Loop Drainage Technique vs. Conventional Incision and Drainage for Management of Skin and Soft Tissue Abscesses: Systematic Review and Meta-analysis
2 Department of Medicine, Dar Al Uloom University, Riyadh, Saudi Arabia
Published: 31-Dec-2021
Citation: Alsayed AS, et al. Loop Drainage Technique vs.Conventional Incision and Drainage for Management of Skin and Soft Tissue Abscesses: Systematic Review and Meta-analysis. Ann Med Health Sci Res.2021;11:21-25.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: The loop approach is an alternative to packing that does not require large incisions can be used in both small and big abscesses, preventing premature closure and fostering prolonged drainage in the same way as packing does. Aim: This work aims to determine the efficacy and safety of the Loop Drainage Technique (LDT) versus Conventional Incision and Drainage (CID) for the management of skin and soft tissue abscesses. Materials & Methods: A systematic search was performed over different medical databases to identify general surgery studies, which studied the outcome of the LDT group versus the CID group of skin and soft tissue abscesses patients. We conducted a meta-analysis process on the overall failure rate as a primary outcome (failure is defined as the need for repeat incision and drainage, intravenous antibiotics, admission, or surgical intervention). The failure rate in adult and pediatric patients is considered secondary outcomes. Results: Seven studies were identified involving 877 patients, with 410 patients in the LDT group, and 467 patients in the CID group. Our meta-analysis process showed a highly significant decrease in the overall failure rate in the LDT group compared to the CID group (p=0.01). Also, we found a non-significant difference in failure rate in adult patients (p>0.05), and a highly significant decrease in failure rate in pediatric patients in the LDT group compared to the CID group (p=0.003). Conclusion: To conclude, the Loop drainage technique for management of skin and soft tissue abscesses is better in a decrease in the overall failure rate (need for repeat incision and drainage, intravenous antibiotics, admission, or surgical intervention) also decrease failure rate in pediatric patients but not significant in decrease failure rate in adult when compared to conventional incision technique.
Keywords
Loop drainage; Incision; Drainage, Skin; Soft tissue abscesses
Introduction
In the emergency room, cutaneous abscesses are commonly treated. In the United States, nearly 1.4 million Incisions and Drainage (I&D) procedures for these infections are performed each year. [1] While some sort of I&D is certainly the gold standard, additional abscess cavity packing is debatable. [2] I&D with or without oral antibiotics, packing, or drainage are all alternatives for outpatient management of cutaneous abscesses. Since community-acquired Methicillin-Resistant Staphylococcus Aureus (ca-MRSA) has emerged as the most common cause of abscess formation, complete I&D and judicious antibiotic administration have become increasingly important. Antibiotics have historically been recommended following I&D, although research suggests that antibiotic usage is ineffective for simple abscesses. [3] The American College of Emergency Physicians (ACEP) "choosing wisely guidelines" and the Infectious Disease Society of America (IDSA) have previously advised against using antibiotics in a variety of situations. The use of I&D alone to treat cutaneous abscesses is becoming more common; the effective technique is especially crucial. The LOOP procedure, which involves inserting one or more vascular loops around the abscess cavity, is an alternative to standard packing that keeps the abscess chamber draining. [4]
The LOOP approach is an alternative to packing that does not require large incisions can be used in both small and big abscesses, preventing premature closure and fostering prolonged drainage in the same way as packing does. [5] After the loculations are bluntly opened and the cavity is irrigated, and an avascular loop is introduced into the abscess cavity through two tiny incisions. The vascular loop is loosely tied and left in place for several days to allow the wound to drain, after which it is cut and gently retracted from the wound. Multiple vascular loops can be implanted to span the whole abscess cavity if the abscess is large. It is not necessary to modify or replace vessel loops. [6]
This work aims to determine the efficacy and safety of the Loop Drainage Technique (LDT) vs. Conventional Incision and Drainage (CID) for the management of skin and soft tissue abscesses.
Literature Review
Our review came following the (PRISMA) statement guidelines. [7]
Study eligibility
The included studies should be in english, a journal published article, and a human study describing skin and soft tissue abscesses patients. The excluded studies were either animal or non-english studies or articles describing deep abscesses.
