Maternal and Fetal Effect of Misgav Ladach Cesarean Section in Nigerian Women: A Randomized Control Study
- *Corresponding Author:
- Dr. Oliver C Ezechi
P.O. Box 488, Surulere Lagos, Nigeria.
E-mail: oezechi@yahoo.co.uk
Citation: Ezechi OC, Ezeobi PM, Gab-Okafor CV, Edet A, Nwokoro CA, Akinlade A. Maternal and fetal effect of misgav ladach cesarean section in Nigerian Women: A randomized control study. Ann Med Health Sci Res 2013;3:577-82.
Abstract
Background: The poor utilisation of the Misgav-Ladach (ML) caesarean section method in our environment despite its proven advantage has been attributed to several factors including its non-evaluation. A well designed and conducted trial is needed to provide evidence to convince clinician of its advantage over Pfannenstiel based methods. Aim: To evaluate the outcome of ML based caesarean section among Nigerian women. Subjects and Methods: Randomised controlled open label study of 323 women undergoing primary caesarean section in Lagos Nigeria. The women were randomised to either ML method or Pfannenstiel based (PB) caesarean section technique using computer generated random numbers. Results: The mean duration of surgery (P < 0.001), time to first bowel motion (P = 0.01) and ambulation (P < 0.001) were significantly shorter in the ML group compared to PB group. Postoperative anaemia (P < 0.01), analgesic needs (P = 0.02), extra suture use, estimated blood loss (P < 0.01) and post-operative complications (P = 0.001) were significantly lower in the ML group compared to PB group. Though the mean hospital stay was shorter (5.8 days) in the ML group as against 6.0 days, the difference was not significant statistically (P = 0.17). Of the fetal outcome measures compared, it was only in the fetal extraction time that there was significant difference between the two groups (P = 0.001). The mean fetal extraction time was 162 sec in ML group compared to 273 sec in the PB group. Conclusions: This study confirmed the already established benefit of ML techniques in Nigerian women, as it relates to the postoperative outcomes, duration of surgery, and fetal extraction time. The technique is recommended to clinicians as its superior maternal and fetal outcome and cost saving advantage makes it appropriate for use in poor resource setting.
Keywords
Cesarean section, Maternal and neonatal morbidity, Misgav Ladach
Introduction
Cesarean section is the most common intraperitoneal surgical procedure in obstetric practice; accounting for about 10-35% of all deliveries.[1?4] Over the years there has been a wider recognition of the desire to reduce cesarean section related morbidity and mortality through the modification of some steps of the procedure.[5,6] The Pfannenstiel based (PB) cesarean section technique has been widely accepted and used despite lack of evidence establishing its advantage over order techniques.[6?9] Given that the operation is conducted so frequently, any attempt to reduce risks associated with it (even with relatively modest alterations in the surgical procedure for a particular outcome) is likely to yield significant benefits in terms of costs and better health outcomes for women.[10,11]
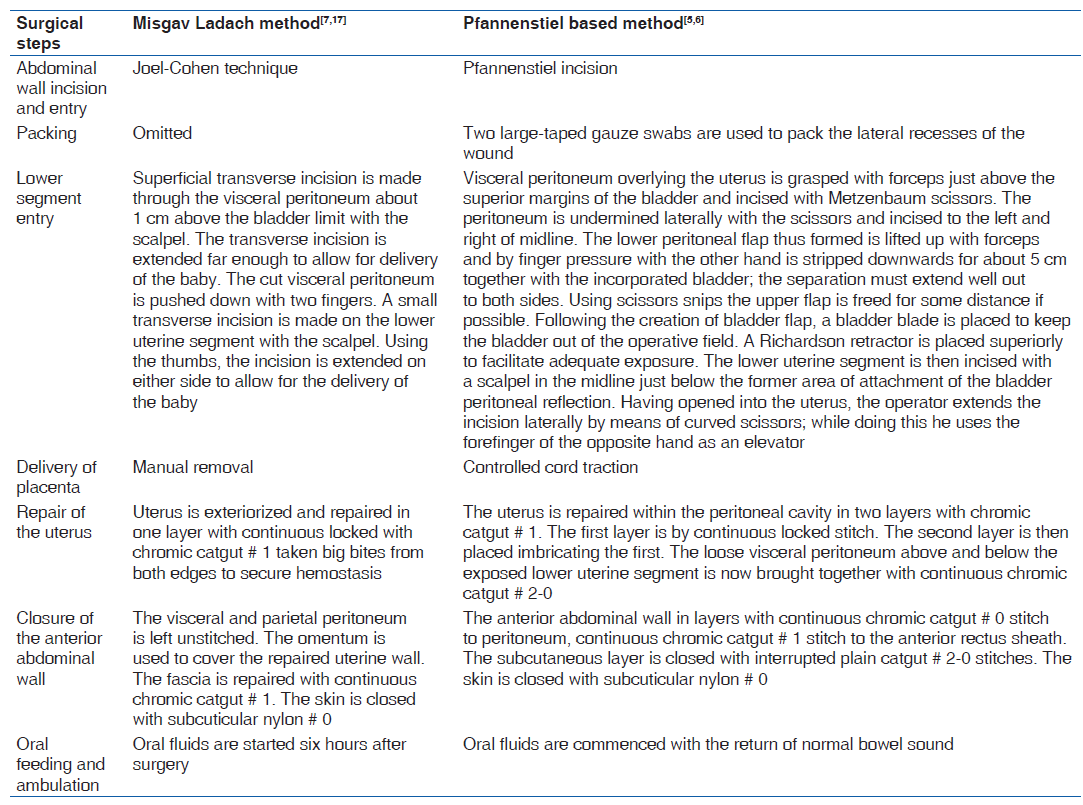
Michael Stark of Misgav Ladach hospital in Jerusalem introduced a novel technique of cesarean section by putting together modification of the various steps in traditional cesarean section.[7,12?15] This new technique was the result of a critical analysis of each surgical step in order to obtain an essentially less traumatic, easy, and quick to perform operation.[5,16] The new technique is now referred to as Misgav Ladach (ML) cesarean section.[17,18]
