Minimally Invasive Plating Osteosynthesis with Nonlocked Small Fragment Implants for Extra-articular Fractures of the Distal Tibia
2 Núcleo Especializado de Ortopedia e Traumatologia, Clínica São Vicente, Rio de Janeiro, Brazil
3 Departamento de Radiologia, Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brazil
Citation: Vincenzo Giordano. Minimally Invasive Plating Osteosynthesis with Non-locked Small Fragment Implants for Extra-articular Fractures of the Distal Tibia. Ann Med Health Sci Res. 2017; 7: 289-294
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: In most diaphyseal and metaphyseal fractures of the distal tibia, treatment with open reduction and absolute stability with a plate is gradually changing to a concept of functional alignment and elastic fixation, a concept based on indirect reduction and percutaneous plating osteosynthesis, known as the MIPO (minimally invasive plating osteosynthesis) technique. In this technique, the bone is accessed through soft-tissue windows away from the fracture, thus avoiding direct exposure of the fracture site. Aim: The aim of this study is to evaluate a case series of distal diaphyseal and metaphyseal extra-articular tibia fractures treated according to the MIPO technique using small fragment non-locked implants. Materials and methods: This retrospective study reviewed of all cases of distal diaphyseal and metaphyseal extra-articular tibia fractures treated at our institution with the MIPO technique using conventional small fragment implants between January 2008 and January 2012. Patient demographics, operative reports, and clinical notes were reviewed, and time to radiographic union was assessed. Clinical outcomes were retrieved from patients at their follow-up visits, using the criteria by Olerud and Molander. Outcome parameters were compared between the 2 groups, distal diaphyseal and distal metaphyseal tibia fractures. Results: Thirty-eight patients with distal diaphyseal and metaphyseal extra-articular tibia fractures treated with MIPO technique using small fragment non-locked implants were identified. The mean time for radiographic union was 14 weeks (range: 12–17 weeks). There was no statistically significant difference between both groups regarding time for union. Of the 38 patients, 20 had a score superior to 91 (excellent) and 18 had between 61 and 90 (good). None of the patients had bad or poor results according to the criteria of Olerud and Molander (less than 60). The main complaints were sporadic or permanent perimalleolar edema, inability to run or jump, and slight reduction in work capacity or daily activities. We found no implant loosening, early loss of reduction, intraoperative malreduction, delayed union or nonunion, refractures, soft tissue irritation, or infection. Implant removal was not necessary in any cases. Conclusion: The use of non-locked small fragment implants is simple, affordable, and reliable method in clinical practice, and presents a good alternative for treating distal tibia fractures, with low rates of technical problems and complications, and satisfactory outcomes.
Keywords
Treatment distal tibia fracture; Plate osteosynthesis; MIPO distal tibia
Introduction
Biological fixation has drastically modified orthopedic trauma surgery [1]. The understanding that minor surgical trauma with less secondary vascular damage and preservation of the periosteum around the fracture zone maintains local healing properties has been essential in the evolution. For most diaphyseal and metaphyseal fractures, the paradigm of open direct reduction with absolute stability has gradually changed to a concept of functional alignment with relative stability based on indirect reduction and percutaneous plating osteosynthesis, known as the MIPO (minimally invasive plating osteosynthesis) technique. Among other advantages, this evolution has led to a reduction in the incidence of complications, especially with regard to soft tissues.
Many studies have pointed out the benefits of the minimally invasive technique for the distal third of the leg, an area in which the soft tissue envelope and vascular supply are critical [2-4]. Borrelli et al. demonstrated better preservation of extraosseous vascularization in the distal third of the tibia in human specimens using MIPO, in comparison with the traditional technique [5]. These authors also recommended the use of less bulky implants for operative stabilization of distal tibia fractures [5]. Despite this recommendation, the choice between locking and non-locking plates is still a matter of debate. Recently in a systematic review comparing the outcomes of locked (n=17) and non-locked (n=11) plates in treating distal tibia fractures, Khalsa et al. showed that locked plating reduces the odds of reoperation and malalignment [6]. However, this study had at least two significant limitations: the use of large fragment nonlocked implants (9 of 11 studies) and the use of periarticular, pre-contoured non-locked plates (2 of 11 studies).
