Measurement of Blood-Loss During Hip Surgery
2 Department of Anesthesiology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences Sawangi (Meghe), Wardha, India
Published: 30-Jul-2021
Citation: Chaudhari A, Deshmukh P*, Sable P, Jejani A, Hakole V. Measurement of Blood-Loss during Hip Surgery. AMHSR. 2021;11:140-146
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
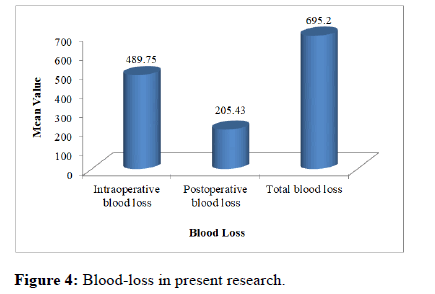
Background: One of the main problems for physicians is measuring bloodloss during surgery. Despite anesthesiologists and surgeons' understanding of the inaccuracy of visual estimation, it remains the foundation for estimating surgical blood-loss. The goal of this research was to estimate the blood-loss of patients having hip surgery. Method: Total 40 patients were enrolled. Total blood-loss was measured by determining intra-operative and post-operative blood-loss and adding them together. Pre-operatively and 24 hours after surgery, blood samples were collected from the patients to assess hemoglobin and hematocrit. The requirement of blood transfusion was noted. Results: The mean intra-operative, post-operative, and total bloodloss was 489.75±123.63ml, 205.43±63.31ml and 695.2±162.44ml respectively. Mean pre-operative and post-operative hemoglobin was 12.30±1.05 and 9.84±0.91 gm/dl respectively, thus drops in hemoglobin was by 2.46±0.14 gm/dl whereas mean pre-operative and post-operative hematocrit was 36.03±3.15% and 29.30±2.36% respectively. There was a drop in hematocrit by 6.73±0.79%. Out of 40, 15(37.5%) patients received blood transfusion postoperatively. Conclusion: In hip surgery most of the intra-operative and postoperative blood-loss occurs in the initial 24 hours of surgery. "Intra-operative blood-loss" and "transfusion rate" are not adequate predictors of total bloodloss.
Keywords
Blood-loss; Hip surgery; Intra-operative; Post-operative; Haemoglobin; Haematocrit; Transfusion
Introduction
Every year, over 313 million surgical operations are performed globally. [1] According to recent estimates, at least 4.2 million individuals die within 30 days following surgery each year, accounting for 7.7% of all fatalities worldwide. [2]
Perioperative bleeding is still a substantial concern during and after surgery, and it is linked to a high likelihood of mortality, complications, and healthcare resource utilization. [3,4]
Estimating intra-operative blood-loss is a routine problem for physicians, and no standardized approach has been utilized consistently until recently. Despite the fact that visual estimate is inaccurate, intra-operative blood-loss is still documented visually. [5]
However, measured blood-loss, coupled with other information such as haemoglobin levels and individual transfusion exacerbates, plays an important role in blood transfusion decisions. Inappropriate transfusion of blood products has hazards and has an impact on the patient's prognosis. [6]
Total hip arthroplasty (THA) is one of the most regular orthopaedic surgeries performed globally.