Meta?analysis of several randomized controlled trials comparing the ML technique, PB technique and lower midline techniques by two Cochrane reviews showed that ML technique is associated with shorter operating time, shorter time from skin incision to birth of baby, less blood loss, fewer analgesic injections, shorter time to oral intake postoperatively, and less fever.[19]
While it is tempting to adopt ML technique in our setting based on the above reviews without further evaluation, it should be noted that all the previous studies comparing the technique were in women from other race and settings.[7,12?15] In our setting unlike in Europe and North America, pelvic infection, adhesions, and uterine fibroid are common findings which may influence the outcome of the ML?based technique.[1]
In addition, the relative tensile strength of the tissues of the Negroid woman and surgical skill of junior obstetric staff on call when most of the cesarean section cases occur may influence the outcome.[1] A more pragmatic way will be to evaluate the ML technique in the new setting. This may also be the reason for its limited application among obstetricians.[5]
This study was, therefore, designed to determine the effect of the ML technique on maternal and infant outcome of operation time, blood loss, wound healing, analgesic use, fetal extraction time, Apgar score, neonatal admission, and deaths among Nigerian women.
Subjects and Methods
The study was conducted in two multidisciplinary proprietary hospitals in Lagos Nigeria over a 48?month period (January 2003-December 2008). Approval from the study was obtained from the research committees of the hospitals which also double as ethics committee. All consenting patients undergoing primary cesarean section in the hospitals that met the inclusion criteria during this period were enrolled into the study. They were randomized into either of two arms of Misgav Ladach method of cesarean section (ML) and Pfannenstiel based Cesarean section method (PB) using computer?generated random numbers. Randomization was hospital based and performed once the decision was made to deliver by cesarean section. Excluded from the study were cases of antepartum hemorrhage, prolonged obstructed labor, chorioamnionitis, preoperative hemoglobin less than 10 g/dl, prolonged premature rupture of membrane and clinically palpable uterine fibroid because the research committees of both hospitals gave their exclusion as condition for approval. Blood loss estimation was by visual inspection by the attending anesthetists. Only surgeons trained and experienced in the two techniques participated in the study.
Sample size
The sample size expression n = 1/d2 × Z2pq was used to determine the minimum number of subjects to be included in each arm of the study; where Z is the value of the Z score corresponding to the level of confidence; P is the estimated proportion of participants with any unfavorable outcome, q = 1 − p and d is the tolerable error margin in our estimate. At 95% level of confidence, Z = 1.96 and P = 0.10, and error margin of 5%, a sample size of 138 was determined. We increased the sample size to at least 152 during the study period in anticipation of nonresponse or withdrawal of consent and the fact that we expected at least 10% of the total sample size in any cell generated in contingency tables. In all 323 women were recruited from the two sites.