We hypothesized that non-locking, small fragment plates could adequately stabilize diaphyseal and metaphyseal extra-articular fractures of the distal tibia, avoiding soft tissue complications such as subcutaneous prominence and skin irritation. In our institution, for the last seven years the senior author of this study has been treating these fractures with the MIPO technique, using non-locking, long (14 holes or more) small fragment plates (3.5 mm reconstruction plate or 3.5 mm dynamic compression (DC) plate), with satisfactory results. In the current study, we present the surgical technique and retrospectively evaluate a case series of diaphyseal and metaphyseal extra-articular distal tibia fractures treated using the MIPO technique and non-locking small fragment plates.
Materials and Methods
Subjects
Following approval from the Hospital Municipal Miguel Couto Institutional Review Board, we analyzed the charts for all skeletally mature patients admitted to our institution for diaphyseal or metaphyseal extra-articular fractures of the distal tibia during a 5-year period (between January 2010 and January 2015) according to the inclusion criteria. Inclusion criteria were: (1) at least 2 years of follow-up data and (2) management using the MIPO technique, using non-locking small fragment reconstruction or DC plates. A total of 104 patients with extra-articular fractures of the distal tibia were admitted to our institution during this period. Forty-three fractures were diaphyseal and 61 metaphyseal. Patients treated with open reduction and absolute stability, intramedullary nailing, MIPO technique with large fragment or precontoured plates, or who had a fracture line extending distally to the tibiotalar joint or proximally to the mid-diaphysis were not included in the study.
Thirty-eight patients were treated with MIPO technique using non-locked small fragment implants. Twenty-six (68.4%) patients were men and 12 (31.6%) were women, with a mean age of 36.6 years (range: 29.2–43.9 years). The right side was affected in 24 (63.2%) patients and the left side in 14 (36.8%). Thirteen (34.2%) fractures occurred in the distal diaphysis and 25 (65.8%) in the distal metaphysis of the bone. According to the AO classification, two (5.3%) fractures were the 42-A1.3 type, six (15.8%) 42-A2.3, two (5.3%) 42-A3.3, three (7.9%) 42-B1.3, 22 (57.8%) 43-A1 and three (7.9%) 43-A2.
Thirty-six (94.7%) patients had an isolated fracture of the distal tibia and two (5.3%) were polytraumatized. All patients sustained closed distal tibia fractures. The most common mechanism of injury was motorcycle accident in 21 (55.3%) patients. The demographic data are shown in Table 1.
| Number | Age (years) | Sex | Diagnosis (fracture) | Side | AO Classification | Trauma mechanism |
|---|---|---|---|---|---|---|
| 1 | 37.9 | F | DD | R | 42-A2.3 | Hit by vehicle |
| 2 | 30.1 | M | DM | L | 43-A2 | MC accident |
| 3 | 41.0 | M | DM | L | 43-A1 | Fall down stairs |
| 4 | 32.8 | M | DM | R | 43-A1 | MC accident |
