Mucoepidermoid Lung Carcinoma in Child
Citation: Jayaprakash KS, Kishanprasad HL, Ismail M, Raju M, Dasguptha A. Mucoepidermoid lung carcinoma in child. Ann Med Health Sci Res 2014;4:276-8.
Abstract
Mucoepidermoid carcinoma (MEC) is a rare malignant tumor arising from the bronchial gland. A case of 6‑year‑old male child who presented with fever, hemoptysis and wheezing since 1month is reported. Chest X‑ray showed features suggestive of foreign body with post‑obstructive pneumonia and was treated for the same with medication without much improvement. Subsequently computerized tomography scan chest was carried out, which showed oval mass with speculated margin in right hilar region with distal segmental atelectasis. Bronchoscopy showed small growth with nodularity in the apical segmental bronchus of the right lower lobe with mucosal erosion and hence carried out broncho‑alveolar lavage showed few atypical squamous cells. Patient underwent right lower lobectomy, which showed a grey white oval mass with solid and cystic areas in the right hilar region with extension in to the lung parenchyma. Histology of the tumor showed mixed solid and cystic areas with sheets of epidermoid cells and mucus‑filled cysts of irregular size. Areas of solid growth were composed of squamoid and intermediate cells. Hence, the final diagnosis of mucoepidermoid carcinoma (MEC) intermediate grade of the lung was made. Early diagnosis can be accomplished if the clinician is alert to persistent pneumonia, coughing and tumor obstruction on image studies. MEC is a comparatively rare low‑grade tumor, which reportedly carries a good prognosis with early surgical intervention.
Keywords
Lobectomy, Lung, Mucoepidermoid carcinoma, Periodic acid-Schiff
Introduction
Mucoepidermoid carcinoma (MEC) is a rare malignant tumor arising from the bronchial gland, with incidence of 0.1-0.2% of all lung cancers.[1-3] It is seen in young patients as compared with most of other lung cancers.[2-4] This tumor originates from glandular tissue identical with salivary glands located in the submucosa of the trachea and bronchus; hence, it is included among carcinomas of salivary gland types along with adenoid cystic carcinoma and epithelial-myoepithelial carcinoma according to the World Health Organization classification of lung cancer.[2-5] Fortunately, low-grade malignant tumors are much more common than high-grade ones. Children, especially have an excellent prognosis if low-grade tumors can be resected completely.[2-5] We report a rare case of mucoepidermoid lung carcinoma-right lung, occurring in a 6-year-old male child who presented with fever, hemoptysis and wheezing since1 month. Therefore, in cases of unclear obstructive symptoms or recurrent pneumonias, a chest radiograph should be used to identify suspicious signs followed by further diagnostic steps including computerized tomography (CT) and bronchoscopy.
Case Report
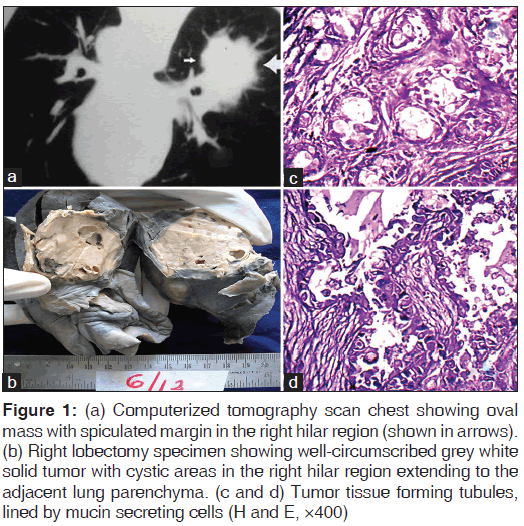
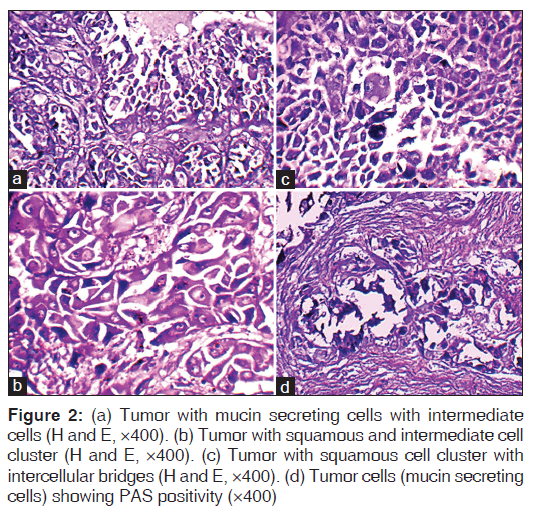
A 6-year-old male child was presented with fever, cough, hemoptysis and wheezing since1 month. Chest X-ray showed features suggestive of foreign body with post-obstructive pneumonia-left lung and was treated for the same with medication without much improvement. Family history and developmental history was unremarkable. Routine hematological, biochemical and microbiological investigations were unremarkable. Subsequently CT scan chest was carried out, which showed oval mass with speculated margin in right hilar region [Figure 1a, shown in arrows] with distal segmental atelectasis. Bronchoscopy showed small growth with nodularity in the apical segmental bronchus of the right lower lobe with mucosal erosion and hence carried out bronchoalveolar lavage showed few atypical squamous cells. Post-bronchoscopy sputum was unremarkable. CT abdomen and pelvis showed no evidence of metastatic deposits. Hence, patient underwent left lower lobectomy. The right lower lobectomy showed a grey white oval mass with solid and cystic areas in the right hilar region with extension