It can cause significant blood-loss, and up to 46% of patients require red blood cell (RBC) transfusions during or after surgery. [7,8]
Moreover, orthopaedic surgeries can cause significant bloodloss from the surgical field and drains as well as extravasation into tissues. [9]
Surgeons can expect total blood-loss of roughly 1 L during the perioperative phase for primary hip arthroplasty when obvious and concealed losses are included. [10]
Pre-operative anaemia is a prevalent disease in patients who undergo major surgery, with a meta-analysis revealing a 39.1% overall incidence rate. [11] Furthermore, pre-operative anaemia was found in roughly 25% of patients hospitalized for elective orthopaedic surgery. [12] Severe anaemia is linked to an increased risk of death and a higher need for RBC transfusions. The most prevalent kind of anaemia in patients having arthroplasty is iron deficiency anemia, which is related with a longer hospital stay, higher 90-day readmission rates, and a greater frequency of post-operative complications. [13] Furthermore, post-operative anemia might raise the risk of a coronary artery disease and slow recovery following joint replacement. [14] Allogeneic transfusion is also linked to post-operative problems such as surgical site infection. [15,16] Blood conservation techniques enhance perioperative outcomes while also lowering expenses. [17,18] The monitoring of intra-operative blood-loss is the first step in reducing blood-loss and enhancing patient care. As a result, the current research was designed to quantify bloodloss during hip surgery in patients who did not receive TXA or utilized a tourniquet using pre-operative and postoperative hemoglobin and hematocrit measurements.
Materials and Methods
After obtaining approval from the Institutional Ethical Committee and written informed consent from all the patients, this observational research was conducted in the Department of Anaesthesiology, Acharya Vinoba Bhave Rural Hospital (AVBRH) affiliated to Jawaharlal Nehru Medical College, Sawangi (M), Wardha, over a period of 2 years from August 2017 to October 2019. Total 40 patients of ASA status I and II, age between 20 years-60 years, weight 40 kg-70 kg, height 150 cm-185 cm, haemoglobin level >10gm%, normal prothrombin time or activated partial thromboplastin time and who scheduled to undergo hip surgeries where tourniquet is not used & done under subarachnoid block were included in the research. Patients with ASA status III and above, having age <20years or >60 years, weight <40kg or >70kg, height <150cm or >185cm, patient with haemoglobin level <10gm%, pre-operative hepatic or renal dysfunction, serious cardiac or respiratory disease or on thrombolytic agents, abnormal prothrombin time or activated partial thromboplastin time, history of thromboembolic disease were excluded from the research.
A night before surgery, all patients had a pre-anaesthetic checkup. A thorough general and systemic examination was done after obtaining a detailed history. A day before surgery, routine examinations, notably haemoglobin and haematocrit levels, were performed. Oral tab was used to premedicate the patients. The night before surgery, take 0.25 mg alprazolam and 20 mg tab Omeprazole. Patients were placed on NBM for 8 hours before to surgery. When the patient arrived in the operating room, a wide bore cannula was secured and ringer lactate was begun at a rate of 10ml/kg. Noninvasive Blood Pressure (NIBP), pulse oximeter, and Electrocardiogram (ECG) monitors were linked to the patient, and all baseline parameters such as Heart Rate (HR), Systolic (SBP) and Diastolic (DBP), Respiratory Rate (RR), and Oxygen Saturation (SpO2) were recorded before surgery. Hemodynamic parameters (HR, SBP, DBP, SpO2, and RR)were recorded shortly before to anaesthetic induction. Subarachnoid block with 3ml 0.5 percent hyperbaric Bupivacaine was used to anesthetize the patients. Cardiorespiratory parameters such as HR, DBP, SBP, RR, and SpO2 were thoroughly monitored for side effects of spinal anaesthesia such as hypotension, bradycardia, drop in oxygen saturation, and so on, and were noted every 5 minutes for the first 30 minutes and every 10 minutes until the end of surgery.