Study identification
Basic searching was done over the PubMed, Cochrane library, and Google scholar using the following keywords: loop drainage, incision and drainage, skin and soft tissue abscesses.
Data Extraction
Comparative studies, clinical trials, and Randomized Controlled Trials (RCTs), which studied the outcome of the LDT group vs. CID group of skin and soft tissue abscesses patients, will be reviewed. Outcome measures included the overall failure rate as a primary outcome (failure is defined as the need for repeat incision and drainage, intravenous antibiotics, admission, or surgical intervention). The failure rate in adult and pediatric patients is considered secondary outcomes.
Study selection
We found 80 records, 50 excluded because of the title; 30 articles are searched for eligibility by full-text review; 10 articles cannot be accessed; 5 studies were reviews and case reports; the desired procedure not used in 8 studies. The studies which met all inclusion criteria were 7 studies.
Statistical Analysis
Pooled Odds Ratios (OR), Proportions (%), with 95% Confidence Intervals (CI) assessed, using a statistical package (MedCalc, Belgium). The meta-analysis process was established via I2-statistics (either the fixed-effects model or the random-effects model), according to the Q test for heterogeneity.
The included studies were published between 2011 and 2020. Regarding the type of included studies, 4 studies (out of 7 studies) were RCTs, while 3 studies were retrospective. Regarding patients’ characteristics, the total number of patients in all the included studies was 877 patients, with 410 patients in the LDT group, and 467 patients in the CID group, while their average empiric antibiotic use was (95%). The mean age of all patients was (21.4 years) [Table 1]. [8-14] Our meta-analysis included 7 studies comparing 2 different groups of patients; with a total number of patients (N=877) [Table 2].
| N | Author | Type of study | Number of patients | Age | Empiric antibiotic use (%) | ||
|---|---|---|---|---|---|---|---|
| Total | LDT group | CID group | (average years) | ||||
| 1 | McNamara et al. [8] | Retrospective | 219 | 85 | 134 | 7 | 100 |
| 2 | JG Ladde et al. [9] | Retrospective | 142 | 51 | 91 | 2 | 88 |
| 3 | Özturan et al. [10] | RCT | 46 | 23 | 23 | 35.5 | --- |
| 4 | Gaszynski et al. [11] | Retrospective | 53 | 36 | 17 | 38.8 | 100 |
| 5 | Rencher et al. [12] | RCT | 81 | 41 | 40 | 7.2 | 93.8 |
| 6 | J Ladde et al. [13] | RCT | 196 | 99 | 97 | 22 | 94.9 |
| 7 | Schechter-Perkins et al. [14] | RCT | 140 | 75 | 65 | 37.5 | --- |
Table 1: Patients and study characteristics.
| N | Author | Primary outcome | Secondary outcomes | ||||
|---|---|---|---|---|---|---|---|
| Overall failure rate | The failure rate in adult patients | The failure rate in pediatric patients | |||||
| LDT group | CID group | LDT group | CID group | LDT group | CID group | ||
| 1 | McNamara et al. | 0 | 1 | --- | --- | 0 | 1 |
| 2 | JG Ladde et al. | 2 | 15 | --- | --- | 2 | 15 |
| 3 | Özturan et al. | 6 | 9 | 6 | 9 | --- | --- |
| 4 | Gaszynski et al. | 0 | 0 | 0 | 0 | --- | --- |
| 5 | Rencher et al. | 3 | 3 | --- | --- | 3 | 3 |
| 6 | J Ladde et al. | 13 | 19 | 13 | 10 | 0 | 9 |
| 7 | Schechter et al. | 9 | 12 | 9 | 12 | --- | --- |
Table 2: Summary of outcome measures in all studies.