in to the lung parenchyma [Figure 1b]. Histology of the tumor showed mixed solid and cystic areas with sheets of epidermoid cells and mucus-filled cysts of irregular size [Figure 1c and d]. Areas of solid growth were composed of squamoid and intermediate cells [Figure 2a and b]. Epidermoid cells showed inter cellular bridges [Figure 2c]. Cysts were lined by columnar cells with mucin-rich cytoplasm. These cells were positive for periodic acid-Schiff stain [Figure 2d]. Hence, the final diagnosis of mucoepidermoid carcinoma-intermediate grade of right lower lobe was made. Lymph-vascular invasion and lymph node metastasis were negative. The post-operative course was good. Since the tumor was low-grade, no adjuvant treatment was administered. Patient had no signs of tumor recurrence for 1 year, to date, since the resection of the tumor.
Figure 1: (a) Computerized tomography scan chest showing oval mass with spiculated margin in the right hilar region (shown in arrows). (b) Right lobectomy specimen showing well‑circumscribed grey white solid tumor with cystic areas in the right hilar region extending to the adjacent lung parenchyma. (c and d) Tumor tissue forming tubules, lined by mucin secreting cells (H and E, ×400)
Figure 2: (a) Tumor with mucin secreting cells with intermediate cells (H and E, ×400). (b) Tumor with squamous and intermediate cell cluster (H and E, ×400). (c) Tumor with squamous cell cluster with intercellular bridges (H and E, ×400). (d) Tumor cells (mucin secreting cells) showing PAS positivity (×400)
Discussion
MEC of the lung is an uncommon tumor type, arising from minor salivary gland tissue of the trachea bronchial tree. The clinical behavior is varied. This occurs in patients with an age range from 3 years to 78 years. Most of these cases are reported in the pediatric population, accounting for 10% of primary lung tumors in this age group.[1,2,4,6] Our case occurred in a 6-year-old child. Because of the typical pattern of involvement of large airways, the clinical symptoms and signs of bronchial MEC include cough, hemoptysis, bronchitis, wheezing, fever, chest pain and rarely, clubbing of the fingers. The clinical and radiographic differential diagnosis usually includes asthma, pneumonia, atelectasis, middle lobe syndrome and pleural effusion. Recurrent pneumonia in the same region of the lung should raise clinical suspicion of an endobronchial lesion or mass, such as mucoepidermoid carcinoma.[1] Because MECs are most commonly found in the segmental or lobar bronchi and symptoms of airway irritation or obstruction are common, hence bronchoscopic examination for diagnosis is essential.[1,2]
These carcinomas usually presents as an intraluminal mass producing luminal occlusion.[3,4] Macroscopically, it appears as an exophytic intra bronchial mass with intact or ulcerated bronchial mucosa. In our case, bronchoscopy showed small growth with nodularity in the apical segmental bronchus of the right lower lobe and bronchoalveolar lavage showed few atypical squamous cells. Microscopically, the tumor cells are located in the submucosa of the large bronchi and comprise of three components: Mucus-secreting, squamous and intermediate cells.[3,4,6,7] These three cell types can be organized in to different patterns including glands, tubules, cysts, nests and solid areas. The mucus-secreting cells are usually large and have light blue mucinous cytoplasm. The squamous cells may be admixed with the mucus-secreting cells and intermediate cells or they can form small nests of their own. The squamous cells shows inter cellular bridges. The intermediate cells usually do not demonstrate specific differentiation and are characterized by a polygonal shape, a centrally or eccentrically located bland nucleus and relatively abundant amphophilic or slightly eosinophilic cytoplasm. Low-grade malignant tumors have mostly cystic components. Mild cytologic atypia can be seen, but mitosis are rare.[2,4,6] Our case was MEC of the lung-intermediate grade with all three components of mucous, intermediate and squamous cells.