Complete hip replacement, total hip arthroplasty, dynamic hip screw, proximal femoral nail, core decompression, and bipolar hemiarthroplasty were all evaluated for the research. Throughout the surgery, blood-loss was measured every 10 minutes by monitoring the weight change of surgical swabs on a digital weighing scale and the volume in the suction reservoir, and this was deemed intra-operative blood-loss. Before shipping them for sterilization, the average weight of a dry gauze and mop was recorded. This was the case with all of the mops and gauze. Blood-loss was measured by subtracting the weight of the drenched mop and gauze from the weight of the dry mop and gauze. A 1gm increase in the weight of wet gauze and mop was judged to be the equivalent of 1ml of blood-loss. [19] Blood-loss in suction drains was estimated by deducting the amount of normal saline utilized for surgical site cleaning from the total output present in the suction. [20] If the intra-operative blood-loss exceeded 40% of the circulating blood volume, intra-operative blood transfusion was begun. In a 3:1 ratio, crystalloids (lactated ringer) were administered to restore the intra-operative blood volume lost. [21]
At the conclusion of the procedure, a vacuum drain was inserted at the surgical site for the following 24 hours. Until 24 hours following surgery, the volume of blood in the suction drain was utilized to monitor post-operative bloodloss. Patients were transferred to the post-operative care unit following surgery. The contents of the drain were measured and documented in the recovery room and post-operative ward until 24 hours after surgery. Total blood-loss was calculated by adding intra-operative and post-operative blood-loss. Routine noninvasive monitoring was performed on the 24th post-operative hour.
A blood sample was obtained from patient 24 hours after surgery to assess post-operative haemoglobin and hematocrit. A reduction in haemoglobin of more than 25% of the preoperative level was deemed a transfusion trigger. The number of patients who had blood transfusions and the quantity of units of blood transfused throughout the post-operative phase, which was 24 hours following surgery, were recorded. Post-operative pain was controlled with analgesic (injection tramadol 100mg i.v slowly in drip) that was provided on the patient's request since discomfort causes a rise in heart rate and blood pressure, which would have impacted postoperative blood-loss.
Statistical Analysis
All of the information was initially entered into Microsoft Excel 2010, and these spreadsheets were then utilized for analysis. The Statistical Package for Social Sciences (SPSS) 20.0 version and Graph Pad Prism 6.0 version were used in the analysis. The quantitative data was presented as Mean ± SD. The qualitative information was represented as a percentage.
Observation and Results
A total of 40 patients undergoing hip surgery were enrolled in the research. The maximum numbers of patients were in the age group of 41-50 years (27.5%) with male predominance. Most of the patients belonged to ASA class II as shown in table 1. The mean age of patients was 40.62 ± 11.29 years. Mean weight and height of the patients was 59.22 ± 6.44 kilograms and 168.55 ± 7.32 cm respectively. Mean duration of surgery was 113.15 ± 11.68 minutes [Table 1].
| Parameters | No. of Patients | Percentage | |
|---|---|---|---|
| Age group (Years) | 20-30 | 10 | 25 |
| 31-40 | 10 | 25 | |
| 41-50 | 11 | 27.5 | |
| 51-60 | 9 | 22.5 | |
| Gender | Male | 31 | 77.5 |
| Female | 9 | 22.5 | |
| ASA Class | Class I | 12 | 30 |
| Class II | 28 | 70 | |
| Weight (Kilogram) | 40-50 | 5 | 12.5 |
| 51-60 | 16 | 40 | |
| 61-70 | 19 | 47.5 | |
| Height (centimeter) | 150-160 | 7 | 17.5 |
| 161-170 | 16 | 40 | |
| 171-180 | 15 | 37.5 | |
| 181-190 | 2 | 5 | |
| Duration of surgery ( Minutes ) | 60-100 | 7 | 17.5 |
| 101-140 | 32 | 80 | |
| 141-180 | 1 | 2.5 | |
Table 1: Distribution of patients according to demographic data and duration of surgery.
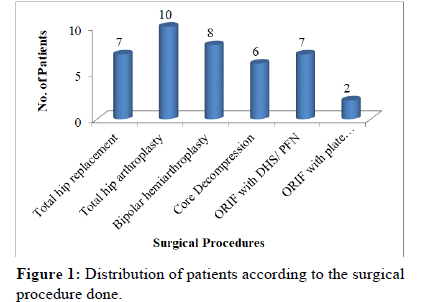
The maximum number of patients underwent total hip arthroplasty 8 (20%) and bipolar hemiarthroplsty 8 (20%) as depicted in [Figure 1].
