Mobile and Portable Dental Services Catering to the Basic Oral Health Needs of the Underserved Population in Developing Countries: A Proposed Model
- *Corresponding Author:
- Dr. Rahul Ganavadiya
Department of Public Health Dentistry, People’s Dental Academy, Bhanpur, Bhopal, Madhya Pradesh, India.
E-mail: rahulsguns@rediffmail.com
Citation: Ganavadiya R, Chandrashekar BR, Goel P, Hongal SG, Jain M. Mobile and portable dental services catering to the basic oral health needs of the underserved population in developing countries: A proposed model. Ann Med Health Sci Res 2014;4:293-304.
Abstract
India is the second most populous country in the world with an extensive rural population (68.8%). Children less than 18 years constitute about 40% of the population. Approximately, 23.5% of the urban population resides in urban slums. The extensive rural population, school children and the urban slum dwellers are denied of even the basic dental services though there is continuous advancement in the field of dentistry. The dentist to population ratio has dramatically improved in the last one to two decades with no significant improvement in the oral health status of the general population. The various studies have revealed an increasing trend in oral diseases in the recent times especially among this underserved population. Alternate strategies have to be thought about rather than the traditional oral health-care delivery through private dentists on fee for service basis. Mobile and portable dental services are a viable option to take the sophisticated oral health services to the doorsteps of the underserved population. The databases were searched for publications from 1900 to the present (2013) using terms such as Mobile dental services, Portable dental services and Mobile and portable dental services with key articles obtained primarily from MEDLINE. This paper reviews the published and unpublished literature from different sources on the various mobile dental service programs successfully implemented in some developed and developing countries. Though the mobile and portable systems have some practical difficulties like financial considerations, they still seem to be the only way to reach every section of the community in the absence of national oral health policy and organized school dental health programs in India. The material for the present review was obtained mainly by searching the biomedical databases for primary research material using the search engine with key words such as mobile and/or portable dental services in developed and developing countries (adding each of these terms in a sequential order). Based on the review of the programs successfully implemented in developed countries, we propose a model to cater to the basic oral health needs of an extensive underserved population in India that may be pilot tested. The increasing dental manpower can best be utilized for the promotion of oral health through mobile and portable dental services. The professional dental organizations should have a strong motive to translate this into reality.
Keywords
Dental manpower, Developing countries, Mobile and portable dental services, Oral health, School dental programs
Introduction
The world’s population has grown rapidly in recent years and India, is the world’s second most populous country after the People’s Republic of China.[1] India is a country with a wide range of variations based on ethnic groups; geographical character, culture, religion and languages.[2] The average life-expectancy is 62.5 years and the literacy rate is 74.0% as per the recent census report (2011).[3] A clear cut disparity was noted in the distribution of the population between rural and urban areas. The urban population was estimated to be 377.1 (31.2%) million and the rural population was 833.1 million (68.8%).[4] Children less than 18 years constitute about 40% of the population. Approximately, 23.5% of the urban population resides in urban slums.[5]
World Health Organization (WHO) recommends a dentist to population ratio of 1:7500 for achieving the optimal oral health. The dentist population ratio in India was 1:300,000 in 1960, which at present stands at 1:10,000. The statistics suggest a significant increase in the dental manpower since 1960. However, a glance at the distribution of dental manpower between rural and urban areas reflects a glaring contrast. About 80% of dentists work in major cities catering to the oral health needs of around 31% of urban population. In rural India, one dentist is serving over a population of 250,000.[2] The oral health-care delivery in India is predominantly by private dental practitioners residing in affluent urban localities on a private fee for service basis.[6] The oral health-care delivery in the public sector is offered only through the network of primary health centers and community health centers (CHC). Each primary health center cater to a population of around 30,000 in plains and 20,000 in hilly, tribal and backward areas and CHC to a population of 120,000.[7] There is no record of organized school dental program on a national basis in India and no attempts have been made to implement national oral health policy in the country though the national health policy was implemented in 1983 itself.[8]
The prevalence of dental caries, periodontal diseases and oral cancer among the Indian population are showing an increasing trend over the years. Prevalence studies on dental caries in India have shown results ranging from 31.5% to 89%.[9] The prevalence of dental caries for the various age groups in the National oral health survey and fluoride mapping in India (2002-2003) was reported to be 51.9% among 5-year-old children, 53.8% in 12-year-old children, 63.1% in 15-year-old adolescents, 80.2% in adults aged 35-44 years and 85.0% in elderly aged 65-74 years.[10] The prevalence of periodontal disease among 12, 15, 35-44 and 65-74 year old population was found to be 57%, 67.7%, 89.6% and 79.9% respectively.[11] The lower prevalence in the elderly population was due to loss of teeth in this group. A multi-centric study carried out by Ministry of Health and Family Welfare, Government of India and WHO collaborative program (2007) found the prevalence of periodontal disease among 35-44 years and 65-74 year old population in some states (Rajasthan, Orissa) to be 100%.[12] Oral and pharyngeal cancers, though are preventable, still remain a major challenge to oral health programs today. Oral cancer ranks amongst the three most common types of cancer in South Central Asia. The age standardized incidence rate per 100,000 populations is 12.6 in India. National Commission on Macroeconomics and Health (2005) has projected prevalence of various oral diseases for 2015. These projections reflect an upward trend for the most oral diseases. These data clearly reflect that the prevalence of various oral diseases have increased over a period of time despite the rising dental manpower in the country. This increase in the prevalence of oral diseases in the country is mainly due to the rising prevalence among the population in rural areas, urban slums as well as school children who represent the major bulk of the underserved population.[6,9,13,14] This is attributed to lack of awareness on etiological factors for oral diseases and methods for preventing and controlling them,[15] poor oral hygiene practices,[16] lack of access to even the basic dental services, high levels of deleterious habits like smoking and use of smokeless tobacco, which are proven risk factors for periodontal diseases and oral cancer,[17] lack of affordability to seek sophisticated dental services through private dental practitioners and lack of perception of the fact that the teeth are worth saving.[15]
This highlights the fact that the existing oral health care delivery in India that is predominantly by private dentists in affluent urban localities on a fee for service basis has not significantly contributed in the promotion of oral health in the general population, especially the extensive rural population, school children and urban slum dwellers. Alternate modes of providing dental services other than traditional dental clinics and private hospitals should be implemented to overcome these discrepancies in the oral health-care delivery between rural and urban population with special emphasis on covering the underserved population. Mobile and portable dental services may offer a viable option to address the issues of oral health-care delivery for an extensive underserved population in a developing country like India with scarce resources. Although, mobile and portable dental services have been successfully implemented in some developed and developing countries to cater to the oral health needs of underserved population,[18,19] the program is not effectively implemented in the country.
