Obsessive-Compulsive and Spectrum Disorders, A Cross Sectional Study among the Medical Students at Tertiary Health Care Centre, Kanchipuram District-Tamil Nadu
Received: 05-Jun-2023, Manuscript No. amhsr-23-101578; Editor assigned: 07-Jun-2023, Pre QC No. amhsr-23-101578 (PQ); Reviewed: 22-Jun-2023 QC No. amhsr-23-101578; Revised: 29-Jun-2023, Manuscript No. amhsr-23-101578 (R); Published: 06-Jul-2023
Citation: Sowmiya KR, et al. Obsessive-Compulsive and Spectrum Disorders, A Cross Sectional Study among the Medical Students at Tertiary Health Care Centre, Kanchipuram District-Tamil Nadu. Ann Med Health Sci Res. 2023;13:689-694.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Obsessive and compulsive disorder is a chronic psychiatric illness which has been recognized as the fourth most common global psychiatric disorder. This study was done with an objective of estimating the prevalence of probable OCD and associated spectrum disorders and to evaluate the association between socio demographic features.
Method: A cross-sectional study was conducted among 477 medical students, at a Medical College in Kancheepuram district, Tamil Nadu employing universal sampling method. The data was collected during the period from July 2022 to September 2022 using the Obsessive- Compulsive Inventory-Revised (OCI-R) scale and score of ≥21 signify probable OCD
Results: Out of the 477 study participants screened for obsessive compulsive symptoms, 183(38.4%), were males and 294 (61.6%).were females. 206 (43.2%) participants had scored above the recommended cut-off on the OCI-R (R) presenting with probable OCD. In this current study age, gender, year of study and occupation of the head of the family were significantly associated with OCD (p value of <0.05).
Conclusion: Probable OCD prevalence is high among medical students emphasizing the need to provide supportive care to the students beginning from first year especially during this COVID pandemic period.
Keywords
COVID-19; Medical students; Obsessive–Compulsive Disorder (OCD); OCD symptoms
Introduction
Obsessive-compulsive disorder is a chronic psychiatric illness which has been recognized as the fourth most common global psychiatric disorder. Obsessions are intentional thoughts which cause intrusive repetitive urges against one’s conscious awareness [1]. Resistance to such thoughts may lead to a marked escalation of anxiety or distress.Most people experience either isolated or multiple symptoms of OCD at different instances of their life that likely do not progress into full blown OCD syndrome [2]. Some patients may have either obsessions or compulsions alone; however, in most cases, both are present together [3].The prevailing behaviours are cleanliness, repetitive checking, fear of negative events, symmetrical and orderly habits, aggression, blasphemousness and sexual obsessions [2]. The latter three are more of pure obsessions [2].The grouping of obsessive-compulsive and spectrum disorders includes Obsessive-Compulsive Disorder (OCD), Hypochondriasis (unduly worried about serious illness), Body-Dysmorphic Disorder (BDD-consistently worried about appearance), Hoarding Disorder (HD-difficulty in discarding or parting with possessions), Trichotillomania (TTM-voluntary plucking of hair) and excoriation (skin-picking disorder). The Etiology of OCD is not exactly known and is likely multifactorial. Genetics attributes to 45% to 65% of OCD syndrome [4]. Certain imaging studies suggest that OCD prevails with an abnormal corticostriato- thalamo-cortical circuit [5,6].
Alongside the other etiologies, the recent outbreak of COVID-19 has also been a concerning factor for the increase in the prevalence of OCD. People are doped with the fear of viruses which led to the increasing compulsive behaviours such as repetitive washing of hands, checking temperature too often, having tablets in the fear of getting the disease.Thus environment (COVID-19 pandemic) and psychology (fear and/ or anxiety) interaction might be involved in OCD [7].People with an early age of onset have more severe symptoms of OCD added to higher rates of ADHD and bipolar disorder [8].
