Management of Severe Chest Injury, Dodoma Referral Hospital Experience
Received: 21-Oct-2022, Manuscript No. AMHSR-22-78009; Editor assigned: 24-Oct-2022, Pre QC No. AMHSR-22-78009 (PQ); Reviewed: 07-Nov-2022 QC No. AMHSR-22-78009; Revised: 22-Feb-2023, Manuscript No. AMHSR-22-78009 (R); Published: 01-Mar-2023, DOI: 10.54608.annalsmedical.2023.94
Citation: Mbelle PJ, et al. Management of Severe Chest Injury, Dodoma Referral Hospital Experience. Ann Med Health Sci Res. 2023;13:500-506
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Chest injuries continue to be major healthy surgical problem, worldwide the surgical admission and death related to penetrating and blunt chest injuries are estimated to be 10% and 25% respectively. It is life threatening condition and usually involves other anatomical area which can worsen the general condition of patients because of inflammatory response. In Tanzania the mortality related with chest injuries is estimated to be 40%. The common mechanism of injury being road traffic accidents, ire arms, falls, arrows, wild animal injuries, assaults etc. The injuries can involve thorax wall, lungs, mediastinum or diaphragmatic wounds. The common diagnosed conditions includes frail chest, fractured ribs, contused lung, hemothorax, pnemothorax, oesophageal rapture, tracheabronchial tree injury, diaphragmatic injury, cardiac injury, tension pneumothorax, open pneumothorax etc. Treatment of thoracic trauma depends on effective prioritization of management based on the principals of ABC with a rapid identi ication of severe injuries and aggressive surgical treatment of life threatening injuries.
Keywords
Thorax; Trauma; Blunt; Penetrating; Thoracotomy; Pneumothorax; Hemothorax; Frail
Key Points
• Multidisplinary team approach is mandatory for the proper management of severe chest injury.
• Advanced trauma life support protocol (ABCDE) can easily detect the life threatening condition for the immediate intervention.
• Despite of good surgical outcome, management with rib fixation is an area of additional study.
• Hemopnemothorax can be managed successfully with tube thoracotomy unless the patient has massive hemotharax >200 mls/h which might require emergency thoracotomy.
• Definitive surgical intervention should be conducted after achieving stability of the patient.
Introduction
Chest injury remain to be common contributor of morbidity and mortality. Despite of having few cases of severe chest injuries, the occurrence of none severe form of thoracic injuries in our set up is still remarkable, the thoracic injuries account significantly in magnitude of surgical hospitalization, prolonged hospital stay and cost of patient care. The study done by massaga reported the mortality rate caused by chest injury patients was about 24.2%, and these injuries are associated with other injuries which can be abdomen, head, and orthopedic traumas. The incidence of severe chest injuries is uncommon in our set up, however the common thoracic injuries being blunt chest injuries, penetrating injuries, pneumothorax, hemothorax, fractured ribs, contused lungs etc. Most of these chest injuries can be easily detected by physical examination and simple radiological work up like chest ray and sonography (FAST), which are available in our environment. Advanced radiological imaging like CT scan is rarely used because is not available in every peripheral healthy facility. An intergrated approach and cooperative multidisciplinary team of healthy workers are mandatory in achieving an effective management of severe thoracic injuries.