| 5 | 39.5 | M | DD | R | 42-A3.3 | Sports injury |
| 6 | 29.2 | F | DD | R | 42-A1.3 | Sports injury |
| 7 | 38.4 | M | DD | L | 42-A2.3 | MC accident |
| 8 | 32.1 | M | DM | R | 43-A1 | MC accident |
| 9 | 40.7 | F | DM | R | 43-A2 | Fall down stairs |
| 10 | 31.7 | M | DM | R | 43-A1 | MC accident |
| 11 | 36.3 | M | DM | R | 43-A1 | MC accident |
| 12 | 40.1 | M | DM | R | 43-A1 | MC accident |
| 13 | 33.3 | F | DM | L | 43-A1 | MV collision |
| 14 | 39.1 | M | DM | L | 43-A1 | MC accident |
| 15 | 42.8 | F | DD | R | 42-A2.3 | Fall down stairs |
| 16 | 40.9 | F | DM | R | 43-A1 | Fall to the ground |
| 17 | 35.8 | M | DD | L | 42-B1.3 | MC accident |
| 18 | 32.0 | M | DM | R | 43-A1 | MC accident |
| 19 | 34.5 | M | DM | R | 43-A1 | MC accident |
| 20 | 30.8 | F | DM | R | 43-A1 | MC accident |
| 21 | 40.2 | M | DM | R | 43-A1 | Sports injury |
| 22 | 38.6 | M | DM | E | 43-A1 | MC accident |
| 23 | 32.6 | M | DM | R | 43-A1 | MC accident |
| 24 | 37.1 | M | DD | R | 42-A3.3 | Sports injury |
| 25 | 37.0 | M | DM | L | 43-A2 | Hit by vehicle |
| 26 | 31.9 | M | DD | R | 42-B1.3 | MV accident |
| 27 | 39.5 | F | DM | R | 43-A1 | Fall down stairs |
| 28 | 42.8 | M | DM | R | 43-A1 | Fall to the ground |
| 29 | 33.9 | M | DM | L | 43-A1 | MC accident |
| 30 | 38.7 | M | DM | L | 43-A1 | MC accident |
| 31 | 41.0 | F | DD | R | 42-A2.3 | MC accident |
| 32 | 38.2 | F | DM | R | 43-A1 | Fall to the ground |
| 33 | 37.4 | M | DD | L | 42-B1.3 | MC accident |
| 34 | 41.3 | M | DM | R | 43-A1 | Hit by vehicle |
| 35 | 35.0 | M | DM | L | 43-A1 | Sports injury |
| 36 | 40.1 | F | DD | R | 42-A1.3 | Fall to the ground |
| 37 | 33.5 | F | DM | L | 43-A1 | MC accident |
| 38 | 33.0 | M | DD | R | 42-A2.3 | MC accident |
Abbreviations: M - Male; F - Female; DD - Distal Diaphyseal; MD - Distal Metaphyseal; R - Right; L - Left; MC - Motorcycle; MV - Motor Vehicle
Table 1: Patient demographic data (n = 38).
The polytraumatized patients had their fractures acutely stabilized with external fixation upon admission. One had bilateral femur fractures, blunt abdominal trauma, and distal metaphyseal tibia fracture of the left leg (case 13). The other had proximal metaphyseal fracture of the right tibia, left acetabular fracture, chest trauma, and distal metaphyseal fracture of the left leg (case 14).
The mean period between admission and definitive surgical procedure was 8 days (range: 0–10 days). All patients except for the polytraumatized patients were immobilized using a removable splint until the surgical procedure.
Surgical technique
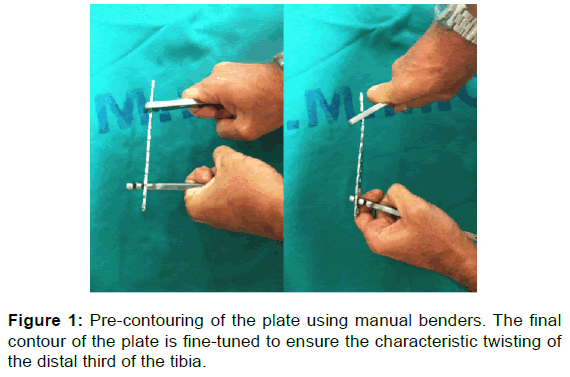
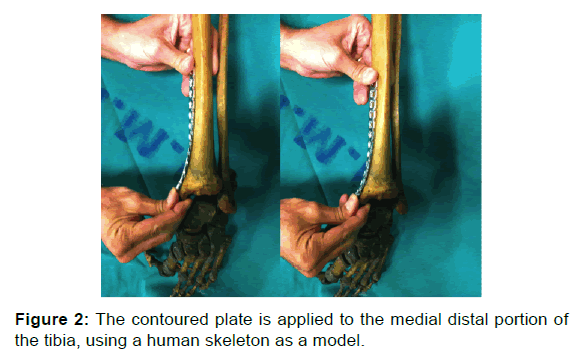
One surgeon performed the procedures on all patients. A nonlocked small fragment DC plate was used in 10 cases and a nonlocked small fragment reconstruction plate in 28 cases. Plates containing a minimum of 14 holes were precontoured into position using the distal third of the tibia of a human skeleton on the day before surgery [Figures 1 and 2].