As the onset of OCD is mainly during adolescence with an average age of 19-20 years, all medical students, are subjected to increased risk of experiencing OCD syndrome [1]. This could be due to various reasons including but not limited to difficulty in adapting to the newer environment, fear of failure, stressful schedules and sleep deprivation. Furthermore, medical schools insist on precision and perfection of the students and working in a known contaminated zone triggers their fear towards acquiring a disease. These factors may pave the way for obsessive thoughts and compulsive actions such as being constantly meticulous, excessive washing and lack of control over thoughts which acts as a hindrance to complete one’s day to day activities. In addition, the global outbreak of COVID-19 highlighted that the healthcare providers are the most susceptible front-line workers. This led to further chaos among the mental health of the medical students. The fear of rapid transmission of COVID-19, fatality rate, lack of effective treatments and vaccines, and mass quarantine measures were all triggering factors [6].
With this background, aim of this study is to find the prevalence of probable OCD and associated spectrum disorders and to evaluate the association between socio demographic features during the COVID-19 pandemic to have forethought on early intervention, diagnosis and management.
Methodology
This cross-sectional study was conducted among medical students, during the period from July 2022 to September 2022 at a Medical College in Chennai, near Kanchipuram, Tamil Nadu. A purposive sampling method was followed, which included all medical students from first year to final year of medical college. Total of 600 undergraduate medical students, 150 from first year MBBS, 150 from Second year MBBS, 150 from Third MBBS Part I and 150 from Third MBBS Part II were contacted to study. All students who were willing to participate in the study were included by universal purposive sampling, and 477 medical students were enrolled in the study after getting their informed consent. OCI-R scale, a simplified version of OCI was used [2]. This scale is a self-reporting scale and has been translated in many languages to broaden its usage in clinical settings. It has 18 questions which has been categorized within 6 subscales depicting the prominent symptoms of OCD comprising of washing, checking, neutralizing, obsessing, ordering and hoarding. Each question has the Likert scale with a score ranging from 0-4 corresponding to the severity of the symptom. The maximum and minimum total score that can be obtained from the entire scale is 72 and 0 [6]. An individual with an OCI-R score of ≥21 may probably have OCD.Data was collected by using a structured questionnaire,which was framed in a Google sheet form and a link was passed to the medical students through social media [6]. The survey consisted of four sections. Basic details regarding their socio-demographic profile such as Age, Gender, year of the study, Family income, Occupation of the head of the family and type of family. Second section includes a set of 18 questions mentioned in the OCI-R scale, third section includes the Likert scale to assess the severity of associated spectrum disorders followed by the last section providing information about the individuals past psychiatric history and family association. Responses were collected for a span of 18 days from 2/9/2022 to 19/9/2022. Ethical clearance was obtained from the institutional ethical committee. Data was entered in Ms-Excel software and analyzed by using SPSS version 26. Descriptive statistics were seen by mean and standard deviation for numerical data, whereas for categorical data, frequency table was represented. Association between categorical variables was seen using chi-square test and difference between means was performed using independent t test considering P value equal or less than 0.05 as statistically significant.
Results
The mean age of the study participants was 20.30 ± SD 1.1 years, male students in the study were183 (38.4%), whereas females were 294 (61.6%).In the current study 436 (91.4%) study participant parents were Non health professionals, whereas majority of them belonged Nuclear family 403(84.5%) The detail of Socio-demographic characteristics of the study subjects are described in Table1.
| Variables | Frequency N=477 (%) |
|---|---|
| Gender | |
| Male | 183 (38.4) |
| Female | 294 (61.6) |
| Year of study | |
| First year | 164 (34.3) |
| Second year | 167 (35.0) |
| Third year | 146 (30.7) |
| Type of family | |
| Nuclear family | 403 (84.5) |
| Joint Family | 51 (10.7) |
| Three Generation family | 23 (4.8) |
| Occupation of head of the family | |
| Non health professional | 436 (91.4) |
| Health professional | 41 (8.6) |
Table 1: Frequency distribution of socio-demographic features of the study participants.