The mobile and portable dental services may solve the disparity in the dentist population ratio between urban and rural areas, lack of access for even the basic dental services in rural areas, the lack of organized dental care for underprivileged in urban slums as well as home/hospital bound patients. In the background stated above, this paper reviews mobile and portable dental services implemented in some developed and developing countries, their utility, applicability and feasibility in the oral health-care delivery for developing country like India having a vast underserved population. This paper proposes a model for oral health-care delivery that may be implemented at district level in India using private and public partnership. This proposed model may be pilot tested in some districts in India and then, on a national basis, if found successful, to cater to the oral health needs of extensive underserved population in India.
Materials and Methods
The literature for the present review was obtained from the following sources:
• Published articles
• Unpublished literature
• Internet news clippings
• Online manuals and books
• Thesis and
• Government projects.
Use of search engine to retrieve the concerned literature
The search for the literature concerning mobile and portable dental services was identified by searching the biomedical databases for primary research material. The databases were searched for publications from 1900 to the present (2013), with key articles obtained primarily from MEDLINE.
Search terms employed to retrieve the relevant literature
In order to ensure that relevant studies were not missed, the search terms remained broad. The following search terms were employed to retrieve the literature using the search engine:
• Mobile dental services
• Portable dental services
• Mobile and portable dental services
• Mobile and/or portable dental services in India
• Mobile and portable dental services in developing countries
• Mobile and portable dental services in developed countries.
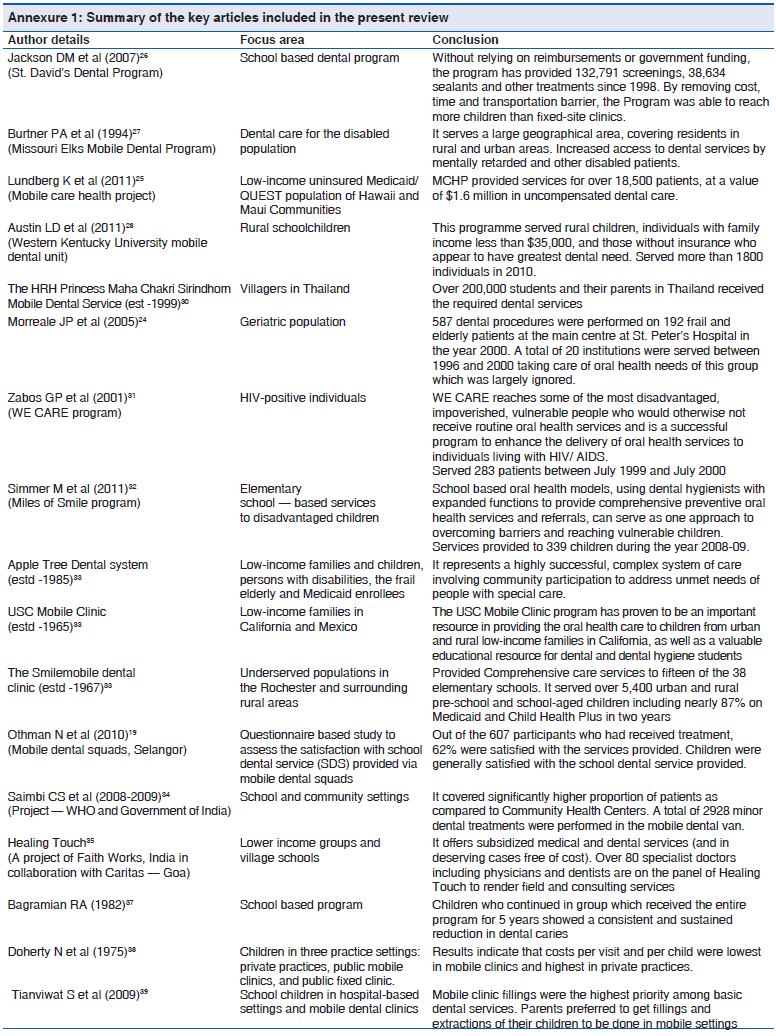
The literature with these search terms anywhere in the title or abstract was considered. No language restrictions were employed. Studies were eligible for consideration in this review if: (a) focus of the study was mobile dental services, portable dental services or combination of these and (b) there was at least one parenting variable discussed. The methodology employed in this review is denoted diagrammatically in Figure 1.
Segregation of the literature
The literature retrieved was then organized as per the following specifications:
• Primary and secondary sources
• Literature from India, from other developing countries and literature from developed countries
• Literature focusing on mobile dental services, portable dental services, mobile and portable dental services
• Literature focusing on cost effectiveness of mobile and portable dental services.
The literature on the mobile and portable dental services from India and other developing countries was scanty. This necessitated the inclusion of mobile and portable dental services in developed countries in our review. The programs successfully implemented in developed countries are reviewed in the present manuscript to demonstrate the utility of mobile dental services that may be implemented in a developing country like India. Though no language barriers were employed, the entire literature reviewed in the present manuscript was in English and the authors did not come across any published literature in a language other than English. The literature from these sources was thoroughly scrutinized by the authors and relevant information from these sources was considered for discussion under different sections of this paper.