Each outcome was measured by
Odds Ratio (OR)
•For the overall failure rate
•For failure rate in adult patients
•For failure rate in pediatric patients
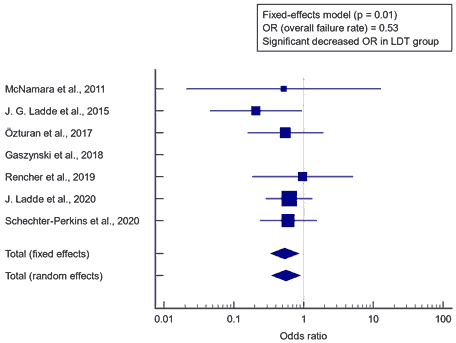
Concerning the primary outcome measure, we found 7 studies reported the overall failure rate. I2 (inconsistency) was 0%, Q test for heterogeneity (p>0.05), so fixed-effects model was carried out; with overall OR=0.53 (95% CI=0.336 to 0.859). The fixed-effects model of the meta-analysis process revealed a highly significant decrease in the overall failure rate in the LDT group compared to the CID group (p=0.01) [Figure 1].
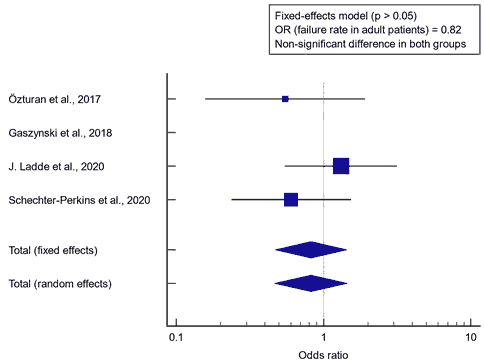
Concerning the secondary outcome measures, we found 4 studies reported failure rate in adult patients. I2 (inconsistency) was 0%, Q test for heterogeneity (p>0.05), so fixed-effects model was carried out; with overall OR= 0.82 (95% CI=0.469 to 1.444). The fixed-effects model of the meta-analysis process revealed a non-significant difference in failure rate in adult patients in the LDT group compared to the CID group (p>0.05) [Figure 2].
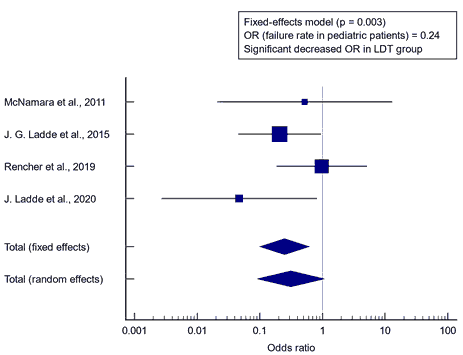
We found 4 studies reported failure rate in pediatric patients. I2 (inconsistency) was 27.9%, Q test for heterogeneity (p>0.05), so fixed-effects model was carried out; with overall OR=0.24 (95% CI=0.100 to 0.615). The fixed-effects model of the meta-analysis process revealed a highly significant decrease in failure rate in pediatric patients in the LDT group compared to the CID group (p=0.003) [Figure 3].
Discussion
This work aims to determine the efficacy and safety of the Loop Drainage Technique (LDT) versus Conventional Incision and Drainage (CID) for the management of skin and soft tissue abscesses. The included studies were published between 2011 and 2020. Regarding the type of included studies, 4 studies (out of 7 studies) were RCTs, while 3 studies were retrospective. Regarding patients’ characteristics, the total number of patients in all the included studies was 877 patients, with 410 patients in the LDT group, and 467 patients in the CID group, while their average empiric antibiotic use was (95%). The mean age of all patients was (21.4 years). Our meta-analysis included 7 studies comparing 2 different groups of patients; with a total number of patients (N=877). Concerning the primary outcome measure, we found 7 studies reported the overall failure rate. Using the fixed-effects model of the meta-analysis process revealed a highly significant decrease in the overall failure rate in the LDT group compared to the CID group (p=0.01) which came in agreement with Gottlieb et al.; Gottlieb et al.; Long et al. [5,15,16]
Gottlieb et al. found that, when compared to CID, a meta-analysis of eight studies (n=910 individuals) found that the LDT resulted in fewer treatment failures. When only randomized controlled trials were considered, the result remained the same. However, no difference was identified in the adult and pediatric subgroups. [15] Long et al. reported that, when compared to traditional incision and drainage, the loop drainage approach has a lower risk of treatment failure. Gottlieb found that a study of data from four trials revealed that the LOOP had a lower failure rate than standard incision and packing, with an Odds Ratio (OR) of 2.63 in favor of failure, but additional research is needed. [5]
Concerning the secondary outcome measures, we found 4 studies that reported failure rates in adult patients. Using the fixed-effects model of the meta-analysis process revealed a non-significant difference in failure rate in adult patients in the LDT group compared to the CID group (p>0.05) which came in agreement with Salfity et al.; Schechter et al. [17,18]
Salfity et al. reported that the majority of the patients in this study were admitted to the hospital with a perirectal abscess (95.7% vs. 94.7%, P>0.05) and similar abscess diameters (5.1 cm vs. 4.08 cm). Even while the conventional group had a larger rate of patients with recurring abscesses, the difference was not statistically significant. Similarly, there was no difference in the proportion of patients readmitted in either group (21.2% versus 14.3%, P>0.05). Schechter et al. reported that between the two therapy groups, there was no significant difference in complications requiring hospitalization (5.9% vs. 6.1%).