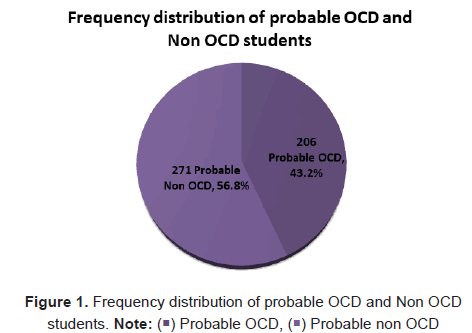
According to OCI-R, there were 206(43.2%) of them were with probable OCD whereas 271 (56.8%) of them were non-OCD persons, and need for further assessment for a definite diagnosis as shown in Figure 1.
Regarding the severity of the “obsessing symptoms” the highest percentage of students answered, “extremely or a lot” was 35.4% for the question “I find it difficult to control my own thoughts”, followed by 33.1% for the question “I am upset by unpleasant thoughts that come into my mind against my will”. 31.7% students responded extremely or a lot of for “I get upset if others change the way I have arranged the things” respectively. The frequency distribution of the students’ responses for the 18 items corresponding to OCI-R score are presented in Table 2.
| No | Questions | Not at all(%) | A little(%) | Moderately(%) | Alot(%) | Extremely(%) |
|---|---|---|---|---|---|---|
| 1 | I need things to be arranged in a particular way | 40 (8.4) | 101 (21.2) | 220 (46.1) | 88 (18.4) | 28 (5.9) |
| 2 | I get upset if objects are not arranged properly | 83 (17.4) | 194 (40.7) | 126 (26.4) | 55 (11.5) | 19 (4.0) |
| 3 | I get upset if others change the way I have arranged the things | 69 (14.4) | 146 (30.6) | 111 (23.3) | 102 (21.4) | 49 (10.3) |
| 4 | I find it difficult to touch an object when I know it has been touched by strangers or certain people | 235 (49.3) | 142 (29.8) | 65 (13.6) | 21 (4.4) | 14 (2.9) |
| 5 | I wash my hands more often and longer than necessary | 186 (39.0) | 125 (26.2) | 112 ( (23.5) | 36 (7.5) | 18 (3.8) |
| 6 | Sometimes have to clean or wash myself simply as I feel contaminated | 115 (24.1) | 147 (30.8) | 111 (23.3) | 80 (16.8) | 24 (5.0) |
| 7 | I feel that there are good and bad numbers | 222 (46.5) | 102 (21.4) | 111 (23.3) | 28 (5.9) | 14 (2.9) |
| 8 | I felt compelled to count/chant while doing a work | 245 (51.4) | 130 (27.3) | 79 (16.6) | 21 (4.4) | 2 (0.3) |
| 9 | I feel the necessity to repeat numbers, writings, speech | 192 (40.3) | 142 (29.8) | 92 (19.3) | 42 (8.8) | 9 (1.8) |
| 10 | I check things more often than necessary e.g., writing or overwriting the script | 139 (29.1) | 162 (34.0) | 97 (20.3) | 63 (13.2) | 16 (3.4) |
| 11 | I repeatedly check gas, lights and water taps even after turning them off | 123 (25.8) | 161 (33.8) | 94 (19.7) | 66 (13.8) | 33 (6.9) |
| 12 | I repeatedly check doors, windows, drawers | 174 (36.5) | 135 (28.3) | 90 (18.9) | 56 (11.7) | 22 (4.6) |
| 13 | I find it difficult to control my own thoughts | 86 (18.0) | 118 (24.8) | 104 (21.8) | 94 (19.7) | 75 (15.7) |
| 14 | I am upset by unpleasant thoughts that come into my mind against my will | 70 (14.7) | 137 (28.7) | 112 (23.5) | 81 (17.0) | 77 (16.1) |
| 15 | I frequently have nasty thoughts and having difficulty in getting rid of them | 153 (32.1) | 153 (32.1) | 89 (18.6) | 50 (10.5) | 32 (6.7) |
| 16 | I have simply saved up a lot of non-specific things eg: pen caps, tablet scraps, used masks | 280 (58.7) | 85 (17.8) | 61 (12.8) | 25 (5.2) | 26 (5.5) |
| 17 | I collect things I don’t need | 258 (54.1) | 132 (27.7) | 52 (10.9) | 22 (4.6) | 13 (2.7) |
| 18 | I avoid throwing things away because I am afraid that I might need them later | 102 (21.4) | 168 (35.2) | 99 (20.8) | 72 (15.1) | 36 (7.5) |
Table 2: Frequency distribution of the participants’ answers for OCI-R scale.
