asymmetrical bicornuate uterus.[2] Ultrasonography is critical in early diagnosis and confirmation with magnetic resonance imaging may be necessary in cases where ultrasound findings are unclear.[2] In all cases of uterine anomaly, the possibility of anomalies of the urinary tract must be excluded. This case presents a clear failure of antenatal diagnosis, which may not be surprising considering the rarity of the condition and the inherent difficulty in achieving a prenatal ultrasound diagnosis.
Once a diagnosis of rudimentary horn pregnancy is made, the treatment is surgery. This will help to avert spontaneous rupture with possible catastrophic consequences. The surgical management of rudimentary pregnancy can also be challenging. Laparoscopic removal is used in early pregnancy.[4,11] The use of a tourniquet to reduce haemorrhage during caesarean delivery is unconventional. It had been previously described by Buntugu et al. for a rudimentary horn delivery.[5] Its use in this patient was to avert the severe haemorrhage, which could have resulted from either the well fused horns or the morbidly adherent placenta or both.[5]
By far the most life threatening complication is rupture of the uterus which can occur spontaneously or following induction of labour.[12] Neonatal survival following rudimentary horn pregnancy is poor. Reports suggest only 11% in the last 50 years.[13]
Conclusion
Rudimentary horn pregnancies like in this case are difficult to diagnose and challenging to treat. This case alerts clinicians and sonographers in our environment to the possibility of a uterine anomaly in unexplained persistent early pregnancy bleeding.
Acknowledgment
We thank the patient and the authorities of Catholic Mission Hospital Moniyan Ogoja for permission to publish this.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Jayasinghe Y, Rane A, Stalewski H, Grover S. The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol 2005;105:1456-67.
- Patra S, Puri M, Trivedi SS, Yadav R, Bali J. Unruptured term pregnancy with a live fetus with placenta percreta in a non-communicating rudimentary horn. Congenit Anom (Kyoto) 2007;47:156-7.
- Tsafrir A, Rojansky N, Sela HY, Gomori JM, Nadjari M. Rudimentary horn pregnancy: First-trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J Ultrasound Med 2005;24:219-23.
- Wang B, Zhou JH, Jin HM. Torsion of a rudimentary uterine horn at 22 weeks of gestation. J Obstet Gynaecol Res 2011;37:919-20.
- Buntugu K, Ntumy M, Ameh E, Obed S. Rudimentary horn pregnancy: Pre-rupture diagnosis and management. Ghana Med J 2008;42:92-4.
- Bolandi MS. A ruptured rudimentary horn of a unicornuate uterus at 18 weeks. Obstet Gynaecol Forum 2011;21:25-7.
- Bhatla N. Malformations and maldevelopments of the genital tract. Jeffcoate’s Principles of Gynaecology. International ed. London: Arnold; 2001. p. 148.
- Dahiya K, Duhn N, Nanda S. Rudimentary horn pregnancy: Series of four cases and review of literature. J Gynaecol Surg 2011;27:139.
- Nahum GG. Rudimentary uterine horn pregnancy. The 20th-century worldwide experience of 588 cases. J Reprod Med 2002;47:151-63.
- Shin JW, Kim HJ. Case of live birth in a non-communicating rudimentary horn pregnancy. J Obstet Gynaecol Res 2005;31:329-31.
- Goel P, Saha PK, Mehra R, Huria A. Unruptured postdated pregnancy with a live fetus in a noncommunicating rudimentary horn. Indian J Med Sci 2007;61:23-7.
- Samuels TA, Awonuga A. Second-trimester rudimentary uterine horn pregnancy: Rupture after labor induction with misoprostol. Obstet Gynecol 2005;106:1160-2.
- Nissi R, Salanta M, Talvensaan-Mattila A. Rudimentary uterine horn pregnancy in a patient with a previous vaginal delivery. J Gynaecol Surg 2010;26:271-2.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.