Oral Health Status of a Sample of Prisoners in Enugu: A Disadvantaged Population
- *Corresponding Author:
- Dr. E.A. Akaji
Department of Preventive Dentistry, University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu, Nigeria
E-mail: ezi787@yahoo.com
Citation: Akaji EA, Ashiwaju MO. Oral health status of a sample of prisoners in Enugu: A disadvantaged population. Ann Med Health Sci Res 2014;4:650-3.
Abstract
Background: The aim of this study is to determine the oral health status of a sample of prisoners at the Federal Prison in Enugu. The health status of inmates in the prison system needs to be incorporated into data and reports that summarize the state of the nation’s health; this will encourage the provision of health care to prisoners and foster development of the nation’s health. Subjects and Methods: The study involved 230 inmates of the Federal Prison in Enugu. An interviewer‑administered questionnaire was used to gather data on the demographic characteristics of the participants, social habits, methods and frequency of cleaning the mouth. Intraoral examination was carried out to determine caries and periodontal statuses employing decayed missing and filled teeth (DMFT) index and community periodontal index of treatment needs respectively. The proportions of participants with other soft and hard tissue conditions were also recorded. Frequency distribution tables with mean values were generated for categorical variables and non‑parametric test was used to relate DMFT values with frequency of cleaning the mouth. Results: Among the participants, 67.0% (154/230) had decayed teeth or tooth missing due to caries. None of the decayed teeth was restored yielding a 0.0% (0/230) index of restorative provision. Spearman correlation (rho) between ranks of DMFT and frequency of cleaning the mouth was −0.32 (95%CI=−0.43 to −0.19). 5.2% (12/230) participants had community periodontal index (CPI) score of 0 and 94.8% (218/230) had CPI of 1, 2, 3 or 4. Also, 56.1% (129/230) had extrinsic stains on their teeth and 17.3% (40/230) presented with fractured teeth. Conclusion: More than half of the participants were affected by dental caries and periodontal health was compromised in the majority of them. Measures to improve their oral health and the establishment of dental health‑care facility in the institution are strongly encouraged.
Keywords
Dental needs, Periodontal status, Prisoners
Introduction
The prison community has attracted much concern in the recent past due to rate of incarceration globally. World-wide rate of imprisonment per 100,000 ranges from 30 as obtained in India to about 750 as in the United States.[1] In Nigeria, the prison population was put at 46,000 with about 65% awaiting trial.[2] Prisoners often come from disadvantaged backgrounds, have low levels of education, poor nutrition, limited physical activity and worse health outcomes after release than the general population due to conditions before and during incarceration.[3-6] Added to this, the health status of prisoners is not routinely incorporated into data and reports that summarize the state of the nation’s health,[7] leading to lack of planned health services for them by relevant health bodies. Most oral diseases are preventable; measures for these are basically within the reach of the individual through good oral hygiene habits such as twice a day use of fluoride toothpaste [8] and regular utilization of oral health-care services.[9] However, these measures may pose extra challenges to an already stretched prison system with vulnerable population group whose oral health needs are complex coupled with poor access to dental care.[10,11]
A survey found a higher mean number of decayed teeth surfaces and a higher percentage of unmet dental needs in a sample of adult felons than was reported for the reference groups.[12] Another study of male prison inmates in Iowa reported fewer missing teeth than most of the subjects in the comparison groups. [13] Compared with dentate, non-institutionalized U.S. adults, Iowa prison inmates had 8.4 times the amount of untreated decay, but similar numbers of missing teeth.[13] In Nigeria, a good number of studies have been carried out on oral health status and dental needs among disadvantaged and vulnerable groups, but only a few focus on prison inmates. Braimoh et al.[14] reported a mean decayed missing and filled teeth (DMFT) of 1.15 for inmates in Benin City, which significantly increased with age (P = 0.038); deep periodontal pockets were found in older inmates and about 95% of participants had indications for oral hygiene instructions (OHI). In a related study by the same investigators, prevalence of traumatic dental injuries was found to be 20.7%; 30% due to fights and 24.1% from police brutality.[15] The authors are not aware of any oral health record for inmates in the south eastern part of the country. The aim of this study was to determine the oral health status of inmates of the Federal Prison in Enugu. The information will not only be for comparison purposes, but aid in treatment planning decisions for this disadvantaged population.