The Past Family history of OCD, past psychiatric history and counseling therapy were reported from 206 Probable-OCD students. Of which we have found that both males and females were reported, however female students tend to reported more. In which 22(64.8%) were females and 12(35.2%) were males reported past psychiatric history, with regard to family history 12(40%) were males and 18(60%) were females .With respect to counseling therapy 5(22.8%) were males and 17(77.2%) were females. The detail of family history of OCD, past psychiatric history and counseling therapy are described in Figure 2.
Psychological spectrum disorders among the study participants were analyzed in the study and most of them had answered “extremely or a lot of” for the question “as represented in Table 3 in which students reported insecure about their appearances was about 25.47% followed by 22.38% for the question “I often feel upset and could not do my daily chores.
| No | Questions | Not at all(%) | A little(%) | Moderately(%) | A lot(%) | Extremely(%) |
|---|---|---|---|---|---|---|
| 1 | I feel like I have the symptoms of an illness when I study the relevant topic | 161 (33.75) | 122 (25.57) | 108 (22.64) | 59 (12.37) | 27 (5.67) |
| 2 | I spend a lot of time feeling insecure about my appearance | 173 (36.27) | 101 (21.28) | 81 (16.98) | 60 (12.57) | 62 (12.9) |
| 3 | I pluck my hair(scalp, eyebrow, eyelashes, etc) simply or against my will | 361 (75.68) | 50 (10.48) | 34 (7.14) | 17 (3.56) | 15 (3.14) |
| 4 | I often pick my skin that it ends up in lesions | 342 (71.71) | 64 (13.41) | 31 (6.50) | 18 (3.77) | 22 (4.61) |
| 5 | I often feel upset and could not do my daily chores | 162 (33.99) | 116 (24.34) | 92 (19.29) | 69 (14.47) | 38 (7.91) |
Table 3: Frequency distribution of other spectrum disorders among the study participants.
The frequency distribution of severity of associated spectrum disorders among the study participants based on gender are shown in Table 4, of which males reported 38(37.5%) body dysmorphia and females reported 84(39.4%). Male students reported 30(29.4%) Hypochondriac whereas females reported 56(26.3%).With respect to depressive symptoms males reported 34(33.1%) whereas females reported 73(34.3%) which need for further assessment for a definite diagnosis.
| Associated spectrum disorders | Male | Female |
|---|---|---|
| N=102 (%) | N=213 (%) | |
| Hypochondriac | 30 (29.4%) | 56 (26.3%) |
| Body dysmorphia | 38 (37.5%) | 84 (39.4%) |
| Depressive | 34(33.1%) | 73 (34.3%) |
Table 4: Frequency distribution of severity of symptoms suggestive of OCD associated spectrum disorders among the study population based on gender.
Using the Chi-square test, on assessing the factors associated with OCD, a significant association was noted between age, gender, year of study and occupation of head of the family. There were significant differences with age and probable OCD (p<0.001).More than half of the students from 104(50.4%) of the probable OCD group were from the second year students. In the current study female students had reported significant association and probable OCD (p<0.005) and also female students had reported more depressive symptoms of 73 (34.3%). There were a significant differences with Probable OCD and Non-health professionals (p<0.006) as presented in Table 5.
