Oral Health Care in Patients with Spinal Cord Injury A Systematic Review
2 Vice Rector Riyadh Elm University, for Post Graduate & Scientific Research, Riyadh, Saudi Arabia
Citation: Alfaqeeh AA, et al. Oral Health Care in Patients with Spinal Cord Injury: A Systematic Review. Ann Med Health Sci Res. 2020;10:1122-1128
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: The increase in the number of vehicle accidents and falls has contributed to many spinal cord injuries (SCIs). One of the personal hygiene functions is oral care with common activities including brushing, flossing, mouth washing, and dental cleaning. However, little research has been done on the oral care that they need during their treatment and rehabilitation processes. This study assesses the oral health care for patients with SCI with a view to identifying possible remedies for improving their health. Materials and Methods: A search for articles on the topic published between 2005 and 2020 was done on PubMed, Medline, Google Scholar, and Cochrane. The Cochrane Risk of Bias Assessment tool was then used to establish the extent to which the articles could be biased to their authors’ ideas. Results: The search yielded 27 articles, but only seven (7) were included based on the set criteria. The included articles addressed oral behaviors and problems among individuals with SCI, their need for dental care and dental health status, the reasons why they have oral health problems, health-related quality of life (QoL), and the attitudes and practices of their caregivers. The common dental health problems included gingival bleeding, plaques, dental caries, and periodontal conditions. The authors agreed that the individuals had fair or compromised dental health status that required interventions. Conclusion: The training of professional providers should focus on providing dental care for SCI patients because of their special needs.
Keywords
Education; Oral health; Spinal cord injury; Training
Introduction
Many people around the world suffer from back pains and injuries resulting from falls and other types of accidents. Such occurrences contribute to the risk of developing debilitating injuries, chief of which are spinal cord injuries (SCIs). [1] During the years when people have SCIs, the injury disrupts the common life activities that individuals are able to perform. This disruption results from the individuals’ inability to use their limbs or torso because, as Kang et al. [2] explained, the condition leads to paralysis. The loss of limb and torso functions renders most of the affected individuals unable to independently eat, bathe, dress, or maintain continence, transfer, and toileting. The interference is expected to be on the rise since the number of individuals who are suffering from SCIs is likely to increase in the near and far future. This increment is based on the fact that there is a burgeoning growth in population, increased aging, and the rising use of transportation systems that are prone to accidents.
There is little or no information about patients with SCI and their oral health status. Oral hygiene differs between people in the entire population and is not limited to patients with certain disabilities. For example, men tend to neglect their oral health when compared to women, and people with low socioeconomic status have a lower tendency to visit the dental clinic regularly. Others engage in activities that increase the risk of developing dental health issues, such as smoking. [3] A report by Sullivan [4] indicated that individuals who live with SCIs are uninformed of their dental problems. It is, therefore, understandable that they do not frequent dental clinics. [5] The patients with spinal cord injury have certain limitations in receiving dental care but certainly will benefit from all types of dental treatment. [6] The focus of the present study, therefore, is on the dental hygiene, which is one of the basic ADLs, among individuals who have sustained SCIs.
Most of the efforts in caring for individuals who have endured SCIs revolve around their survival and the preservation of neurological function. [7] Consequently, they are first admitted to prehospital management units, trauma, and SCI centers. Maharaj et al. [8] explain that all these facilities seek to stabilize the patient after they encounter their injuries, with the facility where they spend most of their time receiving focused care being the SCI centers or units.
The service providers at these specialized facilities also need to be competent in giving oral and dental health care to their patients, along with the care trained to functional recovery. According to Adyanthaya et al. however, many trained dentists are not competent enough to handle the care given to individuals having SCIs and arising dental health issues, especially in the cases where the patients are infants. [9] There is also a lack of dentists specializing in caring for the needs of SCI patients in many countries. [10] There is, as such, a need to understand the needs in this population to recommend the specialization of oral health caregivers and dentists specific to individuals with SCIs. This study, therefore, assesses the status of oral health among patients with SCI to understand the extent to which specialized care is a necessity in meeting their oral health needs.
