Medial Malleolar Fractures: An Anatomic Survey Determining the Ideal Screw Length
2 Department of Orthopaedic Surgery and Traumatology, Hospital Santa Teresa, Petrópolis, Rio de Janeiro, Brazil, Email: labronici@healthcare.com
3 Department of the Locomotive Aparatus, Federal University of Minas Gerais, Belo Horizonte, MG, Brazil, Email: robinsonestevespires@gmail.com
4 Department of Orthopedic Surgery, Greenville Health System University Medical Center, Greenville, South Carolina, USA, Email: jeray_k@gmail.com
Citation: Labronici PJ, Pires RE, Franco MV, Freitas R, Araújo GC, Pires e Albuquerque RS, et al. Medial malleolar fractures: An anatomic survey determining the ideal screw length. Ann Med Health Sci Res 2016;6:308-10.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Medial malleolar fractures are frequent, and their treatment is familiar to the orthopedic surgeon. Lag screw fixation using partially threaded screws remains the standard treatment method for medial malleolar fractures. However, the literature lacks a defined method for selecting lag screw length, relying more so on the empiric choice of the surgeon. Aim: The aim of this study is to help define the ideal lag screw length for medial melleolar fracture fixation. Materials and Methods: One hundred and sixteen anatomic specimens were included in the study. A transverse cut was performed in the distal third of the tibia, roughly 1 and a half times the distal tibial plafond width from the ankle joint. A coronal cut was then performed using the center of the medial malleolus. Three observers measured the distance between the medial malleolus tip and beginning of the medullary canal in all anatomic specimens. Differences in measurements were statistically compared, level of (P ≤ 0.05). Interclass correlation coefficient (ICC) significance level was set at P < 0.05. Results: Measurement average was 55 mm between the medial malleolus tip and the medullary canal, with a standard deviation of 10 mm. High concordance (ICC: 0.819) was achieved among all pairs of observers (P < 0.01). The systematic difference among measurements was absent, and random distribution around general measurements was observed. Conclusion: The authors recommend a screw length of no more than 45 mm to optimize the location of the screw threads in the best cancellous bone in an effort to obtain the most compression.
Keywords
Ankle, ankle fractures, medial malleolus
Introduction
Ankle fractures are one of the most common injuries treated by the orthopedic surgeon.[1]
Although nondisplaced medial malleolar fractures are suitable for conservative treatment, in the vast majority of cases the fractures are displaced and require surgical treatment. Several treatment options are available for medial malleolar fracture fixation, including lag screws, tension band, small precontoured plates, and K-wires. However, partially threaded screws remain the most common method for fracture fixation.[2-5]
However, the literature lacks a defined method for selecting lag screw length, relying more so on the empiric choice of the surgeon.
The present study aims to determine the ideal screw length for medial malleolar fractures based on an anatomic study of the distal tibia metaphyseal bone.
Materials and Methods
Settings and design
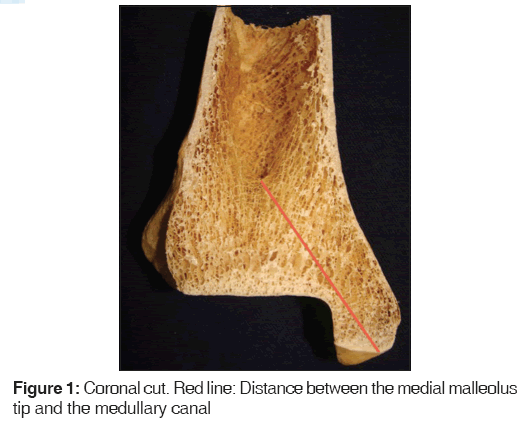
One hundred and sixteen skeletally mature anatomic specimens of the Latin American population were used in the study. Determining the age and gender was impossible due to only the limbs were available for measurements. A transverse cut was performed in the distal third of the tibia, roughly one and a half times the distal tibial plafond width from the ankle joint. Another coronal cut was then performed using the center of the medial malleolus. Using a caliper, three observers measured the shortest distance between the medial malleolus tip and the medullary canal in all anatomic specimens. Two measurements of the same location were performed by each observer to improve measurement accuracy [Figure 1].