| Variable | Probable-OCD students | Probable Non-OCD | Chi-square value | p-value |
|---|---|---|---|---|
| N=206 (%) | N=271 (%) | |||
| Age of the study participants | ||||
| ≤ 20 years | 53 (25.7%) | 163 (60.1%) | 55.9583 | 0.001* |
| >21 years | 153 (74.3%) | 108 (39.9%) | ||
| Gender | ||||
| Males | 94 (19.7%) | 89 (18.6%) | 8.09 | 0.005* |
| Females | 112 (23.6%) | 182 (38.1%) | ||
| Year of study | ||||
| First year | 57 (27.7%) | 107 (39.5%) | 38.6495 | 0.001* |
| Second year | 104 (50.4%) | 63 (23.2%) | ||
| Third year | 45 (21.9%) | 101 (37.3%) | ||
| Occupation of the head of the family | ||||
| Non-health professional | 119 (57.7%) | 189 (69.7%) | 7.33 | 0.006* |
| Health professional | 87 (42.3%) | 82 (30.3%) | ||
| Family type | ||||
| Nuclear family | 159 (77.2%) | 194 (71.6%) | 1.9 | 0.16 |
| Joint family | 47 (22.8%) | 77 (28.4%) |
Note: P value <0.05* statistically significant
Table 5: Frequency distribution and association of probably normal and OCD among different socio-demographic features.
Discussion
This is one of the handfuls of studies in India that deals with prevalence of obsessive-compulsive and spectrum disorders. According to our study 206(43%) of the participants reported probable OCD, which corresponds to a similar study done in Iraq by Taher et al. where the prevalence of OCD among undergraduate students was also reported (43%), probably this could be due to depression, bipolar disorder, stress, anxiety and COVID-19 outbreak [1]. In contrast to study conducted in Brazil by Torres et al. found (3.8%) of Brazilian medical students had a possible case of OCD based on the Obsessive- Compulsive Inventory–Revised self-administered questionnaire [9] and the OCD was associated with freshman, surrounding environmental adaptation and as well as difficulty in making friends. In our study 112(23.6%) female students have reported probable OCD, whereas study done in Iraq by Taher et al.[1] reported 67%, which was comparatively higher to our study results, these findings, along with ours, suggest that constant worry, stress, anxiety may lead to probable OCD, similar study conducted in Pakistan by Khadija et al. reported female medical students, who were in preclinical year suffered from psychological impact of COVID-19 and which may escalated the fear of contamination [10].In contrast to the study conducted in India by Jaisoorya et al. reported no gender differences [3]. On the other hand, study conducted in India by AditiArora et al. reported higher prevalence of OCD among the male students and the probable cause reported was male students fear more as compared to female students [11].In our study we have found that 57(27.7%) of first year and 104 (50.4%) of the students from second year reported higher side of prevalence,whereas study conducted in Iraq by Taher et al [1] and in Brazil by Torres et al.[9] had reported OCD among freshman students. Despite other studies having higher prevalence of washing[1,3,10], we found OCD associated spectrum disorders were high. Our study revealed 84(39.4%) of the female students were increasingly worried about their appearance, which have higher prevalence compared to western studies conducted by Biby et al. who, had reported 13% probable reason would be lower levels of selfesteem which lead to higher levels of obsessive-compulsive tendencies, depressive tendencies and somatization tendencies [12]. Our study observed 30(29.4%)of males and 56(26.3%) of females reported symptoms suggestive of hypochondriasis which was higher to study conducted in Saudi Arabia by Yusuf et al. where the reported prevalence in Males were 4(2.9%) Females 6(3.8%) which probably tells that panic disorders will have similar symptoms, such are fear and worry hypochondriacs. In our study we found symptoms related to trichotillomania 32(6.7%) and excoriation 40(8.38%),whereas study conducted in Brazil by Torresan et al. reported the rates of trichotillomania among individuals with OCD have ranged from 4.9% to 6.9% which could be due to compulsions in OCD often driven by cognitive intrusions[13,14].