Literature Search
Study design
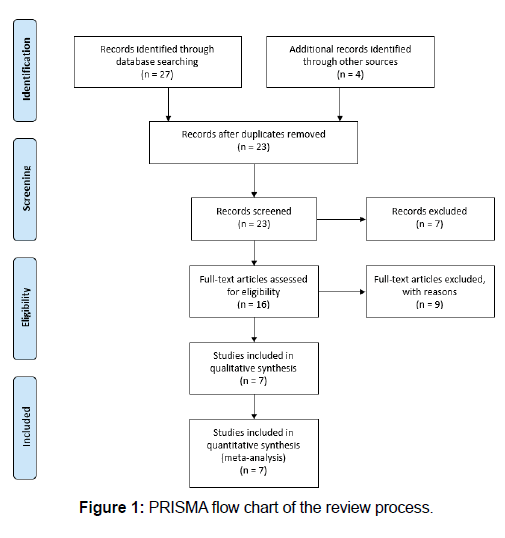
This research adopted the systematic review approach in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [Figure 1]. The method included the performance of a search for relevant articles and studies on the topic from online databases, including PubMed, Medline, Google Scholar, and Cochrane. The studies were filtered based on the year of publication, with only those published between the years 2005 and 2020 being relevant for the systematic review. The keywords used in the research process included oral health, oral hygiene, dental status, spinal cord injury (SCI), spinal injury levels, and prosthetic needs. These keywords corresponded with the research topic, which assessed the oral health status of patients who have suffered from SCIs. Articles were evaluated based on the specified criteria that they met, with the data extracted from their results section to inform the analysis.
Research topics
Specifically, the research narrowed down on patients having different levels of spinal cord injury, with the levels having an impact on the degree to which such patients can accomplish activities of daily living. The research also assessed oral hygiene and oral health status among the spinal cord injury patients, with the focus being on their status of oral hygiene, dentition, and periodontal characteristics, as well as their needs for prosthetics, depending on the level of SCI. The following are the criteria used to determine the articles that inform the systematic review.
Bias assessment
The included articles were analyzed for bias using the Cochrane Risk of Bias Assessment Tool. The tool presents five major domains for assessing bias, namely selection, reporting, performance, detection, and attrition biases. The tool was used to evaluate the risks of bias and to assign scores to each article based on the author’s evaluation of the sources. The risks were assigned numerical values for high (3), low (2), or unclear (1).
Results
The search from the online databases using the keywords yielded a total of 27 sources, while normal Internet searches yielded four additional articles. From the preliminary screening, only 23 articles were worth reviewing, while only 16 were eligible for reviews. An application of the inclusion criteria revealed that only seven met all the criteria and could form part of the systematic review.
The Cochrane Risk of Bias tool’s five domains is useful in the assessment of the bias that the authors of the included articles presented. The selection bias entails the authors’ approach to random allocations to the groups for intervention and controls. The reporting bias domain assesses the extent to which the authors had predetermined outcomes for documentation. The performance bias domain examines how the study participants were blinded from knowing the intervention to which they would be exposed. The detection bias refers to the extent to which the researchers concealed outcome assessors from knowing the interventions that participants received. The attrition bias domain, then, explains how participants were excluded from analysis for various reasons. Table 1 presents the findings from the risk of bias assessments for the included articles.
Table 1: Risk of bias assessment. Scale: high (3), low (2), and unclear (1).
| Article | Selection bias | Reporting bias | Performance bias | Detection bias | Attrition bias |
|---|---|---|---|---|---|
| Adyanthaya et al. [9] | 2 | 2 | 3 | 1 | 1 |
| Karthikayan et al. [10] | 2 | 2 | 1 | 2 | 2 |
| Khattar, D. V. [6] | 2 | 3 | 1 | 1 | 2 |
| Pakpour et al. [27] | 2 | 2 | 2 | 3 | 2 |
| Sullivan et al. [4] | 2 | 2 | 3 | 2 | 2 |
| Yuen et al. [18] | 2 | 3 | 2 | 2 | 2 |
| Yuen et al. [16] | 2 | 2 | 2 | 2 | 2 |
The included articles addressed various aspects of the oral and dental health of people having SCI. Yuen et al. explored and presented the oral behaviors and oral problems that SCI patient’s endured. [11-16] From their survey, they found that most of the individuals (87.5%) brushed their teeth each day while 45.4% used mouthwash. 59.9% of the surveyed respondents had dry mouth symptoms while 65.5% of them visited the dentists within the previous year, and 54.6% had their teeth cleaned. Sullivan et al. investigated 92 individuals with SCI by performing oral examinations and interviewing them. [17-22] They noted that 82% of the individuals had the ability to use at least one hand to reach their mouths, whereas 65% of them could brush their teeth without assistance. Among all the patients surveyed, 48% rinsed their teeth on a daily basis, 14% of them flossed, and only 32% of them successfully had their teeth professionally cleaned within the past year. These research reports point to the idea that there are individuals with SCI who do not have a particularly stellar oral health status.