The Results of the Search are Summarized in Table 1
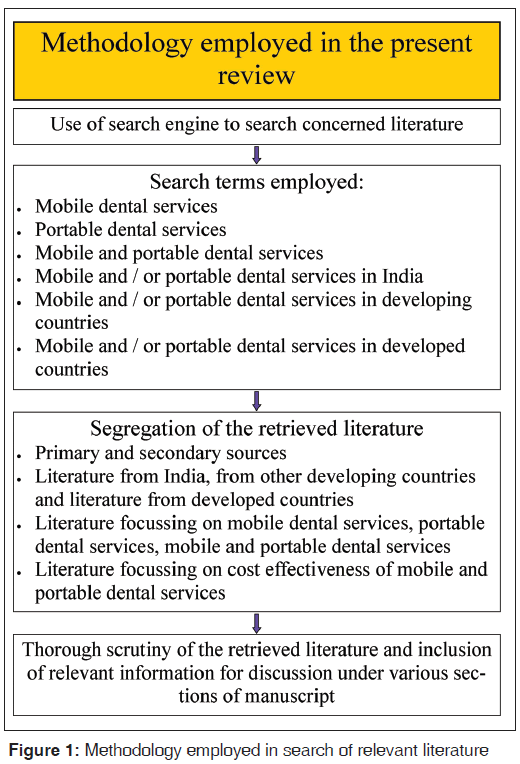
The total literature retrieved and /or collected, the segregation of literature into various specifications and the number of articles considered for discussion in the present review is summarized in Table 1. The results of the key literature considered for discussion in the present review are summarized in Annexure 1.
| Total material retrieved and / or collected | 49 |
| Primary sources | 32 |
| Secondary sources | 17 |
| Mobile dental services | 27 |
| Portable dental services | 12 |
| Mobile and portable dental services | 5 |
| Cost effectiveness of mobile and or portable dental | 4 |
| services | |
| Mobile and or portable dental services in developing | 4 |
| and developed countries | |
| Mobile dental services in India | 4 |
Table 1: Summary of the search results
Annexure 1: Summary of the key articles included in the present review
Definition
According to IAC (Indiana Administrative Code)[20] 4-2-2, Section 2 “Mobile dental facility” is defined as “any selfcontained facility in which dentistry will be practiced, which may be moved, towed or transported from one location to another.” Portable dental equipment on the other hand is defined as any non-facility in which dental equipment, utilized in the practice of dentistry, is transported to and utilized on a temporary basis at an out-of-office location, including, but not limited to:
a. Other dentists’ offices;
b. Patients’ homes;
c. Schools;
d. Nursing homes; or
e. Other institutions.[20]
Brief history
In 1917, the Cleveland Chapter of the Preparedness League of American Dentists presented a “dental ambulance” to the army in the name of Red Cross. Four dentists and one or two assistants operated the ambulance.[21] The earliest records suggesting the utilization of “Mobile Dental Van” other than military setting are credited to Dr. Talley Ballou, dental director of the Bureau of Mouth Hygiene, Virginia.[22]
Portable dentistry began during the World War II. The dental officer of each tactical unit was supplied one large shoulder pouch and his assistant carried two smaller pouches, containing instruments for emergency use in combat when M. D. Chest No. 60 was not available. The pouches included items required for the relief of pain, simple extractions, emergency treatment of maxillofacial injuries and temporary fillings.[21]
Application of mobile and portable dental services
Dental Public Health deals with community as a whole. Mobile and portable dentistry is a potential method to deliver oral health-care in the public sector. Practical application of mobile, portable or hybrid systems may be performed in multiple situations, such as:
• Educating school children regarding oral health.[23]
• Screening of the population for various oral diseases.[23]
• School and community dental health program like sealant application program.[23]
• Providing both preventive and curative services in homebound settings.[24]
• Dental services to people who are homeless, temporarily displaced or migrants.[25]
• Supplementing the medical services in case of any emergency relief situation or vaccination program.
Though mobile and portable dental services provide an innovative solution in bringing dental care to underprivileged areas, they seek the cooperation of professional organizations and other NGO’s in establishing a public-private partnership for their application on a large scale. The successful implementation and execution of oral health-care delivery using the mobile and portable dental services rely largely on collaborative efforts of the following:
• Professional dental associations
• Non-government organizations (NGOs)
• Government sector and
• Local civil society.
One of the successful examples of merging private sector with public health dentistry is the St. David’s Dental Program, a school based dental program for children. This program does not rely on reimbursements or government funding and aims to provide free dental services to low-income children in schools. It is a collaboration of community partners in Central Texas. In the year 2000, the collaboration acquired its first van — “Theo Tooth Mobile”. The Program added its second van (Theo II), associated clinical staff (dentist and dental assistant) and increased the number of children served by 26% in 2011. The program offered 132,791 oral screenings and 38,634 sealants and other treatments since 1998.[26] This program highlights the optimum utilization of dental auxiliaries and benefits to the lower income children in schools in spite of lack of funding from the government sector.
Missouri Elks Mobile Dental Program was established in the early 1970s. The program operates three mobile dental units and serves the disabled population in all areas of Missouri. Referrals are received from Regional Centers for the Developmentally Disabled, the Missouri Crippled Children’s Service and local agencies. The major advantage of this type of program is that it serves a large geographical area, thereby increasing access to residents in rural and urban areas.[27] The Mobile Care Health Project has been a safety net provider of dental services since 1997 for the low-income uninsured Medicaid/QUEST population on the island of Hawaii and on the island of Maui from 2000 to 2003. They elaborated their services to children, the physically disabled, the mentally ill, the impoverished elderly, the recent immigrant, the working poor, the homeless and the unemployed covering almost 18,500 patients.[25] These programs specifically focused on carrying sophisticated dental services to the doorsteps of the underprivileged and disabled population in underserved areas. Such programs will benefit the underserved as well as special groups, such as population in old age homes, institutions for physically and mentally disabled children, home and hospital bound patients who have difficulty in gaining access to the fixed dental clinics irrespective of their ability to pay.