This is one of the handfuls of studies in India that deals with prevalence of obsessive-compulsive and spectrum disorders. According to our study 206(43%) of the participants reported probable OCD, which corresponds to a similar study done in Iraq by Taher et al. where the prevalence of OCD among undergraduate students was also reported (43%)[1], probably this could be due to depression, bipolar disorder, stress, anxiety and COVID-19 outbreak. In contrast to study conducted in Brazil by Torres et al. found (3.8%) of Brazilian medical students had a possible case of OCD based on the Obsessive-Compulsive Inventory–Revised self-administered questionnaire[9] and the OCD was associated with freshman, surrounding environmental adaptation and as well as difficulty in making friends. In our study 112(23.6%) female students have reported probable OCD, whereas study done in Iraq by Taher et al.[1] reported 67%, which was comparatively higher to our study results, these findings, along with ours, suggest that constant worry, stress, anxiety may lead to probable OCD, similar study conducted in Pakistan by Khadija et al. reported female medical students, who were in preclinical year suffered from psychological impact of COVID-19 and which may escalated the fear of contamination [10].In contrast to the study conducted in India by Jaisoorya et al. reported no gender differences [3].On the other hand, study conducted in India by AditiArora et al. reported higher prevalence of OCD among the male students and the probable cause reported was male students fear more as compared to female students [11].In our study we have found that 57(27.7%) of first year and 104 (50.4%) of the students from second year reported higher side of prevalence,whereas study conducted in Iraq by Taher et al. [1] and in Brazil by Torres et al. [9] had reported OCD among freshman students. Despite other studies having higher prevalence of washing [1,3,10], we found OCD associated spectrum disorders were high. Our study revealed 84(39.4%) of the female students were increasingly worried about their appearance, which have higher prevalence compared to western studies conducted by Biby et al. who, had reported13% [12] probable reason would be lower levels of self-esteem which lead to higher levels of obsessive-compulsive tendencies, depressive tendencies and somatization tendencies. Our study observed 30(29.4%)of males and 56(26.3%) of females reported symptoms suggestive of hypochondriasis which was higher to study conducted in Saudi Arabia by Yusuf et al. where the reported prevalence in Males were 4(2.9%) Females 6(3.8%) which probably tells that panic disorders will have similar symptoms, such are fear and worry hypochondriacs. In our study we found symptoms related to trichotillomania 32(6.7%) and excoriation40(8.38%),whereas study conducted in Brazil by Torresan et al. reported the rates of trichotillomania among individuals with OCD have ranged from 4.9% to 6.9% which could be due to compulsions in OCD often driven by cognitive intrusions[13,14].
Strength
The study has exclusive psychological data considering medical students. To our knowledge this is the only study conducted in India for assessing OCD along with all its spectrum disorders. The study has contributed to awareness since the participants had the opportunity to make a self-assessment.
Limitations
The study though has a relatively large sample size, female predominance in the sample is higher, provided this being a purposive sampling. Hence this cannot be considered as a generalised result. The diagnostic tool used here is OCI-R which is a self-reporting scale and reliable personal interviews were not taken to make a confirmatory diagnosis.
Conclusion
Prevalence of Probable-OCD is higher in medical students than in the general population. Young students, females, students with parents of non-health professional background are of predominance to probable OCD. Body dysmorphic, hypochondriac and depressive symptoms are also probably prevalent. Friendly environment, promotion of extracurricular activities, habituation with handling patients, mental health awareness sessions and psychological counsellors are necessary preventive measures for the betterment of the mental well-being of individuals.
References
- Taher TMJ, Al-fadhul SAL, Abutiheen AA, Ghazi HF, Abood NS. Prevalence of Obsessive-Compulsive Disorder (OCD) among iraqi undergraduate medical students in time of COVID-19 pandemic. Middle East Curr Psychiatry. 2021;28:8.
[Crossref], [Google Scholar]
- Niraj Ahuja. A short textbook of Psychiatry. Seventh edition. New Delhi: Jaypee Brothers Medical Publishers (P) LTD. 2011.
- Jaisoorya TS, Janardhan Reddy YC, Nair BS, Rani A, Menon PG, et al. Prevalence and correlates of obsessive-compulsive disorder and subthreshold obsessive-compulsive disorder among college students in Kerala, India. Indian J Psychiatry. 2017;59:56-62.
[Crossref], [Google Scholar], [PubMed]
- Fineberg NA, Hollander E, Pallanti S, Walitza S, Grünblatt E, et al. Clinical advances in obsessive-compulsive disorder: a position statement by the International College of Obsessive-Compulsive Spectrum Disorders. IntClinPsychopharmacol.2020;35:173193.