The maximum patients 21 (52.5%) had hemoglobin levels between 10 gm-12 gm/dl whereas 36 (90%) had preoperative hematocrit level between 31%-40.9%.
However, maximum patients 15 (37.5%) had circulating blood volume level in the range of 4501- 5000 ml, [Table 2].
| Pre-operative parameters | No. of patients | Percentage | |
|---|---|---|---|
| Pre-operative Hemoglobin (gm/dl) | 10 gm/dl -12 gm/dl | 21 | 52.5 |
| 12.1 gm/dl -14 gm/dl | 16 | 40 | |
| 14.1 gm/dl -16 gm/dl | 3 | 7.5 | |
| Pre-operative hematocrit level | 31%- 40.9% | 36 | 90 |
| 41%- 50.9% | 4 | 10 | |
| 51%- 60.9% | 0 | 0 | |
| Circulating blood volume (ml) | 2501-3000 | 2 | 5 |
| 3001-3500 | 3 | 7.5 | |
| 3501-4000 | 6 | 15 | |
| 4001-4500 | 10 | 25 | |
| 4501-5000 | 15 | 37.5 | |
| 5001-5500 | 4 | 10 | |
Table 2: Pre-operative Hematological Parameters.
Mean circulating blood volume was 4325.37 ± 638.67 ml [Table 2].
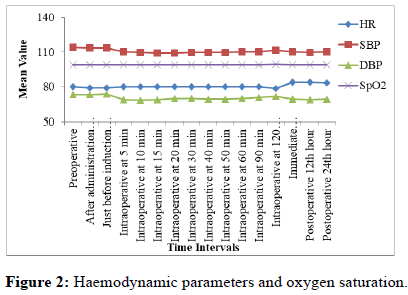
The mean heart rate (HR), diastolic blood pressure (DBP) and systolic blood pressure (SBP) found stable and no significant difference at different time intervals.
Depicting that the intravascular volume was adequately maintained with the help of crystalloid administration.
Oxygen saturation (SpO2) was maintained throughout the research period (pre-operatively, intra-operatively and postoperatively) as shown in [Figure 2].
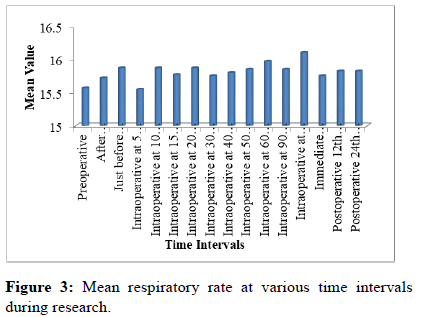
Respiratory rate was found to be normal throughout the research as depicted in [Figure 3].
The mean intra-operative blood-loss was 489.75±123.63 ml; mean post-operative blood-loss was 205.43±63.31 ml and mean total blood-loss was 695.2±162.44 ml [Figure 4].
The maximum number of patients 24 (60%) had postoperative hemoglobin in the range of 8.1-10 gm/dl whereas most of the patients (62.5%) had post-operative hematocrit level between 21% - 30.9 %, [Table 3].
| Parameters | No. of patients | Percentage | |
|---|---|---|---|
| Post-operative Hemoglobin (gm/dl) | 8.1- 10 | 24 | 60 |
| 10.1-12 | 16 | 40 | |
| 12.1-14 | - | - | |
| 14.1-16 | - | - | |
| Post-operative Hematocrit (%) | 21-30.9 | 25 | 62.5 |
| 31-40.9 | 15 | 37.5 | |
| 41-50.9 | - | - | |
Table 3: Distribution of patients according to post-operative hemoglobin and hematocrit.