Case Presentation
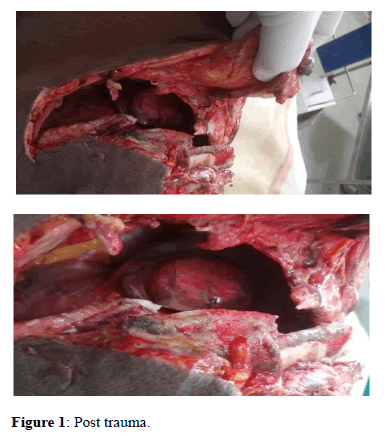
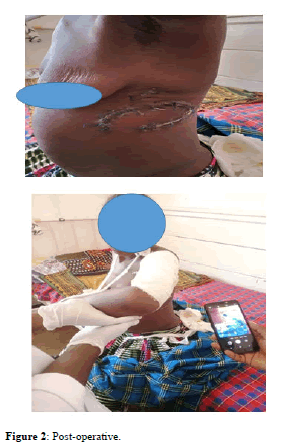
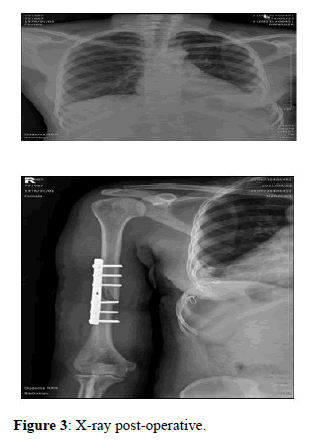
M.H.M female 45 years of age, peasant with history of being hurt by an elephant trunk while working in the farm and sustained open left chest injury which caused 5 ribs fracture, exposed lower and middle lung lobes, and severe loss of blood. The event was associated with injury of left upper arm, hypovolemic shock and deterioration of loss of consciousness. Upon physical examination patient was found to be semiconscious, GCS 12/15, severe pale, dyspneic with cold extrimities, BP was 90/40, weak pulse 120/min, RR 32/ min, spO2 82, she had wound on the left thorax (10 cm × 25 cm size), exposed diaphragm, pericardium and collapsed left lung. She had devitalized tissues, 5 visible fractured ribs, missing segments 6th -10th rib and deformed left upper arm. WBC 15.1, RBC 3.16, HB 9.6, platelets 93, neutrophils 14.2, RBG 7.4, normal serum electrolytes. The focused sonographic assessment revealed negative in other spaces, chest X ray showed multiple ribs fracture 6th -10th rib, with closed fractured left humeral bone. Therefore clinically the patient was concluded to have open Hemopnemothorax with multiple fractured ribs and closed fractured left humerus. The patient was approached by ATLS approach. Aggressive resuscitation included 3 units of whole blood, 1 platelets, 1 FFP and crystalloids fluids/6l’s were given. The antibiotics to cover gram negative and positive were initiated, then surgical intervention was conducted when hemodynamic stability was established. Intraoperative the patient underwent surgical debridement, repair of damaged lower lobe of lung, wire fixation of the fractured ribs, repair of chest wall soft tissue and tube thoracotomy with active sanction was applied. The patient was closely monitored in ICU with significant improvement. The fractured humerus was stabilized by back pop slab and ORIF was done after two weeks later (Figures 1-3).
Discussion
Trauma contributes significantly in causing morbidity and mortality in the poor and developed world, about 10% of trauma admission world wide are due to chest injuries which contributes 25% of deaths. And when it is associated with other lesions produces more fatal outcome in additional of all 50% polytrauma patients accompanied with cardiovascular system trauma. Also the chest injuries have been reported to be the leading cause of death, hospitalization, and long-term disabilities in the first four decades of life [1-4]. The kind of chest injuries are different depending on nature of cause and severity of accidents around the world. The injuries can involve thorax wall, lungs, mediastinum or diaphragmatic wounds. In Tanzania the mortality related with chest injuries is estimated to be contributed by 40%, and it has been reported to be the common cause of surgical admission with high morbidity and mortality [5,6]. There is variation of common causes of chest injury because of different nature of occupation however the road traffic accidents accounts 70% and others being fire arms, falls, arrows, assaults etc. [7]. Most of patients provide history of trauma unless they arise with altered mental status, on physical evaluation they have contusions, lacerations, open wound, deformity, emphysema, reduced or absence of breath sound on affected thorax and crepitus. For full awake patients might present with respiratory distress and paradoxical movement. Chest trauma can arise with pulmonary deterioration and other complication, the risk is so prominent in older patients which have increased ventilator days, pneumonia, and acute respiratory distress syndrome compared with younger patients [9-12]. Mechanism of injury has the role to play when identifying chest injuries, thoracic injuries are usually penetrating or blunt trauma. Blunt trauma is usually caused by events which increase intrathoracic pressure such as car collisions and falls. Penetrating trauma commonly can be due to gun short, stab wounds, and rarely impalement. These injuries are life threatening, sometimes can present without obvious external signs and therefore should be paid