Patients were positioned on a radiolucent operating table in supine position, without a tourniquet. Indirect reduction of the fracture was obtained under fluoroscopy and provisionally maintained with 2.5 mm K-wires. The distal approach involved a transverse medial incision of 10.0 mm immediately proximal to the medial malleolus. The plate was percutaneously inserted through the distal incision in a retrograde fashion. The proximal approach involved a longitudinal medial incision of 10.0 mm made over the tip of the plate. Two 2.5 mm K-wires were routinely placed into the most proximal and most distal holes of the plate to secure the implant to the bone. Three bicortical 3.5 mm screws were usually placed alternately in the plate proximally and distally through stab incisions. The working area of the implant was calculated based on the size of the distal fragment. The quality of reduction and the final position of plate and screws were fluoroscopically assessed. The incisions were closed in a layered fashion, with subcutaneous and skin closure. The distal fibula was not regularly fixed, although open reduction and internal fixation had been performed in the first three patients.
After surgery patients received regular pain medication. Immediate ankle mobilization was encouraged in all patients postoperatively with active flexion and extension. Patients were usually discharged from hospital on the second postoperative day. Partial weight-bearing with crutches was initiated 2 weeks after surgery and was increased gradually, based on the clinical and radiographic findings.
Follow-up and outcome evaluation
All patients were evaluated at 1, 2, 3, 6, and 12 weeks after the procedure, and 6 and 12 months after hospital discharge with clinical and radiographic examination. After the first year, patients underwent clinical and radiographic follow-up examinations every 12 months.
Clinical outcomes were assessed using the functional score of Olerud and Molander, first described for ankle fractures, but which has been used by several authors for distal fractures of the tibia [7-10]. According to these authors, the results are considered excellent when between 91 and 100, good between 61 and 90, bad between 31 and 60 and poor between 0 and 30 [7]. The score of Olerud and Molander is shown in Table 2. Fractures were defined as healed when patients were able to fully bear their weight without significant discomfort and radiographs demonstrated 3 cortices of bony bridging [11].
| Parameter | Degree | Score |
|---|---|---|
| Pain | None While walking on uneven surface While walking on even surface outdoors While walking indoors Constant and severe |
25 20 15 10 0 |
| Stiffness | None When stretching Stiffness |
10 5 0 |
| Swelling | None Only evenings Constant |
10 5 0 |
| Stair climbing | No problems Impaired Impossible |
10 5 0 |
| Sports activities | Normal Difficult Impossible |
10 5 0 |
| Supports | None Taping Stick or crutches |
10 5 0 |
| Work, activities of daily life | Unchanged Unchanged but slower Less heavy work on part-time Partially or totally impaired |
25 20 10 0 |
Table 2: Score of olerud and molander [7].
Statistical analysis
Variables were compared using the Mann-Whitney u test. Statistical significance was defined as p < 0.05. The rate of complications was compared between the 2 groups (distal diaphyseal and distal metaphyseal tibia fractures) using Fisher’s exact test.
Results
The average clinical and radiographic follow-up time was 30.8 months (range 24.0–60.0 months). No patients were lost to follow-up. The mean time for fracture union was 14 weeks (range: 12–17 weeks). Average bone healing time in patients with distal diaphyseal tibia fracture (n=13) was 15.4 weeks (range: 12.0–17.0 weeks) and for patients with distal metaphyseal fracture (n=25) was 13.7 weeks (range: 12.0–16.1 weeks). There was no statistically significant difference between the time of union in the two groups (p=0.74).