Operative technique
Common postoperative procedures
Oxytocics were administered after delivery of baby and placenta in all cases and continued for at least six hours postsurgery. Wound dressing were removed on the third postoperative day, and stitches removed on the fifth postoperative day. The urinary catheter was removed on first postoperative day except otherwise stated by the attending surgeon. Extended prophylactic antibiotics of Clauvinic acid potentiated amoxicillin and Metronidazole were used in all cases. Pentazocine 30 mg 6 h were given to all women for the first 24 h and thereafter on request. Pentazocine was replaced with cap ibuprofen for four days.
Data collection
Information on age, weight at delivery, height, parity, gestational age at delivery, indications for surgery, operation time, fetal extraction time, blood loss (estimate of the attending Anesthetists), postoperative analgesia requirements, number of extra sutures used, blood transfusion, postoperative anemia, puerperal morbidities, duration of hospital stay, time of bowel motion and ambulation after surgery, neonatal outcome, and any other postoperative complication observed were collected prospectively and entered into case report form designed for the study.
Data analysis
The information collected on the case report forms were entered and analyzed using excel enhanced with Megstat. Comparisons were made between the two groups using Chi square with Yates corrections, Fischer’s exact test and student’s t?test as appropriate. The odd risk ratio at 95% confidence interval was obtained was appropriate. A P value < 0.05 was considered significant.
Case definitions
Postoperative morbidity
The occurrence of one or more of the following conditions: Wound infection, endometritis, febrile morbidity, postoperative anemia, blood transfusion, and urinary traction infection.
Wound infection
The presence of one or more of the following; seriosangious/ purulent discharge, induration, erythema, and/or pain and obvious wound dehiscence (partial or total).
Endometritis
The occurrence of at least two of the following; fever, soft and tender uterus, foul smelling lochia, cervical motion tenderness, and culture of pathogenic organism from the endocervical swab.
Febrile morbidity
The rise of temperature to 38°C on at least two occasions 4 h apart, excluding the first 24 h after surgery in the absence of known operative or nonoperative site infection.
Fetal extraction time
The total time elapsed between skin incisions and clamping of the umbilical cord.
Operation time
The total time elapsed between skin incision and the last skin stitch.
Prolonged hospital stay
Hospital stay greater than fifth postoperative day.
Results
During the period of study, 323 consenting women undergoing primary cesarean section in the two hospitals met the inclusion criteria and were thus randomized into either of the two arms. Though the ratio of case enrolled in the two hospitals was in the ratio 9:1 there were no statistically significant difference in characteristics of patients, indications for cesarean section and type of cesarean section (P = 0.23; 95% CI: 0.21-13.7). After randomization, four women randomized to ML group withdrew their consent and were thus excluded from the study. The groups’ allocation was thus 157 in the ML group and 162 in the PB group.
The sociodemographic characteristics of the women are shown in Table 1 and are comparable.
| Characteristics,type and reasonfor cesareansection | ML groupN=157(%) | PB groupN=162(%) | P value | 95%confidenceinterval |
|---|---|---|---|---|
| Mean maternal age | 27.9 (4.9) | 28.0 (5.4) | 0.75 | 0.91-1.19 |
| Parity | 1.4 (1.5) | 1.3 (1.6) | 0.14 | 0.02-1.23 |
| Mean parity | ||||
| 0-2 | 89 (56.7) | 93 (57.4) | ||
| 3-5 | 57 (36.3) | 57 (35.2) | 0.97 | 0.32-3.8 |
| ≥5 | 11 (7.0) | 12 (7.4) | ||
| Mean body mass | 24.5 (5.5) | 24.2 (4.4) | 0.48 | 0.54-4.5 |
| index | ||||
| Gestational age atdelivery | 38.0 (2.1) | 38.1 (2.0) | 0.13 | 0.12-5.7 |
| Type of anesthesia | ||||
| General | 101 (64.3) | 105 (64.8) | 0.98 | 0.60-1.59 |
| anesthesia | ||||