The occurrence of dental health problems among individuals with SCI also affects their QoL. Pakpour et al. explored the overall QoL indicators pertinent to the oral health of SCI patients within the context of Iran. [23-27] From the findings, the authors discovered that the SCI patients in the country generally had a lower oral QoL as compared to other patients who do not have spinal injuries. The article also addressed the specific dental conditions that SCI patients popularly demonstrated, with the analysis of covariance between the SCI patients and their healthy counterparts revealing a higher prevalence of gingival bleeding, elevated levels of plaques, and more dental caries as compared to the general population. [27]
These findings do not present a grim picture of the oral behaviors, but many of the patients explained that they could not access dental services because of high costs, dental fears, or physical barriers. At the time of the survey, Yuen et al. noted that 46.9% of the respondents had oral health problems that needed professional care. [18] Khattar, after conducting a needs assessment of 58 spinal injury patients, discovered that 88% of the patients were in need of periodontal care, whereas 81% of them needed general dental care. The reasons behind these oral health problems included the loss of muscle function (paraplegia), inadequate finances and low income, dry mouth and smoking complaints, inadequate knowledge of tooth brushing techniques, the lack of professional dental cleaning services, and dental fear. Sullivan et al. also explained that the common risk factors for dental and oral health challenges among SCI patients include risky oral habits and employment prior to the occurrence of the injury. [22]
Other studies explored the reasons behind the generally low dental health status among SCI patients. Yuen et al. explored access to dental services when investigating the effects of SCI on the oral health of affected individuals. Their oral health survey findings uncovered the fact that the individuals with SCIs have a lower likelihood of visiting dentists to obtain dental cleaning services as compared to other persons. A multivariate analysis of the reasons behind this low prevalence of dental clinic visits revealed that the individuals with SCI reported the physical barriers to access dental clinics and feared the visits themselves. Yuen et al. also reported that the cost of dental care could be a contributing factor behind the limited access to dental services among individuals with SCI. [18]
The staff members’ actions and attitudes also affect the oral health of SCI patients. Khattar, after surveying both staff members and patients with SCIs at the Indian Spinal Injuries Center, noted that many staff members did not appreciate the role they have to play in caring for SCI patients, with only 70.9% of all surveyed caregivers revealing that they had a role to play in providing oral healthcare. Furthermore, among the staff members who affirmed that they were responsible for the oral care given to SCI patients, only 60% indicated that this role was very important. A staggering 29.1% of staff members were completely uninvolved in cleaning the patients’ teeth and dentures. The barriers that the staff members who were involved in providing oral care services noted included the patients’ gagging, feeling sick, or uncooperativeness by refusing to open their mouths. One staff member reported the lack of adequate time to provide oral care. The promising information from a study was that the majority of staff members were willing to be educated on oral health issues. Table 2 summarizes the findings from the articles that met the inclusion criteria.
Table 2: Summary of article findings by themes.