attention during patient evaluation. Penetrating trauma may cause pneumothorax or haemothorax with massive blood loss, and some patients after chest trauma deteriorate rapidly and can improve only if given proper management. In patients with penetrating injuries surgical operations are frequently indicated, while diagnostic investigations are less required than in blunt trauma. In some cases, the distinction between blunt and penetrating thoracic trauma should have high index of suspicious because penetrating injuries often coexist with severe blunt injuries of solid organs and major vessels. [13,14]. Penetrating thoracic trauma can be associated with laceration of heart, major vessels, intercostal vessels, airways, lung, oesophagus, and diaphragm, intra-abdominal and retroperitoneal organs. Blunt and crush thoracic trauma may cause cardiac contusion, lung contusion, rib fractures, thoracic spine fractures, rupture of bronchus, oesophagus, frail etc. Deceleration and blast mechanism thoracic trauma may cause aortic rupture, airway damage, diaphragmatic rupture, and disruption of any intrathoracic organ and vessel [15]. Regardless of its mechanism and pattern, the main consequence of thoracic trauma is reduction of vital functions such as respiration and circulation leading to hypoxia, hypovolemia, and reduced cardiac output. The sequelae of this injury have a detrimental effect on organs beyond the chest cavity, e.g kidneys, liver, brain, gastrointestinal tract. Treatment of thoracic trauma depends on effective prioritization of management based on the principals of ABC, with a rapid identification of severe injuries and aggressive surgical treatment of life threatening injuries. Patients with chest trauma might be physiologically stable or unstable, therefore the initial assessment of any injured patient must place priority the evaluation of the airway and the cardiovascular system in accordance with ABC algorithm. A rapid physical examination will determine if the patient is cyanotic, tachypneic or has other existing respiration problem. In the patient with a penetrating or blunt injury with hemodynamic instability, most likely has hemorrhage occurring into the chest therefore should be taken to the hospital with no delay. It is important to insert a chest tube as soon as possible during the initial assessment and resuscitation in the emergency department. Bilateral chest tubes may be indicated and chest x-ray can used to confirm tube placement [16-17]. Focused Assessment with Sonography for Trauma (FAST) has been widely used in trauma centers and emergency departments. It is a rapid and non invasive, ultrasound diagnostic protocol is used both in hemo-dynamically unstable and stable patients with penetrating or blunt injuries. It may be very usefully in identifying cardiac tamponade, haemothorax and haemoperitoneum [18]. In patients with hemodynamic instability, a plain Antero Posterior (AP) chest radiograph is still a gold diagnostic standard to identify pneumothorax or haemothorax. The FAST examination should be performed within 10 minutes since the patient’s arrival at the emergency department. A thoracic radiograph before placement of a chest tube may be helpful in excluding rupture of a diaphragm with possible herniation of a stomach or intestines to the pleural cavity, especially in patients following blunt trauma. Clinical signs in patients with chest injuries sometimes are misleading [19]. Therefore, the thoracic radiograph helps to identify important lesions which require emergency surgical intervention or may suggest further investigations such as: CT scan, FAST, Transoesophageal Echocardiography (TEE) or thoracoscopy and laparoscopy [20].
Whole Body Computerized Tomography (WBCT) is a widely accepted diagnostic tool in the primary management of patients following major trauma. WBCT is indicated even when the patient is haemodynamically unstable, it may identify severe injuries within short time. Management of specific chest injury depends on the condition of a patient arriving to the hospital, it is important to identify and treat airway obstruction as soon as possible during the primary survey at the emergency department.