| Spinal anesthesia | 56 (35.7) | 57 (35.2) | ||
| Indications forcesarean section | ||||
| Cephalopelvic disproportion | 46 (29.3) | 48 (29.6) | 0.79 | 1.0-9.1 |
| Persistent fetaldistress | 19 (12.1) | 21 (13.0) | ||
| Abnormallie/malposition | 17 (10.8) | 13 (08.02) | ||
| Severe PIH | 27 (17.2) | 22 (13.6) | ||
| Bad obstetrichistory | 13 (08.3) | 19 (11.7) | ||
| IVF pregnancy | 26 (16.6) | 32 (19.8) | ||
| PMTCT | 9 (05.7) | 07 (04.3) | ||
| Type of procedure | ||||
| Emergency | 92 (58.6) | 91 (56.2) | 0.11 | 0.69-1.76 |
| Elective | 65 (41.4) | 71 (43.8) | ||
Table 1: Sociodemographic characteristics, type of anesthesia, and reasons for cesarean among the study groups
Table 2 shows the comparison of maternal outcome between the two groups. The mean duration of surgery in the ML group of 29.6 (7.5) min was significantly shorter than 37.4 (10.8) min in the PB group (P < 0.001; OR: 7.1; CI: 4.7-11.8). The estimated blood loss was also significantly lower in the ML group (553.6 mls) compared to 734.9 mls in the PB group (P < 0.01; OR: 5.1; CI: 4.3-7.7). The number of cases of postoperative anemia was significantly more in the PB group than in the ML group (P < 0.01; OR: 2.87; CI: 1.4-6.4). Although more women were transfused with blood in the PB group (5.3%) for postpartum hemorrhage compared to 2.0% in the ML group, the difference was not statistically significant (P = 0.38). The mean extra analgesic requirement by the women postsurgery was less in the ML group (2.3 (1.0)) compared to 3.1 (1.3) in the women in the PB group (P = 0.02). There was also statistically significant difference between the two groups with respect to the time of first bowel motion (P = 0.01; OR: 4.0; CI: 2.6-3.4) and the time of first mobilization (P < 0.001; OR: 6.2; CI: 4.7- 8.3). The mean time of first bowel motion was 26.2 (5.6) h in the ML group compared to 39.5 (9.4) h in the PB group. The mean postoperative time at mobilization was 22.5 (6.2) h in ML group as against 34.3 (8.9) h in than PB group. Eighteen (8.1%) women in the PB group had postoperative morbidities of anemia, wound infection, febrile morbidity, blood transfusion, and puerperal sepsis compared to seven (3.4%) women in ML group. The differences were statistically significant at P = 0.001 (OR: 3.3; CI: 1.6-6.8). The mean hospital stay was shorter (5.8 days) in the ML group as against 6.0 days; however, this difference was not significant statistically (P = 0.17).
| Outcome variable | ML group N=157 (%) | PB group N=162 (%) | P value | OR (95%) confidence interval | |||
|---|---|---|---|---|---|---|---|
| Mean operation time (minutes) | 29.6 (7.5) | 37.4 (10.8) | <0.001 | 7.1 | (4.7-11.8) | ||
| Estimated blood loss (mls) | 553.6 (259.5) | 734.9 (333.5) | 0.02 | 5.1 (4.3-7.7) | |||
| Extra stitch to control bleeding | |||||||
| Not required | 128(81.5) | 139 | (85.8) | 0.38 | 0.73 | (0.39-1.38) | |
| Required | 29 (18.5) | 23 (14.2) | |||||
| Women transfused | |||||||
| Not transfused | 149(94.9) | 151 | (93.2) | 0.69 | 1.69 | (0.49-3.82) | |
| Transfused | 8 (5.1) | 11 | (6.8) | ||||
| Hemoglobin levels postpartum | |||||||
| ≥10g/dl | 145(92.4) | 130 | (80.2) | 0.03 | 2.97 | (1.40-6.40) | |
| <10 g/dl | 12(7.6) | 32 (19.8) | |||||
| Mean time of first bowel motion (hours) | 26.5 (4.2) | 34.5 (6.7) | 0.01 | 4.0 | (2.6-13.4) | ||
| Mean postoperative mobilization time (hours) | 22.5 (5.2) | 34.3 (7.6) | <0.001 | 6.2 (4.7-8.3) | |||
| Postoperative morbidities | |||||||
| No | 144(91.7) | 125 | (77.2) | ||||
| Yes | 13(8.2) | 37 (22.8) | 0.001 | 3.28 | (1.60-6.83) | ||
| Mean hospital stay | 5.3 (1.2) | 5.9 (1.9) | 0.14 | 0.58 | (0.19-1.35) | ||
Table 2: Comparison of maternal outcome in the two groups
Table 3 showed the neonatal outcome in the two groups. It was only in the fetal extraction time that there was a statistically significant difference between the two groups (P = 0.001). The mean fetal extraction time was 162 s in ML group compared to 273 s in the PB group (CI: 2.7-7.8). The other parameters compared were number of babies with Apgar score less than 7 at 1 min, neonatal admission and neonatal death.