[Crossref], [Google Scholar], [PubMed]
- Brock H, Hany M. Obsessive-compulsive disorder. StatPearlsPublishing. 2022.
- Nakao T, Okada K, Kanba S. Neurobiological model of obsessive-compulsive disorder: Evidence from recent neuropsychological and neuroimaging findings. Psychiatry Clin Neurosci. 2014;68:587-605.
[Crossref], [Google Scholar], [PubMed]
- Ji G, Wei W, Yue KC, Li H, Shi LJ, et al. Effects of the COVID-19 pandemic on obsessive-compulsive symptoms amonguniversity students: prospective cohort survey study. J Med Internet Res. 2020;22:e21915.
[Crossref], [Google Scholar], [PubMed]
- Joshi G, Wilens T. Comorbidity in pediatric bipolar disorder. Child Adolesc Psychiatr Clin N Am. 2009;18: 291-319.
[Crossref], [Google Scholar]
- Torres AR, Cruz BL, Vicentini HC et al. Obsessive-compulsive symptoms in medical students: Prevalence, severity, and correlates. Acad Psychiatry. 2016;40:46–54.
[Crossref], [Google Scholar], [PubMed]
- Mazhar K, Khaliq F, Arshad D. Association of COVID 19 pandemic with new onset Obsessive-Compulsive Disorder (OCD) symptomology in the medical students – A cross sectional study. BJPsych Open. 2021;18:S270.
[Crossref], [Google Scholar]
- Arora A, Chauhan A, Dhonge SS, Pandey N, Dinesh A, et al. Prevalence of obsessive–Compulsive symptoms and the level of fear due to COVID-19 pandemic among the undergraduate medical students in a tertiary care unit in Southern India. Indian J Public Health 2022;66:76-9.
[Crossref], [Google Scholar], [PubMed]
- Biby EL.The relationship between body dysmorphic disorder and depression, self‐esteem, somatization, and obsessive–compulsive disorder. Journal of clinical psychology. 1998;54:489-99.
[Crossref], [Google Scholar], [PubMed]
- Al-Turki YA, Sagga AT, Alhamidi HA, AlShammari SI, Alteraiqi BA, et al. Prevalence of hypochondriasis among medical students at King Saud University. The European Journal of Social &Behavioural Sciences. 2013.
[Crossref], [Google Scholar]
- Torresan RC, Ramos-Cerqueira AT, Shavitt RG, do Rosário MC, de Mathis MA, et al. Symptom dimensions, clinical course and comorbidity in men and women with obsessive-compulsive disorder. Psychiatry research. 2013;209:186-95.
[Crossref], [Google Scholar], [PubMed]

 ) Probable OCD, (
) Probable OCD, ( ) Probable non OCD
) Probable non OCD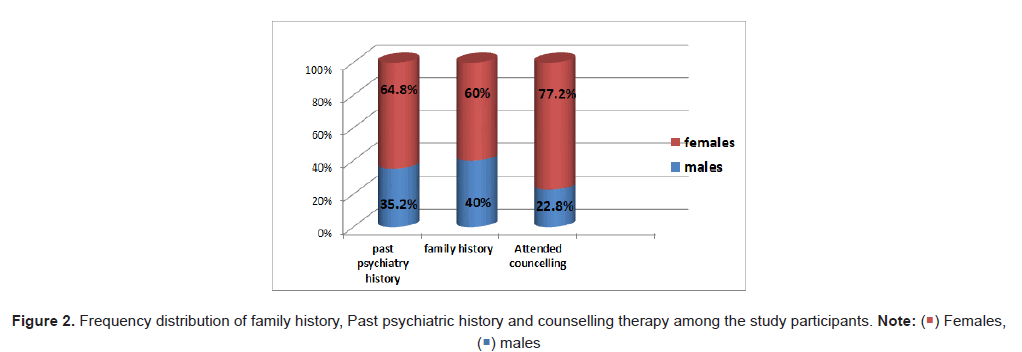
 ) Females,
(
) Females,
( ) males
) males


 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.