Statistical analysis
According to Bland-Altman recommendation of 100 as an adequate sample size for a study of agreement among measurements (95% confidence interval [CI]), 116 anatomic specimens were obtained to ensure that this study was well powered (95% CI).[6]
The interclass correlation coefficient (ICC) was applied according to Landis and Koch to assess interobserver reproducibility. [7] Bland-Altman plots were used to analyze measurement dispersion by each observer and verify if bias or another systematic discrepancy existed among these measurements. The statistical analysis was performed using the IBM SPSS Statistical for Windows Software (Version 20.0, Armonk, New York, IBM Corp), and significance level was 5% (P ≤ 0.05).
Ethical approval was granted by the Local Ethics Committee.
Results
The measurements are described in their central dispersion tendency in Table 1. The narrow CIs and variations suggest high measurement precision [Table 1].
| Observer | Mean (mm) | SD | CI 95% | Median | Q1 | Q3 | Minimun (mm) | Maximum (mm) | CV |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 52.9 | 12.3 | 50.6-55.1 | 51 | 45 | 60 | 25 | 100 | 23.3 |
| 2 | 56.8 | 9.8 | 55.0-58.6 | 57 | 50 | 63 | 33 | 97 | 17.3 |
| 3 | 55.9 | 9.1 | 54.3-57.6 | 55 | 50 | 61 | 38 | 88 | 16.2 |
SD: Standard deviation, CI: Confidence interval, Q: Quartile, CV: Coefficient of variation
Table 1: Observers measurements
Observer 1 presented the highest agreement level (ICC = 0.979), almost perfect. His precision was followed by observers 2 (ICC = 0.962) and 3 (ICC = 0.936), expressing high measurement reproducibility (P < 0.01).
Table 2 provides information about means and agreement limits according to Bland-Altman [Table 2].
| Observer | ICC | SD | CI 95% | P |
|---|---|---|---|---|
| 1×2 | 0.762 | 1.23 | 0.969-0.985 | <0.0001 |
| 1×3 | 0.792 | 0.98 | 0.946-0.974 | <0.0001 |
| 2×3 | 0.927 | 0.91 | 0.674-0.829 | <0.0001 |
ICC: Interclass coefficient of correlation, SD: Standard deviation, CI: Confidence interval
Table 2: Interobserver reproducibility
Agreement limits for observers 1 and 2 were narrow (maximum 1 mm), showing high reproducibility. Observer 3 presented slightly wider limits, reaching 1.3 mm. The absence of systematic differences between repeated measurements from the same observer was found.
This study showed an average distance of 55 mm between the medial malleolus tip and the start of the medullary canal in 116 skeletally mature anatomic specimens, with a 10 mm standard deviation (SD).
Discussion
Displaced medial malleolar fractures usually require surgical treatment, and partially threaded screws are the most commonly employed surgical option for fracture fixation.[8-13] However, the literature lacks criteria for the adequate choice of lag screw length.
Excessively long partially threaded screws can bypass the good cancellous bone in the metaphyseal area and lead to inefficient compression due to poor screw thread purchase inside the medullary canal. An excessively short screw can endanger fracture compression due to screw threads not completely bypassing the fracture site. The present study showed an average distance of 55 mm (SD: 10 mm) between the medial malleolus tip and the start of the medullary canal in 116 Latin American cadavers, with a 10 mm SD. Therefore, when using a typical partially threaded screw (roughly 16 mm of thread length), one can conclude that the ideal screw length is roughly 45 mm for placement of the screw threads in the optimal cancellous bone to generate effective fracture site compression.
