Neonatal Airway Obstruction from an Immature Teratoma: The Challenge of Appropriate Investigation in a Low‑resource Setting
- *Corresponding Author:
- Dr. Abdallah Y
Department of Pediatrics and Child Health, Makerere University College of Health Sciences, P.O. Box 7072, Kampala, Uganda.
E-mail: yasam786@hotmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Citation Abdallah Y, Micheal A. Neonatal airway obstruction from an immature teratoma: The challenge of appropriate investigation in a low-resource setting. Ann Med Health Sci Res 2016;6:59-61.
Abstract
Teratoma in the nasopharynx is one of the rare causes for nasal symptoms in the newborn. The present report was on a term “neonate” who had respiratory distress from a hidden teratoma. Cheaper and readily available investigation modalities including postnasal space X‑ray and examination under anesthesia revealed nothing. A postnasal space computed tomography also revealed nothing. Magnetic resonance imaging revealed a mass which was resected endoscopically and histology revealed an immature teratoma. Herein, we present the case, management challenges and literature review to emphasis that negative investigations with persistent nasal symptoms should prompt further evaluation and teratoma should be considered when encountering newborn with nasal symptoms without obvious cause
Keywords
Airway, Immature, Teratoma
Introduction
Teratomas are rare congenital tumors composed of tissues derived from the embryonic germ cell layers.[1] They may occur in the gonads and extragonadal locations. The incidence of teratoma is 1:4000 live births with the most common site being the sacrococcygeal area.[2] Head and neck teratomas are very rare accounting for < 5% of all teratomas with nasopharyngeal ones being extremely rare.[2,3] Teratoma of the nasopharynx may arise from the skull base or the posterior pharyngeal wall. Nasopharyngeal teratomas can cause tracheoesophageal obstruction,[2] and we present a case report of a neonate whose nasopharyngeal teratoma presented with airway obstruction.
Case Report
A term male neonate delivered by spontaneous vaginal delivery weighing 3.5 kg following an uneventful pregnancy and was admitted shortly after birth to the nursery with grunting respiration and cyanosis (saturation of 70% in room air), Apgar scores were 51 then 85. His mother attended antenatal clinic; she had normal booking blood and her antenatal ultrasound scans (weeks 28 and 36) were unremarkable. Clinical examination was unremarkable except for weak cry and slight resistance during the insertion of a nasogastric tube through the left nostril. A presumptive diagnosis of choanal stenosis and possible recurrent laryngeal nerve palsy were made.
The infant was placed on the continuous positive airway pressure (CPAP) in which he was comfortable on FiO2 of 21%. Chest and postnasal space X-ray were obtained and were normal.
An ear, nose, and throat surgeon were consulted, and a planned examination under anesthesia (EUA) was organized. The initial EUA revealed nothing; infant continued to need CPAP.
Head and neck computed tomography (CT) was ordered which revealed nothing [Figure 1]. Magnetic resonance imaging (MRI) which was not readily available was ordered, and it revealed a large heterogeneous enhancing lobulated mass in the left naso- and oral-pharyngeal cavity measuring 1.7 cm × 2.1 cm × 2.4 cm [Figure 2].
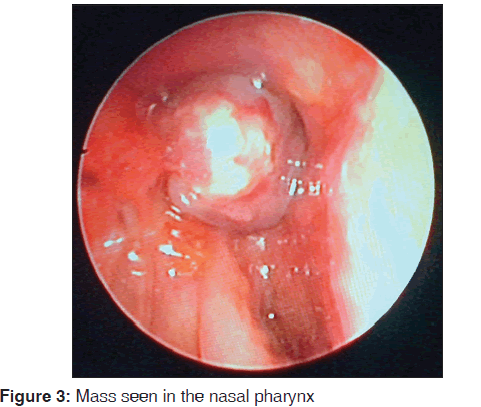
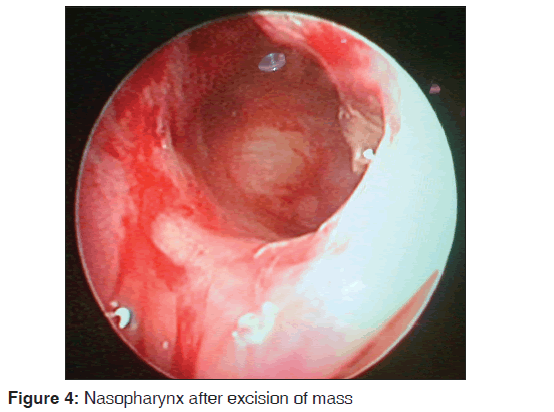
Excision of the mass was performed endoscopically [Figures 3 and 4] and the histology revealed immature teratoma. The infant was followed up for recurrence with a repeat EUA conducted at 3 months of age, and the site looked clear. Alfa-fetoprotein level was also done at 3 months and was 47.8 IU/ml which was normal for age.