Pneumothorax is a common injury in both blunt and penetrating thoracic trauma, the condition is not an immediately threatening but it can progress and cause loss of life. Simple pneumothorax might be asymptomatic, however many cases present with ipsilateral chest pain, absent or diminished breath sounds, hyper resonance to percussion, shortness of breath, dyspnea, and subcutaneous emphysema of the chest wall. Hypoxia and tachypnea may also be present.
Open pneumothorax is commonly diagnosed as a result of a penetrating wound that creates a direct connection between the pleural space and the outside world. This equilibrates the intrathoracic pressure with atmospheric pressure and disrupts the physiologic pressure gradient that drives respiration. Alternatively the negative intrathoracic pressure generated during inspiration draws air into the chest via wound. The wound subsequently closes down creating a large pneumothorax. This so called “sucking chest wound” can occur in a variety of traumatic mechanisms, including blast injuries, high velocity gunshot wounds, slash injuries with large soft tissue defects and impalement.
The diagnosis of a simple pneumothorax is confirmed by chest radiographs or CT scan, with the increasing prevalence of CT imaging in the evaluation of blunt trauma patients, it can identify pneumothoraces which can not be seen on radiographs. These ‘occult’ pneumothoraces are occurring in 15% to 20% of blunt trauma patients and some times in 17% of penetrating trauma patients.
Ultrasound imaging can also be used to diagnose pneumothorax, which can show Ultrasonographic findings such as comet tail artifacts or B-lines being created between the water and air interface of the visceral pleura in normal lung. Pneumothorax is identified by the absence of lung sliding, loss of comet tail artifacts, the presence of A-lines, and the lung point sign all suggest pneumothorax.
A-lines are artifacts reflecting off the parietal pleura that appear as equally spaced, hyperechoic horizontal lines. These are present in pneumothoraces, but not visible when B-lines are present.
The so called “lung point sign” is created by the intermittent contact between the lung and the chest wall in the setting of pneumothorax. Although it lacks some sensitivity (66%), it is 100% specific for pneumothorax when present on ultrasonographic examination. Negative predictive values for lung sliding and comet tail artifacts approach 100% for each finding. Sensitivity and specificity of the combined finding of absent lung sliding with present. A-lines is 95% and 94%, respectively.
Simple pneumothoraces that are small on chest radiographs can likely be managed conservatively. Kong and coworkers reported on the outcomes of 125 patients with pneumothoraces from stab wounds that measured less than 2 cm on chest radiographs among those, only 3% required chest tube placement, and larger enlarging or symptomatic pneumothoraces should be managed with tube thoracostomy.
Size of the chest tube is an area of ongoing research study done by Inaba showed that smaller chest tubes 28F or 32F were just as effective as larger tubes 36-F or 40-F in evacuating pneumothoraces. A recent, small, randomized clinical trial demonstrated that 14-F chest tubes were equivalent to 28-F chest tubes in terms of success in pneumothorax evacuation and insertion-related complications.
Open pneumothorax requires immediate treatment in the prehospital setting. An occlusive dressing secured on 3 sides is the preferred initial treatment for this injury. In the prehospital setting, this may require the addition of needle decompression if tension physiology develops after the dressing is applied. In the emergency department, a chest tube should be placed away from the soft tissue defect and operative repair of the soft tissue defect is required to reestablish the intrathoracic pressure gradients necessary for ventilation.
Tension pneumothorax causes a threat to life because of the progressive build up of air within the pleural cavity, caused by one way leak from a lacerated lung, airway or a chest wall. Air enters the pleural space on inspiration, but cannot be evacuated during expiration due to the functioning of oneway flap valve. This creates progressive accumulation of air with collapse of the ipsilateral lung, causing severe hypoxia, shift of the mediastinum to the opposite side, compression of the contralateral lung with atelectasis and decreasing venous return to the heart.
The combination of hypoxia, impaired ventilation and critically reduced cardiac output leads to traumatic cardiac arrest unless the tension is decompressed. Tension pneumothorax can complicate both penetrating and blunt trauma. It may be also induced iatrogenically during the insertion of central venous lines or by the incorrect application of occlusive dressings to penetrating chest wall wounds.