Table 4 shows the drop in hemoglobin and hematocrit postoperatively from the pre-operative levels among research population. Out of 40 patients, 15 (37.5%) patients received blood transfusion post-operatively [Table 4].
| Parameters | Pre-operative | Post-operative | Drop from baseline |
|---|---|---|---|
| Haemoglobin (gm/dl) | 12.30±1.05 | 9.84±0.91 | 2.46 ±0.14 |
| Hematocrit (%) | 36.03±3.15 | 29.30 ± 2.36 | 6.73 ± 0.79 |
Table 4: Drop in haemoglobin and hematocrit post-operatively from the pre-operative levels among the patients.
Discussion
Major orthopedic surgeries over hip joints are associated with large amount of blood-loss. Amount of blood-loss determines the morbidity, mortality, duration of surgery, duration of hospital stay, the need to re-explore and most importantly the need for blood transfusion. [22] The current research evaluated perioperative blood-loss following hip surgery, finding the first post-operative 24 hours as the time during which roughly 90% of blood-loss occurs for all operations studied. Most of the patients were admitted with the history of trauma as trauma is common in age group of 41 years-50 years, so the maximum numbers of patients (27.5%) were in the age group of 41 years-50 years. As trauma is more common in males, therefore males outnumbered the females. Most patients were classed as ASA grade 2 as similar to Magill et al research. [23] Maximum number of patients underwent total hip arthroplasty 8 (20%) and bipolar hemiarthroplsty 8 (20%), this is supported by results of Thipparampall et al. [24] Mean duration of surgery was 113.15 ± 11.68 minutes which are comparable with the research done by Vijay. The mean pre-operative hemoglobin level was 12.30 ± 1.05 gm/dl and the mean hematocrit level was 36.03 ± 3.15%. This finding is in accordance with the research done by Thipparampall. However, the mean circulating blood volume was 4325.37 ± 638.67 ml.
The change in the mean heart rate from the baseline throughout our research was non-significant symbolizing that the intravascular volume irrespective of the blood-loss, was well managed with the help of I.V. crystalloids. Mean systolic and diastolic blood pressure at different time intervals was found to be stable, depicting that the intravascular volume was adequately maintained with the help of crystalloid administration. Since the blood-loss in current research was in the range of Class I of American College of Surgeon’s Classification of Acute Hemorrhage, therefore the blood pressure changes in our research are also justified by the same classification. Oxygen saturation was maintained throughout the research period (pre-operatively, intra-operatively and post-operatively) indicating that none of the patient developed oxygen saturation below 95%. Respiratory rate was found to be normal throughout the research as the blood-loss in present research was in the range of Class I of American College of Surgeon’s Classification of Acute Hemorrhage which shows normal respiratory rate of 14-20/min.
The mean intra-operative blood-loss was 489.75 ml ± 123.63 ml. None of the patient had an intra-operative blood-loss of more than 40% and as the loss was in the range of Class I of American College of Surgeon’s Classification of Acute Hemorrhage, [25] therefore no patient received intra-operative blood transfusion, thus complication associated with blood transfusion was not seen in our research. These findings agree with the findings, of Thipparampall. A number of related studies were reported. [26-29] Articles from GBD study were reviewed. [30-32]
Blood-loss during the post-operative period is believed to be a mix of ongoing bleeding and hyper fibrinolysis, and is sometimes referred to as "hidden loss" since it is not visible. The mean post-operative blood-loss was 205.43 ± 63.31 ml and mean total blood-loss was 695.2 ml ± 162.44 ml. Mean pre-operative and post-operative hemoglobin was 12.30 ± 1.05 and 9.84 gm/dl ± 0.91 gm/dl respectively, thus drops in hemoglobin by 2.46 ± 0.14 gm/dl whereas mean preoperative and post-operative hematocrit was 36.03 ± 3.15% and 29.30 ± 2.36% respectively. There was a drop in hematocrit by 6.73 ± 0.79%. This drop in hemoglobin and hematocrit can be attributed to significant amount of bloodloss. 15 (37.5%) patients received blood transfusion postoperatively.