The US Department of Health and Human Services identified 4230 Dental Health Professional Shortage areas with 49 million people living in them. To fill this lacuna, mobile dental health units like the Western Kentucky University (WKU) mobile dental unit was implemented. It took the help of student dental hygienists and primarily focused on placement of sealants to second and seventh grade rural school children. More than 1800 individuals were served on WKU’s mobile dental health unit in 2010.[28] This program stressed on how best the auxiliary dental manpower in the form students from dental training schools can be utilized to promote the oral health-care of the underserved population. The utilization of dental schools trainees who work under the supervision of qualified dentists will serve the dual purpose of serving the underserved and adequate training of dental school trainees to work in a social set up. The biggest advantage of Mobile Dental Clinics is that they can treat patients who have no/limited access to traditional fixed dental clinics/hospitals. They are also the best option for providing oral health education and creating awareness among rural and isolated communities. The disadvantages of mobile dental units are the high operating and maintenance cost, the difficulty in transporting the unit to isolated areas like high altitudes, dense forests etc., which are poorly connected by roads.
Portable dental units come in handy in situations like naturally isolated areas such as high altitudes or dense forests, military and missionary programs or disaster situations.[29] Portable systems are smaller and more compartmentalized than mobile vehicle systems. They can easily be transported, are time efficient and relatively less equipments are required. Overhead cost benefit is also an advantage when considering a portable system over a mobile van.
The HRH Princess Maha Chakri Sirindhorn Mobile Dental Service is an excellent example showing the successful implementation of portable dental devices. For this program, the Department of Community Dentistry had produced portable units with the help of Thai Dental Product Company. Their design included compressor, ultrasonic scaler with saliva ejector, an aerator with fiber optic, low and high speed hand pieces, triple syringe and a light curing unit. These portable units were used on more than 200,000 needy students and their parents in Thailand who received quality dental care through them. Currently the program has been expanded to remote areas including the provinces of Nong Khai, Sisaket, Surin, Chaiyaphum, Petchburi, Uttaradit, Nakorn Panom and Mukdahan.[30] One model provided dental services using portable dental units for the geriatric population.[24] The model suggested the method of setting up mobile dental practice in settings like long-term care institutions. Initially, the mobile practice served St. Peter’s Chronic Care Hospital and it has since grown incrementally. A total of 20 institutions were served between 1996 and 2000. A total of 587 dental procedures were performed on 192 patients at the main center at St. Peter’s Hospital in the year 2000.[24] An excellent example of portable dentistry dedicated to special groups is the WE CARE program that focused on human immunodeficiency virus positive clients attending 3 community-based organizations in Harlem, Washington Heights and midtown Manhattan. WE CARE served 283 patients between July 1999 and July 2000.[31] An alternate mode of delivery of dental care is the Miles of Smile program. It is a collaboration between the University of Missouri–Kansas City School of Dentistry, the Olathe School District and an Extended Care Permit I dental hygienist. The program provided school–based services to disadvantaged children in four elementary schools. Dental hygiene students, supervised by a dental hygiene faculty member with an extended care permit, provided comprehensive preventive oral health-care. Services included prophylaxis, radiographs, sealants, fluoride varnish, oral health education and nutritional counseling to 339 children during the year 2008-2009.[32] This program collectively worked to provide school based services to the disadvantaged children in four Title I schools using community collaborative practice oral health model and teledentistry. The various portable dental services discussed above highlight the utility of portable dental services to cater to the oral health needs of children, special groups, as well as underserved population in remote rural areas and urban slums. The disadvantage of portable dental services is relatively limited armamentarium, which may limit the ability to offer comprehensive care and management of patients with severe behavioral and medical problems. Besides this, the set up looks messy with wires lying on the floor and the sound produced by the compressor, which most often is placed in the treatment vicinity may be irritating to the operator as well as the patient.
Mobile Portable Hybrid system is hybrid of a fixed site dental clinic and a mobile van model, in which portable equipment are loaded. The systems can either be a dental trailer full of portable equipments, which is parked at a site to set up the equipment or a complex system of various units that are transported by truck and transferred into a fixed facility.
Apple Tree Dental system delivers its services to people with special needs in Minnesota, USA. It operates in the Minneapolis/St. Paul Twin Cities area, Hawley, Madelia and Rochester. “Multi-Site Delivery Vehicle” truck holds up to three mobile offices at one time. Services are provided to lowincome families and children, persons with disabilities and the frail elderly; 75% of the patients are Medicaid enrolees. Mobile offices with multiple units have the advantage of “swapping out” of equipments needing repair or maintenance without affecting the operation. Treatment time is not compromised due to waiting for repairs.[33] The USC Mobile Clinic is being operational since 45 years. It has delivered dental care services to over 85,000 children from low-income families in California and Mexico. It operates in 14 sites, seven in the urban surroundings of the Los Angeles Area and seven in the rural areas of Kern County. During the academic year 2004-2005, 3rd and 4th year dental, dental hygiene students and pediatric dental residents provided more than 1550 procedures for about 1200 patients. A typical clinic can accommodate 90-120 pediatric patients. More than 90% of the children visiting the USC Mobile Clinic saw a dentist for the first time, which suggests the importance of this program.[33] The Smile mobile is a fully equipped dental clinic on wheels. It was first introduced in 1967 by Eastman Dental Center with the intention to focus on disadvantaged communities. It serves its purpose by providing 100% of its service to underserved populations in the Rochester and surrounding rural areas. Fifteen of the 38 elementary schools in the Rochester City School District are served by the Smile mobile program. Over the last 2 years, it provided services to over 5400 urban and rural pre-school and school-aged children.[33] The mobile portable hybrid systems offer holistic care to an extensive underserved population through an interdisciplinary approach and maximize efficiency by taking advantage of both mobile and portable dental services. The major disadvantages are high cost of initial implementation and maintenance.