It should be remembered that tension pneumothorax might occur in patients with a simple pneumothorax who have been kept on positive pressure ventilation. Early identification and treatment are the key to effective management. Diagnosis of a tension pneumothorax should base on physical examination, and radiological examination is rarely performed. The classic signs are connected with decreased or lack of breath sounds and hyper resonant percussion note on the ipsilateral side, tracheal and cardiac deviation to the contralateral side, reduced chest movements, elevated venous pressure, progressive tachycardia, hypotension with pulsus paradoxus. When treatment is delayed the condition might leads to full circulatory collapse and cardiac arrest with Pulseless Electrical Activity (PEA). In rare cases tension pneumothorax may be bilateral.
Tension pneumothorax is the most frequent reversible cause of death during resuscitation of patients in traumatic cardiac arrest. In a dying patient immediate decompression should be done on the affected side, converting tension pneumothorax into an open pneumothorax or simple pneumothorax. In emergency the decompression is achieved by insertion of a large bore cannula into the fifth intercostal space in the anterior axillary line. The hiss of air usually confirms decompression and clinical improvement should be noticed. The cannula should be left open (resulting in an open pneumothorax) and the next step is to insert a chest tube, followed by reexamination of the chest and an AP chest radiograph. It must be remembered that a needle thoracostomy can easily become kinked or displaced, allowing the tension pneumothorax to recur. Hemothorax is another cause of death commonly occurs due to bleeding Intercostal and internal mammary vessels a, hemithorax can hold up to 3l of blood. It is estimated that approximately 50% of patients with hilar, great vessel or cardiac wounds die immediately after the injury, while about 25% survive for about 5-6 minutes before arrival to the hospital and remaining 25% might arrive at the hospital and require immediate diagnosis and surgical treatment. Patients with massive haemothorax can be diagnosed by presence of shock, respiratory insufficiency and deviation of the mediastinum. Patients in shock and with respiratory insufficiency must be intubated with no delay and chest radiogram may confirm the amount of blood loss.
A chest tube should be inserted in order to relieve the threat of ventilatory embarrassment. The main objective in the treatment of massive haemothorax is to restore blood volume, treating actively shock together with drainage of the haemothorax by inserting tube thoracotomy. The proper placement of a chest tube allows for effective evacuation of the blood. However, if initial drainage of blood is >1500 ml or ongoing drainage is >200 ml/h for about 4 or more hours, then thoracotomy in the surgical theatre is required? Ongoing bleeding, patient’s clinical status and requirement for blood transfusion are important parameters that should be taken into consideration deciding about the need for the thoracotomy. In the operated patients major vessels, intercostal arteries, injury to the hilum of the lung or to the myocardium are the main sources of massive bleeding. These injuries should be treated by oversewing the lesion to make sure that bleeding is controlled. Some patients might require resection of the lung segment or lobe and sometimes pneumonectomy when necessary.
The flail chest is an uncommon lesion that usually occurs with a high speed vehicle accident. It is commonly characterized by three or more rib fractures in two or more sites, with or without sternal lesion where the injured segment of the thoracic wall show paradoxical respiratory movement, mechanical respiratory dysfunction, and frequent respiratory failure.
When the chest wall loses its bony stability within thoracic cage, it becomes flail and starts to move in the direction opposite to the stable chest wall during inspiration and expiration (paradoxical). In many patients multiple rib fractures are accompanied by significant blood loss and lung contusion. Diagnosis of flail chest is based on clinical examination, in patients with flail chest, severe pulmonary contusion contributes to respiratory insufficiency. About 75% frail chest patients are associated with pulmonary contusion, which produces an inflammatory response with right to left shunts, resulting in severe hypoxia and severe pulmonary restriction.
Treatment is usually initiated with high flow oxygen and lung expansion by intermittent positive pressure ventilation. Intercostal chest tubes are almost always necessary, particularly if positive pressure ventilation is needed. In cases with respiratory distress and hypoxia due to the flail segment, endotracheal intubation and mechanical ventilation are necessary, particularly in patients with large pulmonary contusion.