| Theme | Sources | Summary of Findings |
|---|---|---|
| Oral behaviors and problems | Yuen et al.[18] Sullivan et al. [22] | 87.5% of SCI patients brushed their teeth. 45.4% used mouthwash, 65.5% visited dentists. 54.6% had tooth cleaning services. 82% could use one hand, 65% could brush their teeth. 48% of patients rinsed their teeth, and 14% flossed daily. |
| Need for dental care | Khattar [6] Pakpour et al. [27] Yuen et al. [18] | 46.9% needed professional dental care. 88% needed periodontal care, and 81% required general oral care. The common dental health problems are gingival bleeding, plaques, and dental caries. |
| Reasons for oral health problems | Khattar [6] Sullivan et al. [22] Yuen et al. [18] | Inadequate finances, paraplegia, smoking, poor toothbrushing techniques or knowledge, dental fear, insufficient dental services. Risk factors for oral health issues include prior employment and smoking. The low likelihood of visiting dentists is due to barriers and dental fears. |
| SCI patients’ dental health status | Karthikayan et al. [10] Khattar [6] Pakpour et al. [27] | Fair, compromised, and worse than the general public. |
| Quality of life | Pakpour et al. [27] | SCI patients have a lower QoL than others. |
| Caregiver/staff members actions and attitudes | Khattar [6] | 70.9% of staff claim responsibility for oral care. 29.1% are uninvolved in caring for SCI patients’ oral needs. |
Discussion
The individuals with SCI generally have poorer oral hygiene as compared with the rest of the population. Some of these issues could be related to their oral health behaviors. The study by Yuen et al. revealed that not all individuals with spinal injuries brush their teeth daily –12.5% of the respondents who did not brush their teeth is a significant number. [18] The same study revealed that a good number of people in this population do not visit dentists or get their teeth professionally cleaned, with less than 50% of the population visiting dental facilities. Furthermore, the majority of people who have had spinal injuries do not receive professional education on teeth brushing and flossing. Yuen et al. study confirmed that less than 40% of the respondents reported receiving meaningful professional instruction on how to brush and floss their teeth. This lack of education could be a contributing factor to the dental health issues that the population encounters. According to Sullivan et al. there are individuals with SCI who participate in risky oral habits such as tobacco smoking. [18]
The common dental conditions that individuals with SCI present could affect their teeth, gums, and overall oral health. Pakpour et al. study revealed that SCI patients have more dental health issues, including plaques, bleeding from the gingiva, and dental caries as compared to individuals with no spinal injuries. [27] According to Yuen et al. the commonly occurring dental health issues among the study population are cavities, teeth needing extraction, gum-related illnesses such as bleeding, plaques, swelling, and pains, toothaches, and loose teeth that are also wobbly. Some of the patients experienced eating disruptions, sleep disruption, and missing school or work after suffering from dental health challenges. [18] According to Khattar, the majority of SCI patients have dental conditions that require treatment, even though the overall evaluation of their oral health was “fair”. Sullivan et al. on the other hand, noted that oral health among SCI patients is compromised, especially with the prominence of periodontal disease among 64% of the patients. [22] These findings demonstrate that the persons suffering from SCI have severe dental health problems that need to be solved with urgency.
From an analysis of the general dental health in this population as compared to other members of the public, most of the articles agree that the general status of dental health among persons with SCI is wanting. Karthikayan et al. defined their dental health status to be “fair” as opposed to the general public. They further explained that dental health issues diminish the overall dental wellbeing of the patients. [17] Yuen et al. explained that more than 50% of the respondents they included in their study had current oral problems or endured oral paints over the previous year. [18] Furthermore, the patients generally have poorer dental health practices with irregular patterns of brushing teeth, high frequency of smoking, and low frequencies of dental clinic visits during a year as compared to other people. [27] Some of the reasons behind the poor practices include poor motor and physical functioning as a result of spinal injuries, dental fears, and poor access to dental clinics. Yuen et al. also explained that many patients are financially constrained and cannot access dental health services. [18] In other cases, staff members note that some patients are not fully cooperative with their caregivers when they are supposed to receive dental services. For instance, that some patients gaggle or do not open their mouths when caregivers are attending to their oral health needs.
The individuals who have endured spinal injuries have challenges that prevent them from getting the attention they need to cope with their dental and oral health issues. Despite their experiences of adverse dental events that Yuen et al. reported, the patients rarely sought medication, with less than a quarter of them reporting to have received pain medication. Even fewer people with SCI visited dental clinics or consulted professional dentists, with the respondents who acknowledged visiting such facilities after experiencing dental health problems being only 18.9%. Another option for individuals having dental issues that interfere with their normal life is to visit emergency departments, yet Yuen et al. reported that only one of the participants in their study managed to visit an emergency care facility. [16]
In facilities dedicated to caring for patients with spinal injuries, the attitudes and behaviors of staff members could also be an impediment to meeting the patients’ dental health needs. The findings that Khattar made after analyzing the responses of staff members at the Indian Spinal Injuries Center reveal the occurrence of negative attitudes towards caring for the patients’ oral health. Not all staff members believe that they should play a role in taking care of the patients’ oral hygiene and, among the staff members who acknowledge this responsibility; only 60% affirmed that the role they played was very important. Therefore, it is highly likely that many staff members do not appreciate the significant responsibility they have towards meeting the oral and dental health needs of patients with spinal injury. The activities of the caregivers at the facility that also show that many professional caregivers are not actively involved in the procedures, with only 70% of them being active in activities such as oral cleaning and dentures. Another barrier preventing staff members’ involvement in such care is the inadequacy of time, with some noting that they do not have enough time from their busy schedules to care for the patients’ dental needs.