Discussion
Teratoma and neuroblastoma are the most common tumors in the fetus and the newborn with the prevalence of congenital teratoma estimated at 1:4000 live births.[2] The most common site for teratomas is the sacral region[3] while nasopharyngeal teratomas are very rare.[3] Many theories have attempted to explain histogenesis of teratomas with the most popular theory suggesting displaced totipotent cells during migration from the York sack to the gonadal ridge. [1] Nasopharyngeal teratomas tend to arise from the skull base or lateral nasopharyngeal walls. Our patient’s teratoma was arising from the skull base.
Four basic histologic classification of teratomas are recognized i.e., dermoid cysts (epithelium-lined with skin elements, composed of ectodermal, and mesodermal layer), teratoid cyst (composed of all the three germ elements but poorly differentiated), true teratoma (three germ elements differentiated into specific tissue or organs), and epignathi (tumor with developmental fetal organs and limbs).
Teratomas may be identified in utero if they are very large or if it causes polyhydramnios by impeding the fetus from swallowing liquor. The mother to our patient had an uneventful pregnancy with normal obstetric ultrasound scans on two occasions. At birth, the tumor may cause respiratory embarrassment as it did in our patient in which case, the main-stay of care is prompt assessment and management of airway. Our patient was managed on CPAP to keep the airway patency.
Nasopharyngeal teratomas tend to be associated with other abnormalities, and reported ones include cleft palate, cardiac abnormalities and microcephaly.[2] It is speculated that these abnormal tissues inhibit fusion of normal tissues. The case we present had no associated abnormalities. Although nasopharyngeal teratomas may protrude through the oral or nasal cavity and associated morbidity and mortality are related to the location and size of the tumor; from our case, we learn that lack of an obvious protruding mass does not preclude the presence of teratoma.
The differential diagnosis for nasopharyngeal teratoma includes meningoencephalocele, encephalocele, glioma, neurofibroma, rhabdomyosarcoma, or hemangioma.
Imaging methods including CT scan and MRI are important; CT scan will characterize bone changes and detect intralesional calcification but the investigation modality of choice for teratoma would be an MRI which demonstrates the soft tissue characteristic of the tumor,[4] and it aids in determining the relation of the mass to other vital structures such as blood vessels. In our case, the X-ray and CT did not identify the mass, but it was on MRI. Immature teratomas such as, we found in our patient, do not have calcified structures and may be missed on X-ray and CT scan. Where resources are constrained, this can become a diagnostic dilemma. It is important that extension of the mass into the brain is ruled out before surgery and in our case, there was no intracranial extension seen on MRI.
The majority of congenital teratomas are benign although malignant ones have been reported. Teratomas that are histologically immature and those containing York sack tumor have a higher tendency for malignant transformation.[5,6] The treatment of choice is complete excision coupled with close follow-up with tumor marker assay (alpha fetal protein) and imaging.[3,5,6] Recurrence has been reported in some cases including those with incomplete resection, tumor rupture, nongonadal teratoma, especially sacral, immaturity, and raised alpha fetal protein level.[3,6] Although at 3 months, our patient did not have makers of recurrence, close follow-up is necessary.
Conclusion
• A differential diagnosis of nasopharyngeal teratoma should be considered in any newborn with persistent nasal symptoms
• Immature teratomas can be challenging to identify where resources are limited, but persistent symptoms with negative investigations should prompt further evaluation. MRI is the investigation modality of choice in identifying teratomas.
Acknowledgements
We thank the parents to our patient for their patience and acceptance for this case report to be published. We would also want to thank the nurses and doctors at International Hospital Kampala for the service they rendered to this infant during his hospital stay.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Barksdale EM Jr., Obokhare I. Teratomas in infants and children. Curr Opin Pediatr 2009;21:344-9.
- Coppit GL 3rd, Perkins JA, Manning SC. Nasopharyngeal teratomas and dermoids: A review of the literature and case series. Int J Pediatr Otorhinolaryngol 2000;52:219-27.
- Isaacs H Jr. Perinatal (fetal and neonatal) germ cell tumors. J Pediatr Surg 2004;39:1003-13.
- Robson CD. Imaging of head and neck neoplasms in children. Pediatr Radiol 2010;40:499-509.
- Marina NM, Cushing B, Giller R, Cohen L, Lauer SJ, Ablin A, et al. Complete surgical excision is effective treatment forchildren with immature teratomas with or without malignant elements: A Pediatric Oncology Group/Children’s Cancer Group Intergroup Study. J Clin Oncol 1999;17:2137-43.
- Mann JR, Gray ES, Thornton C, Raafat F, Robinson K, Collins GS, et al. Mature and immature extracranial teratomas in children: The UK Children’s Cancer Study Group Experience. J Clin Oncol 2008;26:3590-7.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.