| Outcomevariable | ML groupN=157(%) | PB groupN=162(%) | P value | OR (95%confidenceinterval) | |
|---|---|---|---|---|---|
| Mean fetalextraction time(minutes) | 162 (5.1) | 273 (7.1) | 0.001 | 3.1 (2.7-7.8) | |
| Apgar score at1 min | |||||
| Greater orequal to 7 | 128 (81.5) | 139 | (85.8) | 0.38 | 0.73 (0.39-1.38) |
| Less than 7 | 29 (18.5) | 23 (14.2) | |||
| Neonatal admission | |||||
| Admitted | 149 (94.9) | 151 | (93.2) | 0.69 | 1.69 (0.49-3.82) |
| Not admitted | 8 (5.1) | 11 | (6.8) | ||
| Neonatal death | |||||
| Yes | 148 (94.4) | 154 | (95.1) | 0.95 | 0.85 (0.29-2.49) |
| No | 9 (7.6) | 8 (4.9) | |||
Table 3: Comparison of fetal outcome in the two groups
Discussion
Our study evaluate the maternal and short?term fetal outcome of two cesarean techniques of Misgav Ladach and Pfannenstiel based methods, with aim of proving the reported advantage of ML technique among Nigerian women. We were able to show the advantage of ML technique over PB technique in operation time, blood loss, hemoglobin levels postsurgery, time to first bowel motion, ambulation time, and postoperative morbidity like previous study in Refs. 13, 15, and 17. The mean operation time (P < 0.001), estimated blood loss (P = 0.002), time to first bowel motion (P = 0.01), and mean postoperative mobilization time (P < 0.001) were significantly shorter among the ML arm compared to PB arm. Also among the ML arm, the rate of postoperative morbidity of 8.2% was signifantly lower than rate 22.8% among the PB arm (P = 0.001). However, no difference was found between the techniques as it relates to the number of women that were transfused (P = 0.69), requiring extra stitch to control bleeding (P = 0.38), or stayed more than six days in the hospital (P = 0.14).
The finding above confirms the theoretical basis of Misgav Ladach technique of close relation between tissue trauma and morbidity and supports the assertion that the introduction of ML technique removes the unnecessary step in PB technique including the reduction of CS related morbidity.[7,13,15,17] Every unnecessary surgical step increases tissue damage and inflammatory response, with a consequent rise in hemorrhage and infection risk.[7] This study in addition excludes any expected effect of race and environment on the outcome of the new technique.
Among the fetal outcome parameters of mean fetal extraction time, Apgar score, neonatal admission, and death rates evaluated in the study, it was only in fetal extraction time that ML technique was found to confer significant advantage over PB technique. The mean fetal extraction time of 162 (5.1) s among the ML group was significantly lower than 273 (7.1) s in the PB group (P = 0.001; CI: 2.7–7.8). This finding supports the previous reports by Darj,[7] Ferrari,[16] and Franchi[9] which reported short fetal extraction time in ML technique compared to PB technique. Our study further confirms the conclusion of Carlo Dani and colleague who stated that though ML technique shortens fetal extraction time, it does not influence short?term outcome of the newborn infants.[13] It is therefore reasonable to believe that neonatal outcome depends more on other factors such as chronic hypoxia, delayed decision to intervention interval and pre?existing condition, than on the cesarean section.[9,20]
This study has shown the superiority of ML technique over PB techniques in Nigerian women like their counterparts elsewhere and is therefore recommended for routine cesarean section both for emergency and elective cases. Though this study was a randomized control study which provides grade A evidence, it has some limitation that may impact on its external validity. The restriction of the study sites to Lagos and the exclusion of complicated cases as requested by the research committees make its generalizability difficult. When these limitations are viewed within the context and aim of the study, which is to evaluate what, is already established in other climes, the limitations are, therefore, not enough to invalidate the study. However, more evaluation of the techniques in the other zones of Nigeria and in high risk case is recommended.