Mobile and portable dental services in developing countries and India
A study was conducted to assess the satisfaction with school dental service provided through mobile dental squads in Selangor, Malaysia under four domains of satisfaction namely patient personnel interaction, technical competency, administrative efficiency and clinical set up. The program served its purpose in extending the oral health services to the needy school children and study revealed that 62% of the beneficiaries were satisfied with the services offered.[19] Sri Lanka shares most of the oral health problems common to other developing countries. Dental care is delivered free through hospital dental clinics to adults and school clinics to children. Field medical staff, village health volunteers, religious leaders, school-teachers, traditional medical practitioners and senior students in schools are deeply involved in oral health promotional activities. The traditional concept of health-care delivery filtering through a number of layers has been replaced by an upward movement initiated by the people. Mobile dental clinics or portable equipments were used to set up temporary dental centers in remote areas.[29] A study was conducted to describe the utility of mobile dental unit for providing basic oral healthcare services in Lucknow, India. The program was a collaborative effort of WHO and Government of India. The program operated from September 2008 to May 2009. Mobile dental unit provided its services in school and community settings. A total of 2928 minor dental treatments were performed in the mobile dental unit. Treatment included oral prophylaxis, extractions, restorations (glass ionomer cement and Silver alloy fillings) and fluoride application. It was seen that mobile clinic was able to deliver treatment to significantly higher proportion of patients as compared with CHC. The beneficiaries of the program opined that such services should continue as it offered some basic dental care for the disabled population, children, elderly and females in the village on the site.[34] Faith works India has initiated a project titled “healing touch – a mobile health-care project of specialists for the needy” in collaboration with the Catholic Church Caritas – Goa, India. The mobile clinic was successfully used to provide quality medical and dental care. The program offered an entire range of medical and dental services to the needy population. This program is an example to highlight how mobile dental clinics can be used to merge the health and oral health services. The program highlights the role of non-governmental organizations in promoting health and oral health.[35]
A study conducted in rural areas of Delhi, India, suggested a good model to provide dental services in every section of the community. A mobile dental clinic was used to provide the onsite dental care to the elderly individuals. Portable dental units were installed in each health center to provide the required services. Though the services were available to the entire population in the area, the utilization was found to be poor. This highlights the need to consider the perceived needs of the population and to create awareness among the beneficiaries about the usefulness of such services. The program providers proposed the following recommendations to improve the effectiveness of such programs:
• Recruit more number of dental health workers
• Provide every type of dental service
• Conduct various dental health programs more often
• Every patient should be given sufficient time and
• Publicize the program.[36]
The limited studies conducted to evaluate the cost-effectiveness of mobile and portable dental services in comparison with fixed private and public clinics have found mobile dental clinics to be more cost effective than fixed clinics. Besides costeffectiveness, mobile and portable dental services offer the advantage of overcoming some of the physical and cultural barriers to oral health-care.[37-39]
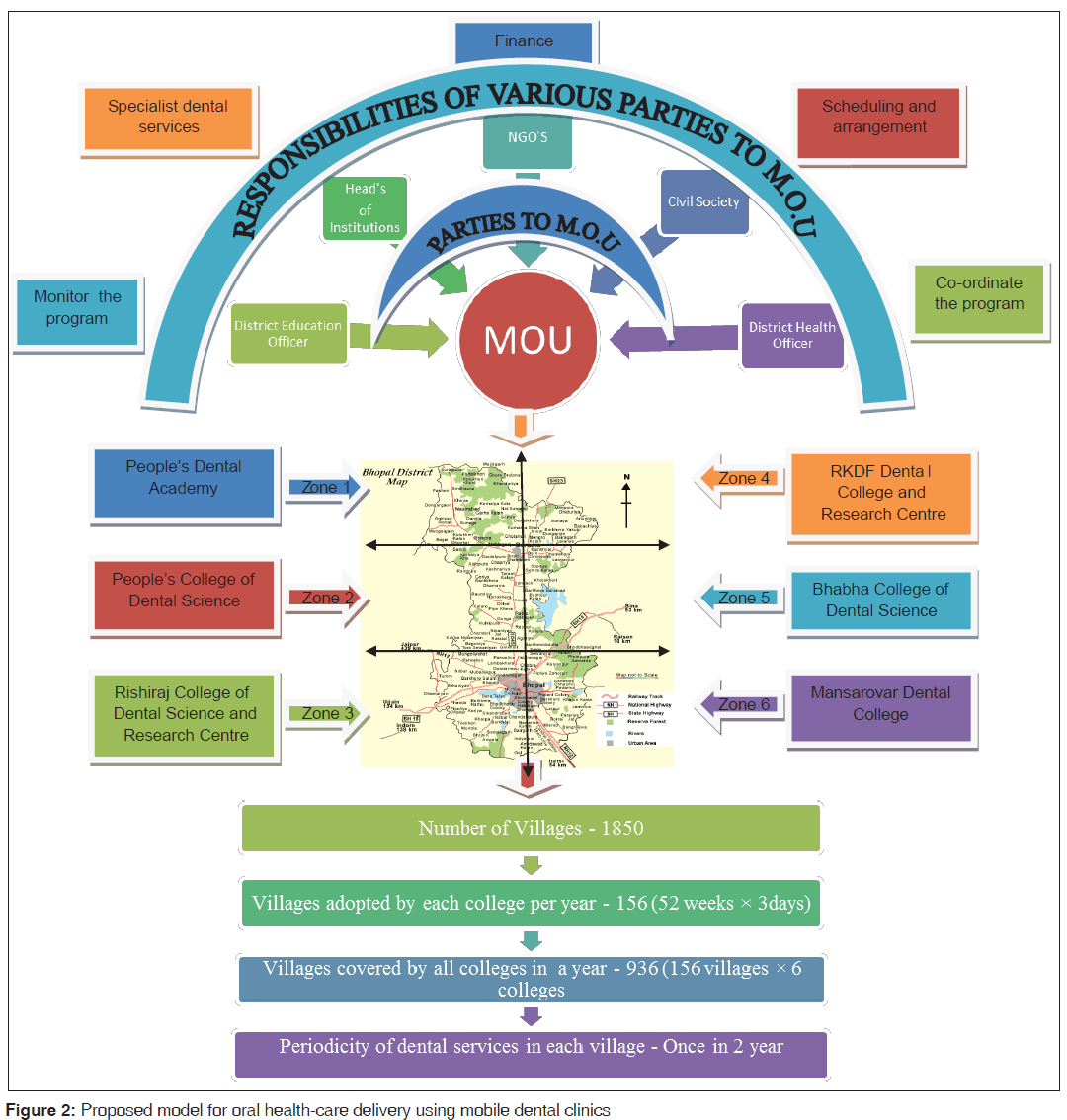
Proposed model for oral health-care delivery using mobile dental clinics for the population of a district in India
Though, there are some disadvantages of mobile and or portable dental services in oral healthcare delivery, their potential advantages in providing basic dental care surpass the drawbacks. With the collaboration of other sectors, it is possible to overcome the barrier of financial considerations, which seems to be a major setback for these programs. The principal unit of administration in India is the district under a collector. A proposed model for offering oral health services using mobile and portable dental units in Bhopal District is suggested here, keeping in mind the increasing prevalence of oral diseases among the rural population, school children and urban slum dwellers, which are denied of an access to basic dental services due various physical and cultural constraints.