The Olerud and Molander functional scores for the 38 patients showed 20 (52.6%) excellent and 18 (47.4%) good results. None of the patients had bad or poor results. There was no difference in the functional outcome between the two groups. On physical examination, good healing of all incisions was noted. The main complaint was minor swelling of the ankle region, mostly noted in the distal metaphyseal tibia fracture patients, although without statistical significance (p=0.4). Inability to run or jump and slight reduction in work capacity or daily activities were rarely observed.
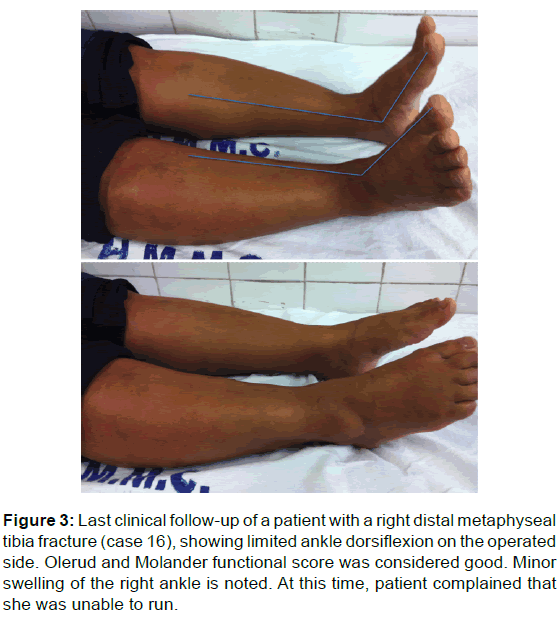
At the last clinical follow-up, all patients had restored normal range of motion of the ipsilateral knee. There was a mean loss of 5o in ankle dorsiflexion (range: 0o–10o). This loss was greater in the distal diaphyseal fracture patients, with a mean of 6o (range: 0°–10°), than in the distal diaphyseal fracture patients, who had a mean loss of 4o (range: 0°–10°), although this difference did not exhibit statistical significance (p=0.61) [Figure 3].
Figure 3: Last clinical follow-up of a patient with a right distal metaphyseal tibia fracture (case 16), showing limited ankle dorsiflexion on the operated side. Olerud and Molander functional score was considered good. Minor swelling of the right ankle is noted. At this time, patient complained that she was unable to run
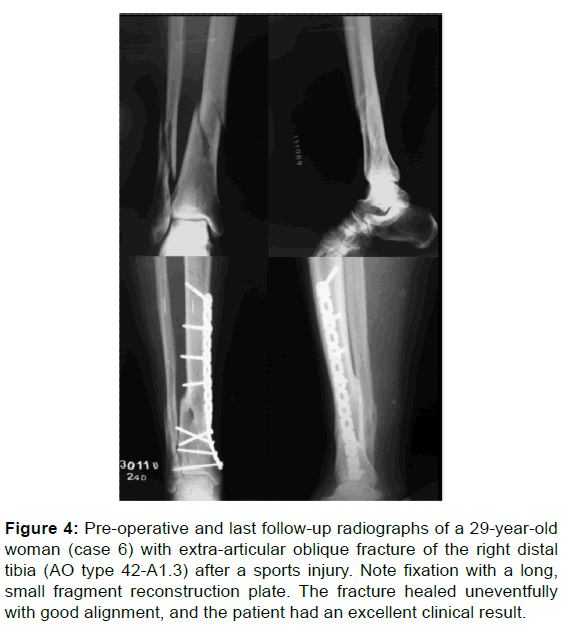
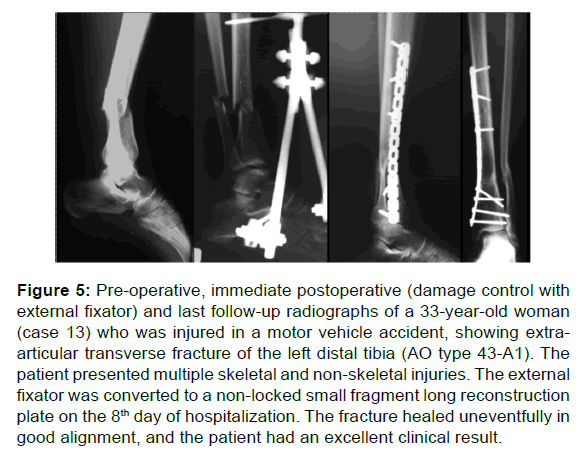
At the last radiographic follow-up, no signs of implant loosening, loss of reduction, or post-traumatic osteoarthritis were seen in any cases [Figures 4 and 5]. Malalignment of the limb with less than 10° valgus angulation occurred in one case, a patient with distal diaphyseal fracture patient (case 1) at the last follow-up. After thorough evaluation of the postoperative x-rays, we noticed that the fracture was initially reduced and fixed in valgus.