Subjects and Methods
The Federal Prison in Enugu had a total of 1255 inmates (1207 males and 48 females) at the time of data collection for this study (June 2010). Sample size of 286 was derived based the formula for sample size determination for population less than 10,000.[16] Ethical clearance was obtained from the Health Research Committee of University of Nigeria Teaching Hospital, Enugu and written permission from the Prison Authorities. A systematic sampling method was used to select the sample size of 286 using different sampling frames for both sexes, but only 230 of the inmates gave verbal consent to participate as they were not permitted to write. Data were gathered through an interviewer-administered questionnaire by trained research assistants from the 230 participants. Information obtained comprised of demographic details, social habits, tooth-cleaning tools and frequency of cleaning the mouth. Thereafter, a dental examination was performed on each participant outside the Prison’s Medical Center under natural light by two calibrated dentists. Dental caries (tooth decay) and periodontal statuses were assessed using the DMFT index with criteria based on World Health Organization oral health survey methods[17] and community periodontal index of treatment needs (CPITN) respectively.[18] Proportions of participants with fractured and stained teeth, soft-tissue lesions and injuries were also recorded.
For the DMFT, all the teeth in each participant’s mouth were examined; caries was recorded as present when there was obvious cavitation. All stages of caries that preceded cavitation were excluded and all questionable lesions were regarded as sound. The index of restorative provision was calculated by the ratio of the total number of filled teeth to the total DMFT. For the periodontal assessment, six selected index teeth were examined. These were 16, 11, 26, 36, 31 and 46 (Federation Dentaire Internationale tooth notation).The CPITN scores were recorded using codes 0, 1, 2, 3 and 4. The codes, their interpretations and corresponding required treatment are tabled below:
| CPITN codes | Interpretations | Required treatment |
|---|---|---|
| 0 | No disease; healthyperiodontal tissues | No treatment needed |
| 1 | Gingival bleedingafter gentle probingbut no periodontalpockets, no calculusand no overhangingrestoration | OHI needed |
| 2 | Periodontal pocketswere present, butnone was greater than3mm, supra-gingivalcalculus was alsopresent | Scaling and Polishingwith OHI needed |
| 3 | Pathological pocketsof 4 or 5mm deepwere present | Deep scaling withOHI needed |
| 4 | One or more toothin the sextant hadpocket greaterthan 6mm | Scaling and rootplaning±flap surgery |
In this study community periodontal index (CPI) score 0 was regarded as healthy periodontium while scores 1, 2, 3 and 4 constituted unhealthy periodontium. The data obtained were computed and analyzed using the Statistical Package for Social Sciences software for windows (version 15 SPSS Inc. Chicago. IL), and Graph Pad Prism for windows (version 5, San Diego California)
Results
Two hundred and thirty inmates aged 15-66 years (mean: 28.48 ( 9.5 years) participated in this study. 91.3% (210/230) of all the participants had been incarcerated for 0-5 years and 2.2% (5/230) for more than 10 years; the mean number of years of incarceration was 5 (0.8)years. 50.0% (115/230) of them had secondary school as the highest level of education attained, 9.6% (22/230) had no formal education and 1.7% (4/230) had completed tertiary education [Table 1]. Out all the participants, 37.4% (86/230) use a toothbrush and toothpaste to clean their mouth, 52.2% (120/230) use chewing stick, 2.6% (6/230) use salt, water or finger and 7.8% (18/230) use nothing at all. With respect to their social habits, 52.2% (120/230) were current smokers, 47.8% (110/230) were not; 38.7% (89/230) consume alcohol regularly, 61.3% (141/230) do not.