Metastasis to regional lymph nodes is distinctly unusual. High-grade tumors more commonly show areas of solid growth. Atypia, mitotic activity and necrosis are characteristic and regional lymph node involvement is more frequent in these tumors. This high-grade variant is difficult to distinguish from adenosquamous carcinoma.[2,5-7]Cytokeratin (CK-7) and thyroid transcription factor 1 (TTF-1) may be useful in differentiating MEC of the bronchus from primary lung adenocarcinoma. MECs of the bronchus are negative for TTF-1, but the tumor cells are positive for CK-7.[4,6,7] In our case, immune marker study was not carried out due to limited resources.
Surgical intervention is the treatment of choice for patients with MECs if they have no distant metastases or unresectable lesions.[4,6,7] Low-grade tumors should be removed completely for the best therapeutic effect. Anatomical resection with lobectomy and mediastinal lymph node dissection is efficient and simple.[2,4,6] Patients with central lesions might require more aggressive approaches, such as sleeve resection or pneumonectomy.[5-7] The surgeon should plan a conservative resection with bronchoplasty or sleeve resection for a localized tumor diagnosed as MEC.[4,5,7] Sometimes the tumor originates at the carina and a complicated carinal resection with reconstruction might be needed. Endoscopic resection is not recommended because of difficulty in control of hemorrhage and incomplete resection. Few case reports of successfully managed MECs with bronchoscopic neodymium-yttrium aluminum garnet laser surgery.[5-7] Although such laser surgery is less invasive than surgical resection and preserves lung function, further long-term follow-up is needed for possible tumor recurrence. Our case was managed with right lower lobectomy with good outcome. Since the tumor was low-grade, no adjuvant treatment was administered.
Histological grade, tumor staging and complete tumor resection are important prognostic indicators.[3,5-7] Patients with low-grade MEC can be cured following complete resection and lobectomy with complete regional lymph node dissection with 5-year survival rate of 80%.[1,3,5-7] However, high-grade tumors usually have a worse prognosis with 5-year survival rate of 31%.[6,7] Our patient had no signs of tumor recurrence with 1-year of follow-up.
Conclusion
MEC of the lung is a rare type of malignancy that usually presents with obstructive symptoms. Early diagnosis can be accomplished if the clinician is alert to persistent pneumonia and cough with tumour obstruction on image studies. MEC is a comparatively rare low-grade tumor, which reportedly carries a good prognosis with early surgical intervention.
References
- Liu X, Adams AL. Mucoepidermoid carcinoma of the bronchus: A review. Arch Pathol Lab Med 2007;131:1400-4.
- Yang CS, Kuo KT, Chou TY, Lin CM, Hsu WH, Huang MH, et al. Mucoepidermoid tumors of the lung: Analysis of11 cases. J Chin Med Assoc 2004;67:565-70.
- Kitada M, Matsuda Y, Sato K, Hayashi S, Ishibashi K, Miyokawa N, et al. Mucoepidermoid carcinoma of the lung: A case report. J Cardiothorac Surg 2011;6:132.
- Heitmiller RF, Mathisen DJ, Ferry JA, Mark EJ, Grillo HC. Mucoepidermoid lung tumors. Ann Thorac Surg1989;47:394-9.
- Huang HK, Cheng YL, Chang H, Tzao C, Lee SC. Mucoepidermoid carcinoma of the lung. J Med Sci 2009;29:305-8.
- Green LK, Gallion TL, Gyorkey F. Peripheral mucoepidermoid tumour of the lung. Thorax 1991;46:65-6.
- Niggemann B, Gerstner B, Guschmann M, Paul K, Wit J, Mau H, et al. An 11-yr-old male with pneumonia and persistent airway obstruction. Eur Respir J 2002;19:582-4




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.