Figure 4: Pre-operative and last follow-up radiographs of a 29-year-old woman (case 6) with extra-articular oblique fracture of the right distal tibia (AO type 42-A1.3) after a sports injury. Note fixation with a long, small fragment reconstruction plate. The fracture healed uneventfully with good alignment, and the patient had an excellent clinical result.
Figure 5: Pre-operative, immediate postoperative (damage control with external fixator) and last follow-up radiographs of a 33-year-old woman (case 13) who was injured in a motor vehicle accident, showing extraarticular transverse fracture of the left distal tibia (AO type 43-A1). The patient presented multiple skeletal and non-skeletal injuries. The external fixator was converted to a non-locked small fragment long reconstruction plate on the 8th day of hospitalization. The fracture healed uneventfully in good alignment, and the patient had an excellent clinical result.
There was no case of implant loosening, early loss of reduction, delayed union or nonunion, wound breakdown, or infection. No hardware was removed.
Discussion
The results of the current study indicate that non-locking, small fragment plates can adequately stabilize diaphyseal and metaphyseal extra-articular fractures of the distal tibia, avoiding soft tissue complications. In treating fractures of the distal third of the tibia, preservation of soft tissue integrity is particularly critical [2-4,9]. In this area, the anteromedial cortex of the tibia is subcutaneous and the soft tissue envelope is thin. Many authors have demonstrated that the integrity of the tissues surrounding the fracture site, including the periosteum, is necessary to provide the resources for bone regeneration [5,12,13]. Using a rabbit osteotomy model, Whiteside and Lesker showed that an increase in the amount of dissection leads to higher rates of healing complications [13]. Borrelli et al. demonstrated preservation of blood supply to the distal tibia after minimally invasive plating in comparison with open plating techniques. [5]. Furthermore, clinical data have confirmed that the rate of wound healing problems, infection, and nonunion are high in patients who receive open reduction internal fixation (ORIF) and medial plating for distal extra-articular tibia fractures, with incidences as high as 46% [14].
On the other hand, the percutaneous plating technique has been associated with undisturbed union and a low complication rate, even though non-locking plates are used [15-17]. This finding suggests the biological superiority of the MIPO technique in limiting surgical soft tissue trauma at the fracture site. [15]. Indeed, many authors have demonstrated the benefits of indirect reduction techniques and small incisions to insert hardware, minimizing the amount of dissection of the fracture fragments associated with more traditional methods of internal fixation [8-11,18-24]. When compared to intramedullary locked implants, another minimally invasive option for the management of these fractures, several authors have observed higher rates of malalignment and residual deformity from the nails [11,25]. Alignment problems with the use of intramedullary nails in distal tibia fractures have been described in 7% to 35% of cases [11,25]. Im and Tae compared the use of intra- and extramedullary implants in these fractures and observed a statistically significant mean final angulation of 2.8o in the first group versus 0.9o in the second group. [26].