• Bhopal District has approximately 1850 villages. Most of these villages have schools and they lack an access for even the basic oral health services.
• Bhopal District has six dental institutions for training undergraduate students. It is mandatory to have a mobile dental clinic with a portable dental chair in each such institute as per Dental Council of India (DCI) regulations. So, we assume that there are at least six mobile and portable dental units in the district.
• A memorandum of understanding (MOU) has to be developed between these dental institutions and the NGOs to execute the program in a prescheduled manner so that every institution will have fixed number of villages to be covered in an academic year without overlapping. The district collector (DC), district health officer (DHO), district education officer (DEO), the heads of the dental institutions, representatives of the NGOs and local civil societies should be made the parties to the MOU.
• The roles and responsibilities of each party in the MOU should be specified. The DC, DHO and DEO may coordinate the entire program with close monitoring on the monthly progress. The dental institutions may offer onsite and specialist dental services through referral and teledentistry. The NGOs may finance and publicize the program, local civil societies to schedule and make local arrangements for the successful implementation of the program.
• If one mobile dental clinic works for 3 days in a week (every alternate day in a week) covering a new village every time, then total number of villages covered by each institute per year will be 156 (52 weeks × 3 days/week).
• Total number of villages covered by all these colleges together every year will be 936 (156 villages × 06 colleges).
• In this way, all the villages can be covered within 2 years and thus, periodicity of dental services in each village will be once in every 2 years. The diagrammatic presentation of this proposed plan is depicted in Figure 2.
• The services when offered in the school premises in these villages will enable the service providers to cover the school children as well as rural population.
• The program may be expanded on the remaining days of week to cover the underserved population in urban slums.
However, the limitation of this model is that treating every villager for his/her basic oral healthcare needs in 1 day is nearly impractical. Also, it would be unethical to provide incomplete treatment in the hope to cover maximum population within a village. It would be much better to give priority in carrying out treatment for those individuals who require emergency services such as extractions, pus drainage etc., and if time permits, then restorations can also be carried out. Another team can carry out the screening procedure of the villagers. Referrals can be made for those conditions that require elaborate treatments such as Root Canal Treatments, Fabrication of Complete Denture, etc., to any nearby dental hospital or clinic. Most important function that the Mobile Dental Unit can fulfill is to create awareness in the community. Mobile dental clinics serve as a potential tool to be explored for school dental health programs in developing countries like India, which lack organized school health programs. Offering treatments in their own set up can do a lot in gaining the confidence of children than blanket referral. When children watch others being treated, it will definitely alleviate any apprehensions they may have on dental procedures.[40] It also helps in building a positive attitude towards dentistry, which may further motivate them to avail the dental services through referrals. Organized school health programs can combine the general and oral health promotion programs. Oral health messages along with health messages can be reinforced throughout the school years and this may influence the development of healthy life-style and behaviors among children. Schools provide a platform for promoting health and oral health not only for the school children, but also for the school staff, family and members of the community as a whole.[41] Besides, the school-based model has several distinct advantages. First, procedures such as screening, preventive services and scaling can be accomplished by dental auxiliaries such as dental hygienists, school dental nurse and dental therapists,[42] thus reducing the requirement of additional dentists. Second, there is a significant reduction in the unit cost of providing dental care to children. Third,[42] the school model does not require parents to take their children to dental clinics. This plays a major role in low-income areas, where social and economic factors are prime concern for single-parent families. Fourth and most importantly, these programs are expected to improve children’s oral health. The primary advantage of the school-based model is to address issues regarding access and oral health disparities.[42] The undergraduate students can be utilized for the purpose of screening and to offer preventive services to the needy children under supervision. This has the dual advantage of training the undergraduates to treat underserved populations in social settings and offering the basic services to the populations, who otherwise would not have received any care at all.
A qualitative research explored dentists’ perceptions of the use of portable dental units in community outreach programs in Iran. Qualitative semi-structured interviews were conducted by one interviewer, among seven dentists, two specialists and 11 final-year dental students who had experience with portable dental units. The predominant view most noted within interviews was that the portable units were very useful for the community outreach programs, with two subcategories of serviceability and access to oral health.[43]
The portable dental services generally less expensive, more accessible and less susceptible to mechanical difficulties,[44] can increase the awareness of the practicing dental community,[45] the oral health education to the elderly, children and their families may increase the value placed on preventive dental care[46] and improve the community oral health status.[47]
Disadvantages include dependency upon electricity meaning the device is not completely self-sufficient. Portable units may not be appropriate for periodontal treatment or complex oral surgeries. Portable dental systems may also be incapable of delivering all the services provided by mobile dental systems, like endodontic procedure.[48] Adequate dental services are not available once the mobile or portable dental units leave the facility.[49] Until permanent dental settings can be implemented in every long-term-care facility, mobile and port-able dentistry can provide dental care for the patients with access problems.[50] Efforts to promote portable dental chairs and dental vehicles will be necessary to convince both the public and the government to provide funding for these types of services.
In this way, the mobile dental services, if implemented with willingness to serve, can create awareness to such an extent that the unfelt needs may become felt needs and the felt needs become demands. It can be hoped that oral health of people will improve by successful implementation of mobile and portable dental services. This proposed plan highlights the importance of private and public partnership for the promotion of oral health.
Summary and Conclusion
India is a developing country with an extensive rural population (68.8%). Children less than 18 years constitute about 40% of the population.[51] Approximately, 23.5% of the urban population resides in urban slums. The extensive rural population, school children and urban poor are denied of even the basic dental services, though there is continuous advancement in the field of dentistry. This in fact is responsible for the upward trend in oral diseases in spite of improving economy and rising dental manpower. State health services in developing countries like India offer medical and dental services to the masses through CHC and primary health centers (PHC), with no significant improvement in the existing scenario. This national problem can be dealt with by offering promotive and preventive dental services using mobile and portable dental services.