Conclusion
In hip surgery most of the intra-operative and post-operative blood-loss occurs in the first 24 hours of surgery. "Intraoperative blood-loss" and "transfusion rate" are not adequate predictors of total blood-loss, so they should not be used to estimate the success of blood-loss assessment methods. The methods to reduce intra-operative & post-operative bloodloss are indicated. This will improve patient’s outcome and will reduce blood transfusion rate.
Limitations of the research
• Sample size needs to be increased to have further insights to make intra group comparison of blood-loss amongst different types of hip surgeries.
• To have uniformity of sample single type of surgery needs to be chosen.
References
- Meara JG, Leather AJ, Hagander L, Aikire BC, Alonson N, Ameh EA et al. Global Surgery 2030: Evidence and Solutions for achieving health, welfare, and economic development. Surgery. 2015;158:3-6.
- Nepogodiev D, Martin J, Biccard B, Makupe A, Bhangu A. National Institute for Health Research Global Health Research Unit on Global Surgery. Global burden of post-operative death. Lancet. 2019;393:401.
- Smilowitz NR, Oberweis BS, Nukala S, Rosenberg A, Zhao S, Xu J et al. Association between anemia, bleeding, and transfusion with long-term mortality following noncardiac surgery. Am J Med. 2016;129:315-323.
- Christensen MC, Dziewior F, Kempel A, Von Heymann C. Increased chest tube drainage is independently associated with adverse outcome after cardiac surgery. J Cardiothorac Vasc Anesth. 2012;26:46-51.
- Piekarski F, Wunderer F, Raimann FJ, Neef V, Peuckert M, Brenner T, et al. Erfassung von intra-operativen Blutverlusten Ergebnisseeiner multizentrischen Erhebung und- Überblickaktueller Methodenzur Quantifizierung von Blutverlusten. Anä sthIntensivmed. 2020;61:110-6.
- Müller MM, Meybohm P, Geisen C, Schmitz-Rixen T, Serve H, Seifried E et al. Patient blood management-Wie geht das praktisch? Anästhesiol Intensivmed Notfallmed Schmerzther. 2014;49:266-272.
- Song K, Pan P, Yao Y, Jiang T, Jiang Q. The incidence and risk factors for allogenic blood transfusion in total knee and hip arthroplasty. J Orthop Surg Res. 2019;14:273.
- Carling MS, Jeppsson A, Eriksson BI, Brisby H. Transfusions and blood-loss in total hip and knee arthroplasty: A prospective observational research. J Orthop Surg Res. 2015;10:48.
- Sehat KR, Evans RL, Newman JH. Hidden blood-loss following hip and knee arthroplasty. Correctmanagement of blood-loss should take hidden loss into account. J Bone Joint Surg Br. 2004;86:561-565.
- Bradley KE, Ryan SP, Penrose CT, Grant SA, Wellman SS, Attarian DE, et al. Tranexamic acid or epsilon-aminocaproic acid in total joint arthroplasty? A randomized controlled trial. Bone Joint J. 2019;101:1093-1099.
- Fowler AJ. Meta-analysis of the association between pre- operative anaemia and mortality after surgery. Br J Surg. 2015;102:1314-1324.
- Muñoz, M. Pre-operativehaemoglobin levels and iron status in a large multicentre cohort of patients undergoing major elective surgery. Anaesthesia. 2017;72:826-834.
- Mathew KK. Is iron deficiency anemia a risk factor for poorer outcomes in primary total knee arthroplasty?. J Arthropl. 2020;35:1252-1256.
- Jørgensen CC, Kehlet H. Lundbeck Foundation Centre for Fast- track Hip and Knee replacement collaborative group. Early thromboembolic events £1week after fast-track total hip and knee arthroplasty. Thromb Res. 2016;138:37-42.
- Everhart JS, Sojka JH, Mayerson JL, Glassman AH, Scharschmidt TJ. Perioperative allogeneic red blood-cell transfusion associated with surgical site infection after total hip and knee arthroplasty. J Bone Joint Surg Am. 2018;100:288-294.