In the current study, non-locked long (more than 14 holes) small fragment implants (reconstruction or DCP) used with a MIPO technique demonstrated excellent radiographic and clinical outcomes. Functionally, all patients had excellent or good scores, with no need for any secondary procedures to treat mechanical or biological failure. Critiques of the MIPO technique in this region are mainly related to its inability to achieve anatomic reduction equivalent to open fixation, as well as the presence of large implants, which may potentially increase the risk of skin damage. Muzaffar et al. found two cases of superficial infection, two cases of deep infection requiring hardware removal, three cases of palpable implant, and three cases of malunion [27]. Lau et al. reported the need to remove the plate in 52% of the patients because of internal skin overpressure, also observing that 15% developed late infection [3]. Proper study of the fracture pattern prior to surgery is recommended to choose the appropriate reduction technique and implant size, and may reduce these complications [27].
The only case in this present study that presented with residual angular deformity in the last consultation actually resulted from an intraoperative misevaluation by the authors, not a loss of reduction stemming from mechanical failure of the implant (DCP). We stopped using the DCP during the course of the study, because we encountered greater difficulties in contouring and placing this plate in the distal tibia, compared to reconstruction plates. As stated by Borg et al., correct bending of the plate is essential to fitting the curvature of the medial aspect of the tibia [28]. In addition, in our study no patients had skin problems related to the implant or required hardware removal.
Fixation of the fibula is an important if controversial question in the treatment of distal tibia fractures. Even though many authors advise fibula fixation in cases where it is deemed necessary to restore stability and normal anatomy in the ankle joint, it does not seem particularly necessary for fracture reduction and alignment when there is no articular involvement [17,22,29,30]. Fibula fixation was performed in the first three patients of our cohort, and 35 patients did not receive fibula fixation. We observed that indirect reduction maneuvers with traction, rotation, and percutaneous temporary fixation with K-wires are sufficient to obtain and maintain proper alignment during bridge plating for the treatment of extra-articular distal tibial fractures. Comparable results were found whether fibula fixation was performed or not, suggesting it is not necessary for extraarticular distal tibia fractures treated with the MIPO technique.
There are some recognized limitations in the current study. First, it is a retrospective case series with all patients primarily managed at the same institution; this makes the study potentially vulnerable to selection bias, since it may not appropriately represent the wider population. However, in this consecutive controlled case series from a single surgeon, all patients were exposed to the same interventions and postoperative protocol. One strength of this study is the fact that it is one of very few using non-locked small fragment plates for minimally invasive surgery of extra-articular distal tibia fractures. Furthermore, we can argue that there is low internal validity, since no comparison was made between locking and non-locking plates to treat of extra-articular distal tibial fractures. However, other studies reported no differences in bone healing and complications when locking and non-locking plates were used for biological fixation of extra-articular distal tibia fractures treated with the MIPO technique, although locking implants have a greater effect on stability [6,15,17]. Even though the advantages of locked plates are widely known, the advantages of non-locked implants to treat extra-articular distal tibia fractures with the MIPO technique are commonly forgotten or underrated. These advantages include the possibility of multiple screw angulations (especially in the shorter distal fragment), the option to use compression screws through the plate (if an articular fracture is present), and lower cost.
Conclusion
The findings from this current study support our hypothesis and show that non-locking, small fragment plates can adequately stabilize diaphyseal and metaphyseal extra-articular fractures of the distal tibia, with the expected satisfactory results. The use of non-locked small fragment implants is a simple, inexpensive, and reliable method in clinical practice, and presents a good alternative for treatment of distal fractures of the tibia, with low rates of technical problems and complications.
Conflict of Interest
All authors disclose that there was no conflict of interest.
Acknowledgements
This study was performed in accordance with the ethical standards of the Hospital Municipal Miguel Couto Institutional Review Board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
REFERENCES
- Nikolaou VS, Efstathopoulos N, Papakostidis C, Kanakaris NK, Kontakis G, Giannoudis PV. Minimally invasive plate osteosynthesis – An update. Curr Orthop. 2008;22:202–207.
- Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P, et al. Distal tibia fractures: Management and complications of 101 cases. Int Orthop. 2010;34:583–588.
- Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008;32:697–703.
- Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg.2006;14:406–416.
- Borrelli J Jr, Prickett W, Song E, Becker D, Ricci W. Extra-osseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma. 2002;16:691–695.
- Khalsa AS, Toossi N, Tabb LP, Amin NH, Donohue KW, Cerynik DL. Distal tibia fractures: locked or non-locked plating? A systematic review of outcomes. Acta Orthopaedica. 2014;85:299–304.
- Olerud C, Molander H (1984) A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg 103:190–194.
- Collinge C, Kuper M, Larson K, Protzman R (2007) Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma 21:355–361
- Collinge C, Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma. 2010;24:24–29.
- Li Y, Liu L, Tang X, Pei F, Wang G, Fang Y, et al. Comparison of low, multidirectional locked nailing and plating in the treatment of distal tibial metadiaphyseal fractures. Int Orthop. 2012;36:1457–1462.
- Vallier HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): Plating versus intramedullary nailing. J Orthop Trauma. 2008 22:307–311.
- Neagu TP, Ţigliş M, Cocoloş I, Jecan CR. The relationship between periosteum and fracture healing. Rom J Morphol Embryol. 2016;57:1215–1220.
- Whiteside L, Lesker PA. The effects of extraperiosteal and subperiosteal dissection. II. On fracture healing. J Bone Joint Surg Am. 1078;60:26–30.
- Sathiyakumar V, Thakore RV, Ihejirika RC, Obremskey WT, Sethi MK. Distal tibia fractures and medial plating: factors influencing re-operation. Int Orthop. 2014;38:1483–1488.
- Ozkaya U, Parmaksizoglu AS, Gul M, Sokucu S, Kabukcuoglu Y. Minimally invasive treatment of distal tibial fractures with locking and non-locking plates. Foot Ankle Int. 2009;30:1161–1167.
- Vidović D, Matejčić A, Ivica M, Jurišić D, Elabjer E, Bakota B. Minimally-invasive plate osteosynthesis in distal tibial fractures: results and complications. Injury. 2015;46 Suppl 6:S96–S9.
- Zhou K, Chen N. Locking versus non-locking neutralization plates with limited excision and internal fixation for treatment of extra-articular type a distal tibial fractures. Open Orthop J. 2017;11:57–63.
- Ahmad MA, Sivaraman A, Zia A, Rai A, Patel AD. Percutaneous locking plates for fractures of the distal tibia: our experience and a review of the literature. J Trauma Acute Care Surg. 2012;72:E81–E87.
- El-Nahal W, Khaled SA, Koptan W, Galal A. Time to union and functional outcome following minimally invasive plating of extra-articular fractures of the distal tibia. Egypt Orthop J. 2016;51:85–89.
- Francois J, Vandeputte G, Verheyden F, Nelen G. Percutaneous plate fixation of fractures of the distal tibia. Acta Orthop Belg. 2004;70: 148–154.
- Krackhardt T, Dilger J, Flesch I, Höntzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005;125:87–94.
- Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Rel Res. 2003;408:286–291.
- Pai V, Coulter G, Pai V. Minimally invasive plate fixation of the tibia. Int Orthop. 2007;31:491–496.
- Redfern DJ, Syed SU, Davies SJM. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury. 2004;35:615–620
- Nork SE, Schwartz AK, Agel J, Holt SK, Schrick JL, Winquist RA. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Joint Surg Am. 2005;87:1213–1221.
- Im GI, Tae SK. Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma. 2005;59:1219–1223.
- Muzzafar N, Bhat R, Yasin M. Complications of minimally invasive percutaneous plating for distal tibial fractures. Trauma Mon. 2016;21:e22131.
- Borg T, Larsson S, Lindsjö U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury. 2004;35:608–614.
- Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia. Results in 20 patients. Injury. 2006;37:877–887.
- Toms AD, McMurtie A, Maffulli N. Percutaneous plating of the distal tibia. J Foot Ankle Surg. 2004;43:199–203.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.