Mobile and portable dental units are an effective and efficient way to take the sophisticated dental services to the doorsteps of the rural masses, school premises and urban slums through optimal utilization of dental institutions, dentists and dental auxiliaries. Since, the district under a collector is the principal unit of administration in India; the model proposed depicted how a district level oral health-care program may be implemented using mobile and portable dental services.
In the districts lacking adequate number of dental institutions, there is an immediate need to strengthen the existing dental infrastructure by attaching a mobile and portable dental unit with one qualified dentist, two dental hygienists for each PHC and CHC. These mobile and portable dental units at PHCs and CHCs may be utilized to offer onsite emergency services with referral to the fixed clinics for follow-up and specialist care in the same manner as depicted in the model. The model when applied utilizing the services of the school teachers, dental hygienists, health-care workers such as village health guides, trained dais, ASHA and Anganwadi workers may play vital role in promoting health as well as oral health of the underserved. This collaboration between medical and dental service providers could reduce infrastructure and transportation charges. Though, the mobile and portable systems have some practical difficulties such as financial considerations, the lack of separate national oral health policy, organized school dental services and evidence based literature highlighting the effectiveness of such programs in developing countries like India necessitates the pilot testing of the proposed model in some districts. The program may be implemented on national basis by categorizing the states/districts into high, medium and low priority areas based on remoteness and access to medical/ dental facilities. This pragmatic model will be pilot tested with a follow-up survey to determine its feasibility, potential advantages and disadvantages in Bhopal District, India. The model, if found to be effective may be used to offer basic health as well as oral health-care services to an extensive underserved population in the country. The mobile dental services may also be utilized to implement telemedicine and teledentistry services. The professional dental organizations like Indian Dental Association and DCI should have a strong motive to translate this into reality.
The present review discussed some of the mobile and portable dental service programs implemented in some developed and developing countries highlighting the urgent need for such programs to promote the oral health of an extensive underserved population in India. The review of the published literature suggests that there is an immediate need for well-conducted studies and systematic reviews on the effectiveness of mobile and portable dental services in developing countries.
Acknowledgements
First and foremost I offer my sincerest gratitude to my supervisor, Resp. Dr. Chandrashekar BR, who has supported me throughout my work with his patience and knowledge. The good advice and support of Resp. Dr. Pankaj Goel, Professor and Head of the Department of Public health dentistry, has been invaluable on both an academic and a personal level, for which I am extremely grateful. I am also thankful to Resp. Dr. Sudheer Hongal and Resp. Dr. Manish Jain who showed their kind concern and consideration regarding my academic requirements.
References
- Osotimehin B. UNFPA report. In: Kollodge R, editor. State of World Population 2011. United Nations Population Fund, New York, ©UNFPA/Pedro Sá da Bandeira UNFPA; 2011.
- Ahuja KN, Parmar R. Demographics and current scenario with respect to dentists, dental institutions and dental practices in India. Indian J Dent Sci 2011;3:8-11.
- India Factsheet Economic and Human Development Indicators. Available from: http://www.undp.org/ content/dam/india/docs/india_factsheet_economic_n_hdi. [Last cited on 2011 Aug 25].
- Chandramouli C. Rural urban distribution of population. Census of India; 2011. Available from: censusindia.gov. in/2011-prov-results/paper2/.../Rural_Urban_2011.pdf. [Last cited 2013 May 20].
- Press Information Bureau, Government of India. Available from: http://www.pib.nic.in/newsite/erelease. aspx?relid=71733. [Last cited on 2013 May 24].
- Singh A, Purohit B. Targeting poor health: Improving oral health for the poor and the underserved. Int Aff Glob Strategy 2012;3:1-6.
- Park K. Health care of the community. In: Textbook of Preventive and Social Medicine. 21st ed. Jabalpur, Madhya Pradesh, India: Bhanot Publication; 2011. p. 841-3.
- National Health Policy 2002. Available from: http://www. mohfw.nic.in/NRHM/Documents/National_Health_ policy_2002.pdf. [Last cited on 2013 May 24].
- Grewal H, Verma M, Kumar A. Prevalence of dental caries and treatment needs amongst the school children of three educational zones of Urban Delhi, India. Indian J Dent Res 2011;22:517-9.
- Bagramian RA, Garcia-Godoy F, Volpe AR. The global increase in dental caries. A pending public health crisis. Am J Dent 2009;22:3-8.
- Mathur B, Talwar C. National Oral Health Survey and Fluoride Mapping 2002-03. New Delhi, India: Dental Council of India; 2004.
- Shah N, Pandey RM, Duggal R, Mathur VP, Rajan K. Oral Health in India: A Report of Multi Centric Study. New Delhi, India: Directorate General of Health Services, Ministry of Health and Family Welfare, Govt. of India and World Health Organization Collaborative Program; 2007.
- Dhar V, Jain A, Van Dyke TE, Kohli A. Prevalence of dental caries and treatment needs in the school-going children of rural areas in Udaipur district. J Indian Soc Pedod Prev Dent 2007;25:119-21.
- Saravanan S, Kalyani V, Vijayarani MP, Jayakodi P, Felix J, Arunmozhi P, et al. Caries prevalence and treatment needs of rural school children in Chidambaram Taluk, Tamil Nadu, South India. Indian J Dent Res 2008;19:186-90.
- Chandra Shekar BR, Reddy C. Oral health status in relation to socioeconomic factors among the municipal employees of Mysore city. Indian J Dent Res 2011;22:410-8.
- Chandra Shekar BR, Reddy CV, Manjunath BC, Suma S. Dental health awareness, attitude, oral health-related habits, and behaviors in relation to socio-economic factors among the municipal employees of Mysore city. Ann Trop Med Public Health 2011;4:99-106.
- Petersen PE. Strengthening the prevention of oral cancer: The WHO perspective. Community Dent Oral Epidemiol 2005;33:397-9.