Concerning the secondary outcome measures, we found 4 studies that reported failure rates in pediatric patients. Using fixed-effects model of the meta-analysis process revealed a highly significant decrease in failure rate in pediatric patients in the LDT group compared to the CID group (p=0.003) which came in agreement with Aprahamian et al.; Hamreus et al.; Ladd et al.; Lautz et al.; Aprahamian, et al; reported that micro incisions and loop drainage are safe and efficient therapy options for children with subcutaneous abscesses. [19-22] The findings reduce the need for repeated wound packing and make postoperative wound management more straight forward. Loop drainage allows for a faster discharge time, decreased recurrence rates, and less scarring.
Hamreus, et al. reported that, when compared to open drainage, loop drainage results in lower costs, shorter hospital stays, and a lower rate of operation failure in pediatric patients with subcutaneous abscesses. [20] Ladd et al. performed a retrospective assessment of 128 pediatric patients who had cutaneous abscesses and were treated with loop drains. There were no recurrences or severe morbidity associated with the operation. Loop drains are a successful approach for draining and treating complex abscesses in children with poor postoperative wound care. [21]
Lautz et al. found that Incision and loop drainage in the treatment of subcutaneous abscesses in children in all anatomical regions was demonstrated to be safe and successful. These discoveries minimize the need for repeated wound packing and make postoperative wound management more straightforward. Compared to other procedures, loop drainage takes less time to discharge and has a lower recurrence rate. [22] On other hand, our result came in disagreement with Seal et al. who compared the effects of I&D with packing against vascular loops on abscess drainage in children observed that no difference in complication/treatment failures or return PED visits between the two approaches. [23]
Conclusion
To conclude, the Loop drainage technique for management of skin and soft tissue abscesses is better in a decrease in the overall failure rate (need for repeat incision and drainage, intravenous antibiotics, admission, or surgical intervention) also decrease failure rate in pediatric patients but not significant in decrease failure rate in adult when compared to Conventional incision technique.
Acknowledgment
All the listed authors contributed significantly to the conception and design of study, acquisition, analysis, and interpretation of data and drafting of the manuscript, to justify authorship.
References
- Merritt C, Haran JP, Mintzer J, Stricker J, Merchant RC. All purulence is local-epidemiology and management of skin and soft tissue infections in three urban emergency departments. BMC Emerg Med. 2013;13:1-9.
- List M, Headlee D, Kondratuk K. Treatment of skin abscesses: A review of wound packing and post-procedural antibiotics. South Dakota Medicine 2016;69.
- Hankin A, Everett WW. Are antibiotics necessary after incision and drainage of a cutaneous abscess? Ann Emerg Med. 2007;50:49-51.
- Gaszynski R, Punch G, Verschuer K. Loop and drain technique for subcutaneous abscess: A safe minimally invasive procedure in an adult population. ANZ J Surg. 2018;88:87-90.