| Characteristic | No. (%) | Mean (SD) |
|---|---|---|
| Age (in years) | ||
| <20 | 17(7.4) | 28.5 (9.5) years |
| 20-29 | 147(63.9) | |
| 30-39 | 43(18.7) | |
| 40-49 | 7(3.0) | |
| 50 or more | 16(7.0) | |
| Gender | ||
| Male | 224(97.4) | |
| Female | 6(2.6) | |
| Marital status | ||
| Single | 58(25.2) | |
| Married | 172(74.8) | |
| Educational level | ||
| No formal education | 22(9.6) | |
| Primary education | 75(32.6) | |
| Secondary education | 115(50.0) | |
| Undergraduates | 14(6.1) | |
| BSc/BA and | 4(1.7) | |
| post-graduatesIncarceration period (years) | ||
| 0-5 | 210(91.3) | 5 (0.8) |
| 6-10 | 15(6.5) | |
| >10 | 5(2.2) | |
Table 1: Demographic characteristics of the participants
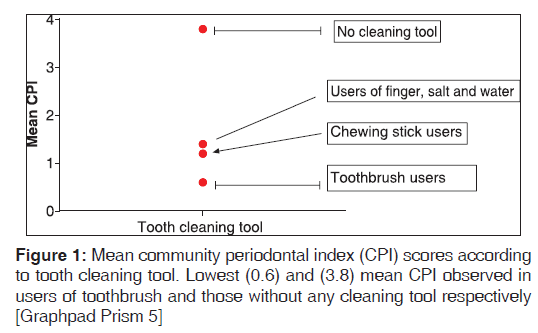
In [Table 2], 67.0% (154/230) of all participants had experienced dental caries, but no decayed tooth was restored so the index of restorative provision for the group was zero. One participant had all his teeth missing with resultant DMFT score of 32. Since the DMFT values were not normally distributed, non-parametric statistics was used to relate the DMFT values with the frequency of cleaning the mouth. Spearman correlation (rho) between the rank of DMFT values and frequency of cleaning the mouth was –0.32 within a 95% confidence interval of –0.43 to –0.19 (P < 0.001). 56.1% (129/230) of all the participants had extrinsic stained teeth, 17.3% (40/230) had at least one fractured tooth and 29.6% (68/230) had soft-tissue lesions and/or injuries. Also, 94.8% (218/230) of all the participants had unhealthy periodontal tissues and 5.2% (12/230) had healthy periodontal tissues. The mean CPI scores according to tools used to clean the mouth are shown in Figure 1; lowest (0.6 ( 0.2) was observed among toothbrush users and highest (3.8 ( 0.4) in those without a cleaning tool.
| Variables | No. | Percentage |
|---|---|---|
| Inmates affected by caries | 154 | 67.0 |
| Inmates unaffected by caries | 76 | 33.0 |
| Inmates with healthy periodontium | 12 | 5.2 |
| Inmates with unhealthy periodontium | 218 | 94.8 |
| Inmates with stained teeth | 129 | 56.1 |
| Inmates without stains on the teeth | 101 | 43.9 |
| Inmates with fractured teeth | 40 | 17.3 |
| Inmates without fractured tooth | 190 | 82.7 |
| Inmates with soft-tissue lesions/injuries | 68 | 29.6 |
| Inmates without soft-tissue lesions/injuries | 162 | 70.4 |
Table 2: Oral health profile of the participants
Discussion
We investigated the oral health status of prison inmates in the Federal Prison in Enugu. In this study, more than 90% of the study participants had unhealthy periodontal tissues, this finding is consistent with that of similar studies.[14,19] Although a good oral hygiene educational session may suffice for those with score 1, the score 2 group will require professional oral prophylaxis and those in groups 3 and 4 will require more complex treatments. Participants with extrinsic stained teeth, possibly from food debris, smoking or alcohol may also benefit from the provision of basic tools for cleaning the mouth, oral health promotion programs and professional oral prophylactic procedures to avoid a buildup of dental deposits, which may further compromise the health of the periodontal tissues.
The caries experience among participants in our study was high with more than half of them affected. While not discounting the assistance other institution dwellers may receive from their care givers, prison inmates usually operate under a restricted schedule for their day to day activities that may generally affect all their hygiene practices. We observed a reasonable inverse link between actual DMFT values and frequency of cleaning the mouth. This strengthens the view that tooth decay is a function of oral cleanliness, which in turn is a product of tooth brushing habit.[8] Although a good number of participants in the present study had missing teeth, more had untreated decayed teeth similar to findings of other studies.[14,20] We found one inmate with all his teeth missing, an observation that also featured prominently in related studies.[11,19,20] The challenges posed by total loss of all teeth in the mouth such as problems with feeding, communication and general well-being could be minimized if the missing teeth are replaced with dentures.