The aim of further management is to preserve respiratory function. In all patients effective pain relief is required, in some cases epidural anaesthesia may be very effective. Careful fluid management is indicated because injured lungs are extremely sensitive to inadequate perfusion and to fluid overload.
Surgical fixation in costal fractures continue to be controversial Bottlang et al used anatomic plates and intramedullary splints in patients with severe damage level of with broken ribs with good results. In study patients reached an 84% force vital capacity at three months and 50% returned to work at six months.
A systematic review and metaanalysis which included a total of 538 patients compared the results of non-surgical and surgical treatment. The latter treatment was associated with less time on mechanical ventilation support, less pneumonias, less tracheostomies, and a lower mortality rate. A similar study with 753 patients shared similar results, suggesting that the surgical fixation of rib fractures have significant benefits. This study suggested that the surgical fixation of the fractured ribs could lead to significant benefits.
Cardiac lesion is a life-threatening injury if is not diagnosed and intervened surgically immediately, there are three types of injuries of the heart, which might include rupture, contusion and tamponade. Patients with myocardial rupture, usually the right atrium or ventricle rarely reach the hospital alive. The rupture of the left ventricle is rare and is associated with blunt chest trauma and may be mistaken for aortic injury. Myocardial contusion is a tolerable injury, manifested by chest pain in about 50% of cases and may be associated with sternal fracture. There are pleural rub, murmurs and evidence of low cardiac output. Usually there are arrhythmias such as ventricular fibrillation, atrial fibrillation. If the ECG shows ST elevation, it is mandatory to perform a coronary angiography. When this injury is suspected CPK and troponin must be requested. If heart failure signs are present it is necessary to use inotropes, intravenous fluids and keep the patient in the intensive care unit. The tamponade is associated with penetrating trauma of the chest, if the diagnosis is not made immediately most of these patients do not survive their arrival to the emergency room. With only 100 of blood contained in the pericardial sac, it is enough to cause heart failure, and in about 10% may have Beck triad and Kusmaul sign.
Diagnosis must be suspected by simple chest X-ray and confirmed with an ultrasound or ECHO. ECG shows low voltage complex and electrical alternans. Treatment must be immediate with pericardiocentesis and sometimes an urgent thoracotomy is needed, CPR is usually ineffective in tamponade cases. In patients with suspected cardiac injury and who are hemodynamically stable, chest CT is recommended, which has high diagnostic significance. Pulmonary contusion usually occurs together with chest wall injury. The contused lung is often damaged and unable to participate in the gas exchange of respiration. If Condition is huge and associated with frail chest can result to respiratory distress. There are few clinical signs of pulmonary contusion, chest radiographs and CT scanning are the 2 methods of diagnosing pulmonary contusions. Appearance of pulmonary contusion on chest radiographs is often delayed. CT scanning has proven to be a more accurate method for diagnosing pulmonary contusions. In a study by Miller and colleagues, CT scans identified 100% of pulmonary contusions compared with just 38% identified by chest radiographs. Rodriguez and coworkers noted in a study of more than 1000 patients with pulmonary contusion that more than 73% of contusions were seen only on CT imaging. In addition to early diagnosis, CT imaging can also determine the total contused lung volume. The treatment of pulmonary contusion is supportive and consist of oxygen therapy, pulmonary toilet, fluid restriction, pain management, and appropriate diuresis. The use of antibiotics and intubation have not been adviced unless otherwise indicated. Surgical intervention can be indicated in penetrating trauma with blunt pulmonary contusion, and lobectomy can be indicated in case of severe contused pulmonary contusion with large regions of necrosis. Diaphragmatic injuries commonly occur following thoracic compression and violent abdominal injury. The diaphragm normally rises to the fifth intercostal space during normal expiration, so that any patient after midtorso trauma is at risk for diaphragmatic rupture. The left diaphragm is injured 6 times more frequently than the right one. Right-sided lesion may show only