- Rasouli MR, Maltenfort MG, Erkocak OF, Austin MS, Waters JH, Parvizi J. Blood management after total joint arthroplasty in the United States: 19-year trend analysis. Transfusion. 2016;56:1112-1120.
- Pujol NA, Morrison R, Casson C, Khan S, Marriott A, Tiplady C, et al. Pre-operative screening and intervention for mild anemia with low iron stores in elective hip and knee arthroplasty. Transfusion. 2017;56:3049-3057.
- Reshan RG. Preloading vs Coloading of Crystalloid Fluid To Control Hypotension Due To Spinal Anesthesia. Int J Curr Adv Res. 2018;6:585-588.
- Chen JY, Lo NN, Tay DK, Chin PL, Chia SL, Yeo SJ. Intra- articular administration of tranexamic acid in total hip arthroplasty. J Orthop Surg Res. 2015;23:213-217.
- Mehr Aein MS. Does a single bolus dose of tranexamic acid reduce blood-loss and transfusion requirements during hip fracture surgery? A prospective randomezed double blind research in 67 patients. Acta Medica Iranica. 2007;45:437-442.
- Vijay BS, Bedi V, Mitra S, Das B. Role of tranexamic acid in reducing post-operative blood-loss and transfusion requirement in patients undergoing hip and femoral surgeries. Saudi J Anaesth. 2013;7:29-32.
- Jejani A, Chaudhari A, Singam A, et al. Evaluation of role of tranexamic acid in reducing blood-loss and transfusion rate in patients undergoing lower limb orthopaedic surgeries. J Evolution Med Dent Sci. 2020;9:142-147.
- Magill P, Cunningham EL, Hill JC, Beverland DE. Identifying the period of greatest blood-loss after lower limb arthroplasty. Arthroplast Today. 2018;4:499-504.
- Thipparampall AK, Gurajala I, Gopinath R. The effect of different dose regimens of tranexamic acid in reducing blood- loss during hip surgery. Indian J Anaesth. 2017;61:235-239.
- Miller RD. Patient blood management: Transfusion therapy In: Miller’s Anesthesia. 8th Edition. Philadelphia. Churchill Livingstone Elsevier. 2015;61:1830-1867.
- Jejani, Ayushma, Ashok C, Amol S, Pratibha N, Basant L, et al. Evaluation of Role of Tranexamic Acid in Reducing Blood Loss and Transfusion Rate in Patients Undergoing Lower Limb Orthopaedic Surgeries. J Evol Med Dent Sci. 2020;9:142-147.
- Das, Moumita, Tushar S, Sourya A, Samarth S. Pattern of Change in Blood Glucose Level in Hospitalized Patient Treated with Inhaled Corticosteroid. Medical Science. 2020;24:1122– 1127.
- Deo, Nikhil, Gajanan P, Suvarn G, Kiran S. Evaluation of Risk Factors Influencing Instability after Total Hip Replacement. J Clin Diagnostic Res. 2020;14:137-144.
- Pisulkar, Gajanan, Kiran S, Dhruva U, Angachekar, Mohit D, et al. Intraoperative Periprosthetic Fracture of Femur in a Case of Revision Total Hip Replacement: A Case Report. Medical Science. 2020;24:2691–2699.
- Vaidya, Laukik, Kiran K, Waqar N, Simran N, Gajanan P, et al. Revision of Total Hip Replacement Surgery in Elderly Patient and Its Recovery Based on Periprosthetic Fracture Rehabilitation. Medical Science 2020;24:2628-2638.
- Abbafati, Cristiana, Kaja M, Abbas, Mohammad A, Mitra A, et al. Five Insights from the Global Burden of Disease Study 2019. Lancet. 2020;396:1135-59.
- Lozano, Rafael, Nancy F, John EM, Megan K, Celine M, et al. Measuring Universal Health Coverage Based on an Index of Effective Coverage of Health Services in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020; 396:1250-84.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.