One of the methods of improving the oral and dental health of patients suffering from SCI is training. According to Karthikayan et al. SCI patients are physically compromised and require caregivers to help tend to their dental needs. [10] Therefore, they are highly dependent on caregivers both at home and in hospitals. Sullivan et al. confirmed this dependence by revealing that many SCI patients are able to use at least one hand to reach their mouths, but there are still several others that are tetraplegic and unable to use any of their limbs. [22] This latter category of individuals with SCIs has complete dependence on their caregivers for the provision of oral health services. The first aspect of training should focus on equipping the caregivers in domestic settings with the appropriate skills to care for the oral hygiene of the people having SCIs to prevent the occurrence of the oral hygiene challenges that Pakpour et al. explained. [27]
The second aspect of training should target the professional caregivers to give them the knowledge and skills that they need to take care of the needs of individuals with SCI in their facilities. According to Adyanthaya et al. the caregivers should receive training on how to evaluate the oral conditions of SCI patients of all ages, including children and should have the confidence to provide the appropriate care to these patients. [9] Staff members should receive training so that they can be able to assist the patients who cannot perform some actions independently, with Sullivan et al. reporting that 35% of patients are unable to brush their teeth by themselves. [22] The idea of staff training and education received support, are interested in further education on oral health issues in caring for the oral health of their patients [6] [Table 3].
Table 3: Summary.
| Title | Author | Year | Purpose | Methodology | Results and Analysis |
|---|---|---|---|---|---|
| Barriers to dental care for children with special needs: General dentists' perception in Kerala, India. | Adyanthaya, A., Sreelakshmi, N., Ismail, S., & Raheema, M. | 2017 | To identify the perceived barriers to provide oral health care for children with special needs among dental health professionals. | 149 dental professionals were interviewed through a questionnaire. | Many professionals lacked training in caring for SCI cases, and some lacked motivation. The authors recommend the training of dental professionals at the undergraduate level. |
| Spinal cord injury and oral health status: A systematic review. | Karthikayan, R., Sukumaran, A., Iyer, K., & Diwakar, M. K. | 2018 | To assess the oral health status in patients with various levels of spinal cord injury. | A systematic review of five articles published between 2007 and 2017. | SCI patients had fair and compromised oral hygiene. The reasons included poor practices, high plaque levels, gingival bleeding, and dental caries. Patients should receive oral hygiene instructions, and caregivers should also obtain training. |
| Oral health needs assessment of adults with spinal cord injuries resident in an institution. | Khattar, D.V. | 2009 | To ascertain staff members’ level of dental awareness, attitudes to oral health, and their role in the care. To assess patients’ oral health needs. |
The authors performed a clinical examination of patients and administered questionnaires to health care staff. 58 adult patients were examined, and 79 staff members responded. | Patients had a fair level of oral health, while 88% of them needed periodontal care. 70.9% of staff claim responsibility for oral care, while 29.1% of them are uninvolved in caring for SCI patients’ oral needs. |
| Oral health-related quality of life in Iranian patients with spinal cord injury: A case-control study. | Pakpour, A., Kumar, S., Scheerman, J., Lin, C., Fridlund, B., & Jansson, H. | 2016 | To compare the oral health variables, general, and oral health-related quality of life (QoL), depression, and anxiety between spinal cord injury (SCI) patients and healthy controls. | A case-control study involving 203 SCI patients and 203 healthy controls for QoL assessments. | SCI patients have poorer oral health practices, gingival bleeding, plaques, and dental caries as compared to the control group. |
| Predictors of oral health after spinal cord injury. | Sullivan, A., Bailey, J., & Stokic, D. | 2013 | To examine predictors of oral health in people with SCI. | Oral examination of 92 people and completion of questionnaires. | 82% of SCI patients could bring one hand to the mouth, 65% could independently brush their teeth, and 32% had their teeth cleaned. Periodontal disease is prominent, with only 3.3% having tooth decay. Oral health is compromised among SCI patients. |