a raised hemidiaphragm whereas a left sided may show herniation of the stomach, spleen and intestines. Thoracoabdominal CT can be used for accurate diagnosis. All diaphragmatic ruptures should be repaired, if not repaired early might present later, with dangerous incarceration of the small bowel, colon or momentum into the hernial defect. Acute repair may be accomplished via laparotomy or thoracotomy. The preferred surgical closure of diaphragmatic ruptures is based on interrupted sutures. In large defects synthetic prosthetic material or flaps should be used. Common cause of oesophageal injuries is penetrating trauma. The diagnosis is also probable in patients after blunt trauma with pneumothorax or haemothorax in the absence of rib fractures. On chest X-ray patients may present with posterior mediastinitis with fever, pain and persistent pneumothorax. Once diagnosed, posterolateral thoracotomy and routine surgical closure should be performed. Injuries to the oesophagus should be surgically repaired if the injury is less than 6 hours old. It is important to put the sutures in situ in order to avoid damage to the vasculature of the oesophagus. In older oesophageal injuries wide drainage with chest tubes, diverting oesophagostomy and nutritional support by feeding gastrostomy may provide the optimal management. Major tracheobronchial injury is uncommon and when occurs is associated with 80% mortality in the field. Penetrating tracheal injury is often cervical in location and easily detected. In contrast, most tracheobronchial injury caused from blunt trauma is near the carina, and can be more difficult to diagnose. Patient may demonstrate dyspnea, dysphonia, pneumomediastinum, pneumothorax, or subcutaneous emphysema. Although these signs can also be attributed to other pathologic conditions, together these findings should raise suspicion for tracheobronchial tree injury. Initial diagnostic studies should include CT scan to evaluate for mediastinal hematoma, pneumomediastinum, or tracheal deviation. However a negative study does not obviate bronchoscopy if tracheobronchial trauma is suspected. If injury is discovered, treatment depends on the severity. Nonoperative management is appropriate for injuries less than 4 cm, with viable airway tissue and an absence of associated esophageal damage or respiratory compromise.
For those injuries that do not meet nonoperative criteria, surgical intervention depends on location and extent of disruption. The proximal two-thirds of the tracheobronchial tree can be approached via a low collar incision, which can be extended through the manubrium for improved distal access. The distal third of the trachea and the intramediastinal mainstem bronchi, on the other hand, are more easily exposed by right posterolateral thoracotomy.
Simple lacerations can be repaired directly with interrupted absorbable sutures. Larger defects, however, may require pedicle flap closure from the pericardium, parietal pleura, intercostal muscles, or infrahyoid muscles. To further protect the newly repaired tracheobronchial tree, some surgeons use a guardian stitch, or stitch from the chin to the chest, to ensure neck flexion and, therefore, decreased tracheal tension for the first postoperative week.
Conclusion
Severe traumatic injury sounds to have high mortality when management is delayed and improperly provided to our clients. We can be able to salvage significant number of injured patients if only the protocol for the advanced trauma life support is properly followed once traumatic case arrive at our emergence centers. Definitive surgical care should be conducted when the patient is stable aiming to prevent multiple organ dysfunction and failure.
Acknowledgement
I would like to dedicate this written job to my wife Martha mbelle and my lovely children gladness, genevive and brian. They gave me Innermost moral and pychological support during hardship and critical situations. I would like to thank you my colleague doctors from department of general surgery and orthopedic for their proximity, generosity and kindness, because they acted immediately to help and save the life of this patient, I would not be fair without mentioning their names and those were dr peleus kato (mmed surg), dr samweli john (mmed orthopedic), dr mponda Baraka (mmed orthopedic), dr maleko Andrew (mmed general surg). Lastly my appreciation and thanks should be sounded to my hospital director (Dr Ibenze Ernest) and to all nursing staff members working in Dodoma main theatre, orthopedics and general surgery.
References
- Park K. Accidents In Textbook of Social and Preventive Medicine. 17th ed. Banarsidas Bhanot, Jabalpur, India. 2002;1-630.