Conclusion
This study has confirmed the already established benefit of ML techniques in Nigerian women as it relates to the postoperative outcomes, duration of surgery, and fetal extraction time. It is therefore recommended to clinicans as its superior maternal and fetal outcome and cost saving advantage makes it appropriate for use in low resource setting like ours.
References
- Ezechi OC, Nwokoro CA, Kalu BKE, Njokanma OF, Okeke GC. Caesarean morbidity and mortality in a private hospital in Lagos, Nigeria. Trop J Obstet Gynaecol 2002;19:97?100.
- Adeleye JA. Primary elective caesarean section in Ibadan, Nigeria. Int Surg 1977;62:97?9.
- Onifade A. Primary elective caesarean section in multipara. Nigeria Medical Journal 1971;19:30?3.
- Pawlowicz P, Wilczy’nski Jan, Stetkiewicz T. Comparative analysis of modification of Misgav?Ladach and Pfannenstiel methods for caesarean section in the Department of Feto?Maternal Medicine, Polish Mother’s Memorial Hospital, between 1994 and 1999. Singapore J Obstet Gynaecol 2001;32:29?33.
- Ezechi OC, Nwokoro CA, Kalu BK, Njokanma OF, Okeke GC. Evaluation of a novel Caesarean section technique among Nigeria women. Paper presented at the Annual conference of The Society of Obstetrics and Gynaecology of Nigerian 2001, Port Harcourt, Nigeria: 2001. p. 6.
- Kumar SA. Nonclosure of parietal and visceral peritoneum during caesarean section. Journal of Obstetrics and Gynecology of India 2003;53:153?7.
- Stark M. Technique of caesarean section: The Misgav Ladach method. In: Popkin DR, Peddle LJ, editors. Women’s health today: Perspectives on current research and clinical practice. Proc. XIV FIGO Congress Gynecol Obstet: Montreal. New York and London: Parthenon; 1994. p. 81?5.
- Lodh E, Bhattacharjee P. Single lever of caesarean section–A comparative study. Journal of Obstetrics and Gynecology of India 2002;52:36.
- Franchi M, Ghezzi F, Raio L, Naro ED, Milierina M, Agosti M, Bolis P. Joel?Cohen or Pfannenstiel incision at cesarean delivery: does it make a difference? Acta Obstet Gynecol Scand 2002;81:1040?6.
- Abalos E. Surgical techniques for caesarean section: RHL commentary. Geneva: The WHO Reproductive Health Library, World Health Organization; 2009.
- Stark M. Clinical evidence that suturing the peritoneum after laparotomy is unnecessary for healing. World J Surg 1993;17:419.
- Dani C, Reali MF, Olivetto R, Temporin G, Bertini G, Rubaltelli FF. Short?term outcome of newborn infants born by a modified procedure of cesarean section: A prospective randomised study. Acta Obstet Gynecol Scand 1998;77:929?31.
- Stark M, Chavkin Y, Kupferstain C, Guedj P, Finkel AR. Evaluation of combinations of procedures in caesarean section. Int J Gynecol Obstet 1995;48:273?6.
- Stark M, Finkel AR. Comparison between the Joel?Cohen and Pfannenstiel incision in cesarean. Eur J Obstet Gynecol Reprod Biol 1994;53:121?2.
- Ferrari AG, Frigerio L, Candotti G, Origoni M, Mariani A,Petrone M. Modified stark procedure for caesarean. First
Italian experience. Int J Gynecol Obstet 1997;3:95?102. - Darj E, Nordstrom ML. The Misgav Ladach method of caesarean section compared to the Pfannenstiel method. Acta Obstet Gynecol Scand 1999;78:37?41.
- Holmgren G, Sjoholm L, Stark M. The Misgav Ladach method of caesarean section: Method description. Acta Obstet Gynecol Scand 1999;78:615?21.
- Hofmeyr GJ, Mathai M, Shah AN, Novikova N. Techniques for caesarean section. Cochrane Database Syst Rev 2008; CD004662.
- Mathai M, Hofmeyr GJ. Abdominal surgical incisions for caesarean section. Cochrane Database Syst Rev 2007; CD004453.
- Onwudiegwu U, Makinde ON, Ezechi OC, Adeyemi A. Decision?caesarean delivery interval in a Nigerian university hospital: Implications for maternal and mortality. J Obstet Gynaecol 1999;19:30?3.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.