| Factors associated with oral problems among adults with spinal cord injury. | Yuen, H. K., Shotwell, M. S., Magruder, K. M., Slate, E. H., & Salinas, C. F. | 2009 | To explore factors associated with self-reported current oral (tooth and gum) problems and oral pain in the past 12 months among adults with spinal cord injury. | The authors performed an oral health survey online and had 192 respondents from the US. | 47% of respondents had oral problems, and 42% had oral pain. Causative factors included dry mouth, financial barriers, smoking, and paraplegia. |
| Factors that limit access to dental care for adults with spinal cord injury. | Yuen, H., Wolf, B., Bandyopadhyay, D., Magruder, K., S. A., & Salinas, C. | 2010 | To identify barriers and other factors affecting dental care service utilization among people with SCI. | The authors conducted an oral health survey of 192 respondents and compared the results with the subjects from the 2004 Behavioral Risk Factors Surveillance System (BRFSS). | SCI patients are less likely to see a dentist than the general population. Individuals with SCI reported barriers such as dental care costs, physical barriers, and dental fear. The authors recommend the removal of physical barriers to accommodate SCI patients. |
The third aspect of training should focus on individuals with SCI. Yuen et al. found out that the persons with SCI have not had professionals showing them the proper techniques for brushing their teeth since they got their injuries. [16] Apart from the inability to care for themselves, many SCI-affected caregivers to give them the knowledge and skills that they need to take care of the needs of individuals with SCI in their facilities. According to Adyanthaya et al. the caregivers should receive training on how to evaluate the oral conditions of SCI patients of all ages, including children and should have the confidence to provide the appropriate care to these patients. [9] Staff members should receive training so that they can be able to assist the patients who cannot perform some actions independently, with Sullivan et al. reporting that 35% of patients are unable to brush their teeth by themselves. [22] The idea of staff training and education received support, are interested in further education on oral health issues in caring for the oral health of their patients [6] [Table 3].
The third aspect of training should focus on individuals with SCI. Yuen et al. found out that the persons with SCI have not had professionals showing them the proper techniques for brushing their teeth since they got their injuries. [16] Apart from the inability to care for themselves, many SCI-affected persons have little knowledge of how to properly perform some actions like flossing or rinsing their mouths, and Sullivan et al. explained that the minority of SCI patients floss their teeth. [22-27] Training and education could, therefore, greatly benefit these patients and demonstrate to them the methods for improving their oral hygiene.
Conclusion
The systematic review focused on the seven articles that met the inclusion criteria. The arising assessment of the dental and oral health among individuals with SCIs is that it is fair and compromised, but worse than that of the general population. The individuals with this condition need oral health services to alleviate their oral health, oral hygiene, dental status. However, they have poor access to dental health facilities because of physical barriers to reaching the facilities and their dental fears. In many cases, when they get to hospitals or other rehabilitation facilities, they are faced with incompetence or negative attitudes from the health care service providers. At the same time, their family caregivers might not have the competence or experience to perform oral health services. Therefore, there is a need for the education and training of family caregivers, health service providers, and the patients themselves in the management of oral health and hygiene.
Competing Interests
The authors declare that they have no competing interests.
REFERENCES
- James SL, Theadom A, Ellenbogen RG, Bannick MS, Montjoy-Venning W, Lucchesi LR, Abbasi N, Abdulkader R, Abraha HN, Adsuar JC, Afarideh M. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:56-87.
- Kang Y, Ding H, Zhou H, Wei Z, Liu L, Pan D, Feng S. Epidemiology of worldwide spinal cord injury: A literature review. J Neurorestoratol. 2018;6:1-9.
- Weaver FM, Smith B, LaVela SL, Evans CT, Ullrich P, Miskevics S, et al. Smoking behavior and delivery of evidence-based care for veterans with spinal cord injuries and disorders. J Spinal Cord Med. 2011;34:35-45.
- Sullivan AL. Perception of oral status as a barrier to oral care for people with spinal cord injuries. J Am Dent Hyg Assoc. 2012;86:111-119.