- Miller DL, Mansour KA. Blunt traumatic chest injuries. Thorac Surg Clin. 2007;17:57-61. [Crossref] [Google Scholar] [PubMed]
- Frohlich M, Lefering R, Probst C, Paffrath T, Schneider MM. Epidemiology and risk factors of multiple-organ failure after multiple trauma: An analysis of 31,154 patients from the Trauma Register DGU. J Trauma Acute Care Surg. 2014;76:921-927. [Crossref] [Google Scholar] [PubMed]
- Tache S, Mbembati N, Marshall N, Tendick F, Mkony C, O’Sullivan P. Addressing gaps in surgical skills training by means of low-cost simulation at Muhimbili University in Tanzania. Hum Resour Health. 2009;7:64. [Crossref] [Google Scholar] [PubMed]
- Boateng KF, Amoati ABG. Chest injuries in Ghana. West Afr J Med. 2000; 19:175.
- Flagel BT, Luchette FA, Reed RL. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005;138:717-723. [Crossref] [Google Scholar] [PubMed]
- Bulger EM, Arneson MA, Mock CN. Rib fractures in the elderly. J Trauma. 2000;48:1040-1046. [Crossref] [Google Scholar] [PubMed]
- Brasel KJ, Guse CE, Layde P. Rib fractures: Relationship with pneumonia and mortality. Crit Care Med. 2006;34:1642-16426. [Crossref] [Google Scholar] [PubMed]
- Bergeron E, Lavoie A, Clas D. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54:478-485. [Crossref] [Google Scholar] [PubMed]
- Holcomb JB, McMullin NR, Kozar RA. Morbidity from rib fractures in-creases after age 45. J Am Coll Surg. 2003;196:549-555. [Crossref] [Google Scholar] [PubMed]
- Berg RJ, Karamanos E, Inaba K, Okoye O, Teixeira PG, Demetriades D. The persistent diagnostic challenge of thoracoab-dominal stab wounds. J Trauma Acute Care Surg. 2014;76:418-423. [Crossref] [Google Scholar] [PubMed]
- Ludwig C, Koryllos A. Management of chest trauma. J Thorac Dis. 2017;9:172–177. [Crossref] [Google Scholar] [PubMed]
- Zhang S, Tang M, Ma J, Yang J, Qin X, Jin W, et al. Thoracic trauma–a descriptive review of 4168 consecutive cases in East China. Medicine (Baltimore). 2019;98:14993. [Crossref] [Google Scholar] [PubMed]
- Mistry N, Bleetman A, Roberts KJ. Chest decompression during the resuscitation of patients in prehospital traumatic cardiac arrest. Emerg Med J. 2009; 26:738-740. [Crossref] [Google Scholar] [PubMed]
- Subcommittee A, Tchorz KM, Group IAW. Advanced trauma life support (ATLS®): The ninth edition. J Trauma Acute Care Surg. 2013;74:1363. [Crossref] [Google Scholar] [PubMed]
- Saillant NN, Sein V. Management of severe chest wall trauma. J Emerg Crit Care Med. 2018;2:41-48. [Crossref] [Google Scholar] [PubMed]
- Leech C. Whole body computed tomography for trauma: Friend or foe? Emerg Med J. 2017;34:635-636. [Crossref] [Google Scholar] [PubMed]
- Wagner SH, Biberthaler P, Haberle S, Wierer M, Dobritz M, Rummeny E, et al. Whole- Body CT in Haemodynamically Unstable Severely Injured Patients – A Retrospective, Multicentre Study. PLoS One. 2013;8:e68880. [Crossref] [Google Scholar] [PubMed]
- Platz JJ, Fabricant L, Norotsky M. Thoracic Trauma. Surg Clin North Am. 2017;97:783-799. [Crossref] [Google Scholar] [PubMed]
- Phillips B, Turco L, Mirzaie M, Fernandez C. Trauma pneumonectomy: A narrative review. Int J Surg. 2017;46:71-74. [Crossref] [Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.