- Gottlieb M, Peksa GD. Comparison of the loop technique with incision and drainage for soft tissue abscesses: A systematic review and meta-analysis. Am J Emerg Med. 2018;36:128-133.
- Ladde J, Baker S, Lilburn N, Wan M, Papa L. A randomized controlled trial of novel loop drainage technique versus standard incision and drainage in the treatment of skin abscesses. Acad Emerg Med. 2020;27:1229-1240.
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. Bmj 2009;339.
- Namara WFM, Hartin CW, Escobar MA, Yamout SZ, Lau ST, Lee YH. An alternative to open incision and drainage for community-acquired soft tissue abscesses in children. J Pediatr Surg. 2011;46:502-506.
- Ladde JG, Baker S, Rodgers CN, Papa L. The LOOP technique: A novel incision and drainage technique in the treatment of skin abscesses in a pediatric ED. Am J Emerg Med. 2015;33:271-276.
- Özturan İU, Doğan NÖ, Karakayalı O, Özbek AE, Yılmaz S, Pekdemir M, et al. Comparison of loop and primary incision & drainage techniques in adult patients with cutaneous abscess: A preliminary, randomized clinical trial. Am J Emerg Med. 2017;35:830-834.
- Gaszynski R, Punch G, Verschuer K. Loop and drain technique for subcutaneous abscess: A safe minimally invasive procedure in an adult population. ANZ J Surg. 2018;88:87-90.
- Rencher L, Whitaker W, Schechter EP, Wilkinson M. Comparison of minimally invasive loop drainage and standard incision and drainage of cutaneous abscesses in children presenting to a pediatric emergency department: A prospective, randomized, noninferiority trial. Pediatr Emerg Care. 2019.
- Ladde J, Baker S, Lilburn N, Wan M, Papa L. A randomized controlled trial of novel loop drainage technique versus standard incision and drainage in the treatment of skin abscesses. Acad Emerg Med. 2020;27:1229-1240.
- Schechter EMP, Dwyer KH, Amin A, Tyler MD, Liu J, Nelson KP, et al. Loop drainage is non-inferior to traditional incision and drainage of cutaneous abscesses in the emergency department. Acad Emerg Med. 2020;27:1150-1157.
- Gottlieb M, Schmitz G, Peksa GD. Comparison of the loop technique with incision and drainage for skin and soft tissue abscesses: A systematic review and meta-analysis. Acad Emerg Med 2021;28:346-354.
- Long B, April MD. Is loop drainage technique more effective for treatment of soft tissue abscess compared with conventional incision and drainage? Ann Emerg Med. 2019;73:19-21.
- Salfity HV, Valsangkar N, Schultz M, Salfity J, Maxey KJS, Zarzaur B, et al. Minimally invasive incision and drainage technique in the treatment of simple subcutaneous abscess in adults. Am Surg. 2017;83:699-703.
- Schechter EMP, Dwyer KH, Amin A, Tyler MD, Liu J, Nelson KP, et al. 182 loop drainage is non-inferior to traditional incision and drainage of cutaneous abscesses in the emergency department. Ann Emerg Med. 2017;70:S73-S74.
- Aprahamian CJ, Nashad HH, Somma NMD, Elger BM, Esparaz JR, Morrow TJM, et al. Treatment of subcutaneous abscesses in children with incision and loop drainage: A simplified method of care. J Pediatr Surg. 2017;52:1438-1441.
- Hamreus K. Loop drainage of subcutaneous abscesses in pediatric patients. 2016.
- Ladd AP, Levy MS, Quilty J. Minimally invasive technique in treatment of complex, subcutaneous abscesses in children. J Pediatr Surg. 2010;45:1562-1566.
- Lautz TB, Raval MV, Barsness KA. Increasing national burden of hospitalizations for skin and soft tissue infections in children. J Pediatr Surg. 2011;46:1935-1941.
- Seal RS, Tuuri R, Hayden G, Losek J, Cina R, Small J. 210 A retrospective institutional review of vessel loops for incision and drainage of abscesses in the pediatric emergency department. Ann Emerg Med. 2016;68:S82.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.