- Yuen HK, Azuero A, London S. Association between seeking oral health information online and knowledge in adults with spinal cord injury: A pilot study. J Spinal Cord Med. 2011;34:423-431.
- Khattar V. Oral health needs assessment of adults with spinal cord injuries resident in an institution. J. Indian Assoc Public Health Dent. 2009;7:30.
- Wing PC. Early acute management in adults with spinal cord injury: A clinical practice guideline for health-care providers. Who should read it?. J Spinal Cord Med. 2008;31:403-479.
- Maharaj MM, Hogan JA, Phan K, Mobbs RJ. The role of specialist units to provide focused care and complication avoidance following traumatic spinal cord injury: A systematic review. Eur Spine J. 2016;25:1813-1820.
- Adyanthaya A, Sreelakshmi N, Ismail S, Raheema M. Barriers to dental care for children with special needs: general dentists' perception in Kerala, India. J Indian Soc Pedod Prev Dent. 2017;35:216-222.
- Karthikayan R, Sukumaran A, Iyer K, Diwakar MK. Spinal cord injury and oral health status: A systematic review. Int J Community Dent. 2018;6:21.
- Chen Y, He Y, De-Vivo MJ. Demographic and Injury Trends of Traumatic Spinal Cord Injuries in the United States 1972-2014. Arch Phys Med Rehab.. 2016;97:e6-e7.
- Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, Waring W. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2014; 37:481.
- Edemekong PF, Bomgaars DL, Sukumaran S, Levy SB. Activities of daily living (ADLs). Treasure Island, FL: StatPearls. 2020
- LaVela SL, Landers K, Etingen B, Karalius VP, Miskevics S. Factors related to caregiving for individuals with spinal cord injury compared to caregiving for individuals with other neurologic conditions. J Spinal Cord Med. 2015;38:505-514.
- Eckert MJ, Martin MJ. Trauma: Spinal cord injury. Surgical Clinics of North America. 2017;97:1031-1045.
- Yuen HK, Wolf BJ, Bandyopadhyay D, Magruder KM, Selassie AW, Salinas CF. Factors that limit access to dental care for adults with spinal cord injury. Spec Care Dentist. 2010;30:151-156.
- Karthikayan R, Sukumaran A, Diwakar MP, Brinda B. Association between oral health status and oral health-related quality of life in subjects affected with spinal cord injuries: A cross-sectional study. J Spine Surg. 2018;2:1-4.
- Yuen HK, Shotwell MS, Magruder KM, Slate EH, Salinas CF. Factors associated with oral problems among adults with spinal cord injury. J Spinal Cord Med. 2009;32:408-415.
- Almosa NA. Oral health care in patients with spinal cord injuries: An update. Pak oral dent. 2018;38:463-467.
- Burdsall DL. How to successfully hire and manage a personal care assistant. Atlanta, GA: Shepherd Center. 2013.
- Eberhard B, Lauener SK, Imhof RM. Perspectives from family caregivers of persons with spinal cord injury in hospital versus rehabilitation: A pilot study. Rehabil Nurs. 2019;44:311-318.
- Sullivan A, Bailey J, Stokic D. Predictors of oral health after spinal cord injury. Spinal Cord. 2013;51:300-305.
- Bonfá K, Mestriner SF, Fumagalli IH, Mesquita LP, Bulgarelli AF. Perception of oral health in home care of caregivers of the elderly. Revista Brasileira de Geriatria e Gerontologia. 2017;20:650-659.
- Sarmento-Omena AR, Silva LB, Cota AL, Ribeiro CM. Perception and knowledge about oral health of caregivers of children with microcephaly. RGO-Revista Gaúcha de Odontologia. 2019;67.
- Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY, et al. Traumatic spinal injury: global epidemiology and worldwide volume. World Neurosurg. 2018;113:e345-e363.
- Emerich L, Parsons K, Stein A. Competent care for persons with spinal cord injury and dysfunction in acute inpatient rehabilitation. Top Spinal Cord Inj Rehabil. 2012;18:149-166.
- Pakpour AH, Kumar S, Scheerman JF, Lin CY, Fridlund B, Jansson H. Oral health-related quality of life in Iranian patients with spinal cord injury: A case–control study. Injury. 2016;47:1345-1352.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.