- Hamilton J. Mobile Dentistry: Entrepreneurial Boom Spurs Debates. AGD Impact 2007; 35(12): 38-46.
- Othman N, Razak IA. Satisfaction with school dental service provided by mobile dental squads. Asia Pac J Public Health 2010;22:415-25.
- A compilation of the Indiana code and Indiana administrative code. Indiana: Indiana State Board of Dentistry; 2011.Available from: www.in.gov/pla/files/2011_ISDB(2).pdf [Last cited 2013 Sept 12].
- Dental equipment and supply [Internet Source]. Office of Medical History, US Army Medical Department. Available from: http://history.amedd. a r m y . m i l / c o r p s / d e n t a l / w w i i / c h a p t e r v _ w w i i . html. [Updated on 2008 Sep 12; Cited on 2012 May 10].
- Day KC, Doherty JM. Celebrating 75 years of dental public health in Virginia. Va Dent J 1996;73:8-11.
- Carr BR, Isong U, Weintraub JA. Identification and description of mobile dental programs – A brief communication. J Public Health Dent 2008;68:234-7.
- Morreale JP, Dimitry S, Morreale M, Fattore I. Setting up a mobile dental practice within your present office structure. J Can Dent Assoc 2005;71:91.
- Lundberg K, Ignacio CR, Ramos CM. The mobile care health project: providing dental care in rural Hawaii communities. Glob J Community Psychol Pract 2011;1:32-6.
- Jackson DM, Jahnke LR, Kerber L, Nyer G, Siemens K, Clark C. Creating a successful school-based mobile dental program. J Sch Health 2007;77:1-6.
- Burtner AP, Dicks JL. Providing oral health care to individuals with severe disabilities residing in the community: Alternative care delivery systems. Spec Care Dentist 1994;14:188-93.
- Austin LD. Mobile dental health units: a model for improving access to care. Access 2011; 25(4):18-9.
- Lamb R. Portable Mission Dentistry. 4th ed. Broken Arrow, Oklahoma: World Dental Relief; 2008.
- The compact dental unit: mobile miracle in dentistry [Internet]. Available from: http://www.dt.mahidol.ac.th/ en/Direction/2/TheCompact.pdf. [Cited on 2012 May 11].
- Zabos GP, Trinh C. Bringing the mountain to mohammed: A mobile dental team serves a community-based program for people with HIV/AIDS. Am J Public Health 2001;91:1187-9.
- Simmer-Beck M, Gadbury-Amyot CC, Ferris H, Voelker MA, Keselyak NT, Eplee H, et al. Extending oral health care services to underserved children through a school-based collaboration: Part 1: A descriptive overview. J Dent Hyg 2011;85:181-92.
- Mobile-Portable Dental Manual. National Maternal and Child Oral Health Resource Center. [Internet Manual]. Phoenix, Arizona: TraCorp. Available from: http://www.mobile-portabledentalmanual.com. [Cited on 2012 May 10]
- Saimbi CS, Dixit J. Studying the utility of mobile dental van for basic oral treatment in the rural population around Lucknow. Project Report submitted by faculty of dental Sciences, CSM Medical University, Lucknow, India. GOI-WHO Collaborative Programme; 2008-2009.
- Healing Touch - A Mobile Healthcare Project of Specialists for the Needy. India: Faith Works. Available from: http://www. faithworks.co.in/healing_touch.php [Cited on 2012 May 12].
- Goel P, Singh K, Kaur A, Verma M. Oral healthcare for elderly: Identifying the needs and feasible strategies for service provision. Indian J Dent Res 2006;17:11-2.
- Bagramian RA. A 5-year school-based comprehensive preventive program in Michigan, U.S.A. Community Dent Oral Epidemiol 1982;10:234-7.
- Doherty N, Hussain I. Costs of providing dental services for children in public and private practices. Health Serv Res 1975;10:244-53.
- Tianviwat S, Chongsuvivatwong V, Birch S. Optimizing the mix of basic dental services for Southern Thai schoolchildren based on resource consumption, service needs and parental preference. Community Dent Oral Epidemiol 2009;37:372-80.
- Roberts JF, Curzon ME, Koch G, Martens LC. Review: Behaviour management techniques in paediatric dentistry. Eur Arch Paediatr Dent 2010;11:166-74.
- World Health Organization. Status of school health. Report of the school health working group and WHO expert committee on comprehensive school health education and promotion, Geneva, 1996. Available from: www.who.int/entity/school_ youth_health/media/en/87.pdf [Last cited 2013 Sept 13].
- Bailit H, Beazoglou T, Drozdowski M. Financial feasibility of a model school-based dental program in different states. Public Health Rep 2008;123:761-7.
- Nilchian F, Sahlabadi A, Skini M. Portable dental chairs and their role in assisting the community outreach program - A qualitative approach. J Dent Tehran Univ Med Sci 2013;10:233-9.
- Krust KS, Schuchman L. Out-of-office dentistry: An alternative delivery system. Spec Care Dentist 1991;11:189-93.
- Dane JN. The Missouri elks mobile dental program – Dental care for developmentally disabled persons. J Public Health Dent 1990;50:42-7.
- Warren JJ, Kambhu PP, Hand JS. Factors related to acceptance of dental treatment services in a nursing home population. Spec Care Dentist 1994;14:15-20.
- Bolden AJ, Kaste LM. Considerations in establishing a dental program for the homeless. J Public Health Dent 1995;55:28-33.
- de Baat C, Bruins H, van Rossum G, Kalk W. Oral health care for nursing home residents in The Netherlands – A national survey. Community Dent Oral Epidemiol 1993;21:240-2.
- Herman NG, Rosenthal M, Franklin DM. Delivery of comprehensive children’s dental services using portable dental clinics in NYC public schools. A six-year analysis. N Y State Dent J 1997;63:36-41.
- Jacoby T. Theory and practice of mobile dentistry. Dentistry 1990;10:20-1, 26.
- Chandrashekar BR, Suma S, Kiran K, Manjunath BC. The use of school teachers to promote oral hygiene in some secondary school students at Hyderabad, Andhra Pradesh, India: A short term prospective pilot study. J Fam Community Med 2012; 19: 184-9.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.