The index of restorative provision in the present study was 0%; non-availability of dental care facility in and from prison may have been a contributory factor. The presence of unattended fractured teeth and oral soft-tissues lesions/injuries recorded among the participants also lend credence to the absence of such facility in the institution. Availability and accessibility of oral health-care services for prisoners in other countries either partially or totally is well-documented.[11,19,20] In Australia, inmates with a low security classification usually receive treatment in local facilities under escort from custodial staff, whereas inmates with a more restrictive security classification are transported to a dental hospital through a Long Bay Prison. [11] Regular dental care services are available for inmates of Bangalore and Mysore central jails in India and for inmates of Calabria, southern Italy too.[19,20] Since dental health of inmates is known to improve when dental care facilities are available and accessible,[11,12,20] such services ought to be provided for inmates of the Federal Prison in Enugu by the relevant authorities. Another avenue that could be explored is to organize prison outreach services/postings in our Dental school so that undergraduate students and residents will have rotations in the facility as an integral part of the medical care services currently being rendered.
Conclusion
The participants’ caries experience was high and DMFT values of the participants correlated with frequency of cleaning the mouth. The periodontal health was compromised in the majority, an indication for interventions. Oral hygiene measures need to be improved amongst the participants alongside the provision of dental care facility in the institution. While our findings serve as baseline data for inmates of this prison, it is hoped that another one will be carried out on a larger scale for more detailed comparisons.
References
- King’s College London. International Centre for Prison Studies. Entire world–prison 3population rates per 100,000 of the national population. Available from: http://www. prisonstudies.org. [Last accessed on 2010 May 8].
- Rahaman O. Imperative of prison reform, 2010. Available from: http://www.focusnigeria.com/prison-reform.htm.[Last accessed on 2010 Jul 13].
- Condon L, Gill H, Harris F. A review of prison health and its implications for primary care nursing in England and Wales: The research evidence. J ClinNurs 2007;16:1201-9.
- Massoglia M. Incarceration as exposure: The prison, infectious disease, and other stress-related illnesses. J Health SocBehav 2008;49:56-71.
- Fazel S, Danesh J. Serious mental disorder in 23000 prisoners: A systematic review of 62 surveys. Lancet 2002;359:545-50.
- Farrell M, Marsden J. Acute risk of drug-related death among newly released prisoners in England and Wales. Addiction 2008;103:251-5.
- Treadwell HM, Formicola AJ. Improving the oral health of prisoners to improve overall health and well-being. Am J Public Health 2005;95:1677-8.
- Davies RM, Davies GM, Ellwood RP. Prevention. Part 4: Toothbrushing: What advice should be given to patients? Br Dent J 2003;195:135-41.
- Akaji EA, Oredugba FA, Jeboda SO. Utilization of dental services among secondary school students in Lagos-Nigeria. Niger Dent J 2007;16:87-91.
- Heath L, Iqbal Z. Measuring the health status of prisoners. PrisonServ J 2007;174:42-4.
- Osborn M, Butler T, Barnard PD. Oral health status of prison inmates — New South Wales, Australia. Aust Dent J 2003;48:34-8.
- Clare JH. Survey, comparison, and analysis of caries, periodontal pocket depth, and urgent treatment needs in a sample of adult felon admissions, 1996. J Correct Health Care 1998;5:89-101.
- Boyer EM, Nielsen-Thompson NJ, Hill TJ. A comparison of dental caries and tooth loss for Iowa prisoners with other prison populations and dentate U.S. adults. J Dent Hyg 2002;76:141-50.
- Braimoh OB, Sofola OO, Okeigbemen SA. Caries and periodontal health of prison inmates in Benin City, Nigeria.Int J Biomed Health Sci 2011;7:137-45.
- Braimoh OB, Sofola OO, Okeigbemen SA. Traumatic anterior teeth injuries among incarcerated inmates in Benin City Nigeria. Int J Biomed Health Sci 2011;7:201-7.
- Araoye MO. Research methodology with statistics for health and social sciences. 1st ed. Ilorin: Nathadex; 2003. p. 117-21.
- World Health Organization. In: Oral Health Surveys - Basic Methods. 4th ed. Geneva: WHO; 1997.
- Ainamo J, Barmes D, Beagrie G, Cutress T, Martin J,Sardo-Infirri J. Development of the World Health Organization (WHO) community periodontal index of treatment needs(CPITN). Int Dent J 1982;32:281-91.
- Nobile CG, Fortunato L, Pavia M, Angelillo IF. Oral health status of male prisoners in Italy. Int Dent J 2007;57:27-35.
- Reddy V, Kondareddy CV, Siddanna S, Manjunath M. A survey on oral health status and treatment needs of life-imprisoned inmates in central jails of Karnataka, India.Int Dent J 2012;62:27-32.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.