Parker et al.,[3] in a biomechanical study of human cadavers, compared the compression at the fracture site treated with either 30 or 45 mm long partially threaded screws or 45 mm fully threaded screws. The authors hypothesized that the partially threaded screws provide inadequate compression as a result of bypassing the physeal scar, and proposed that better purchase may be achieved with fully threaded screws or shorter partially threaded screws. The median compression at the fracture site achieved with 45 mm fully threaded screws and 30 mm partially threaded screws were significantly higher than that achieved with 45 mm partially threaded screws. Therefore, the authors recommend the use of 45 mm fully threaded or 30 mm partially threaded screws when fixing fractures of the medial malleolus. This information strongly confirms the relevance of the present study. The current literature lacks consensus concerning the precise screw length to provide adequate fracture compression in medial malleolar fractures. Our study demonstrated that screws longer that 55 mm (SD: 10 mm) will probably bypass the metaphyseal area, thereby leading to poor fracture compression.
Weaknesses of the present study include the lack of specimen gender, age, and most importantly bone quality. Although this information could potentially change the measurements (for example with severe osteopenia the canal may be wider and the distance from the tip of the medial mallelous shorter), the authors believe the sample size helps minimize this weakness.
Conclusion
The authors recommend a screw length of no more than 45 mm to optimize the location of the screw threads in the best cancellous bone in an effort to obtain the most compression. The authors believe stable and effective fracture fixation is achieved when using the appropriate screw length, thereby improving clinical outcomes.
Compliance with Ethical Standards
Authors declare that they have no conflict of interest related to the present study.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
This study was performed in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Financial support and sponsorship
Nil.
Conflict of Interest
There are no conflicts of interest.
REFERENCES
- Reinherz RP, Granoff SR, Henning KE, Ross BS. Characteristics and operative management of supination external rotation ankle fractures. J Foot Surg 1991;30:356-63.
- Pagliaro AJ, Michelson JD, Mizel MS. Results of operative fixation of unstable ankle fractures in geriatric patients. Foot Ankle Int 2001;22:399-402.
- Parker L, Garlick N, McCarthy I, Grechenig S, Grechenig W, Smitham P. Screw fixation of medial malleolar fractures: A cadaveric biomechanical study challenging the current AO philosophy. Bone Joint J 2013;95-B: 1662-6.
- Hahn DM, Colton CL. Malleoli. In: Ruedi TP, Buckley RE, Moran CG, editors. AO Principles of Fracture Management. 2nd ed., Vol. 2. Davos, Switzerland: AO Publishing; 2007. p. 888.
- Hak DJ, Lee MA. Ankle fractures: Open reduction internal fixation. In: Wiss DA, editor. Master Techniques in Orthopaedic Surgery: Fractures. Master Techniques in Orthopaedic Surgery. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2006. p. 556-7.
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307-10.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74.
- Ricci WM, Tornetta P, Borrelli J Jr. Lag screw fixation of medial malleolar fractures: A biomechanical, radiographic, and clinical comparison of unicortical partially threaded lag screws and bicortical fully threaded lag screws. J Orthop Trauma 2012;26:602-6.
- Perren SM. Force measurements in screw fixation. J Biomech 1976;9:669-75.
- Messmer P, Perren SM, Suhm N. Screws. In: Ruedi TP, Buckley RE, Moran CG, editors. AO Principles of Fracture Management. 2nd ed., Vol. 1. Davos, Switzerland: AO Publishing; 2007. p. 216.
- Pires R, Pereira A, Abreu-E-Silva G, Labronici P, Figueiredo L, Godoy-Santos A, et al. Ottawa ankle rules and subjective surgeon perception to evaluate radiograph necessity following foot and ankle sprain. Ann Med Health Sci Res 2014;4:432-5.
- Giordano V, Gomes AF, Amaral NP, Albuquerque RP, Pires RE. Preventing surgical complications: A survey on surgeons’ perception of intra-articular malleolar screw misplacement in a cadaveric study. Patient Saf Surg 2011;5:24.
- Barnes H, Cannada LK, Watson JT. A clinical evaluation of alternative fixation techniques for medial malleolus fractures. Injury 2014;45:1365-7.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.