Pattern of Sleep Disorders among Patients in a Nigerian Family Practice Population
Citation: Olanisun Adewole. Pattern of Sleep Disorders among Patients in a Nigerian Family Practice Population. Ann Med Health Sci Res. 2017; 7: 23-31
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Sleep is required for optimal functioning; however data on sleep disorders are scarce in Family medicine practice in Nigeria. Objectives: The study determines the pattern of sleep disorder among patients attending the Family Practice Clinic at Obafemi Awolowo University Teaching Hospital Ile-Ife, (OAUTHC) Nigeria. Socio-demographic and clinical correlates associated with sleep disorder were identified. Methodology: Four hundred and ten patients attending the Family Practice clinic were selected by a systematic random sampling method were studied. Relevant data were collected using a pre-tested intervieweradministered questionnaire which included items from the Pittsburgh sleep quality index and Epworth Sleepiness scale. Results: Of the subjects were recruited, 284 (69.3%) were females. The overall mean age was 48.5+ 16.5 years with individuals aged 45-64 years and above constituting the majority (38.2%). Hypertension was the commonest medical condition seen in 147 (35.8%) subjects. Two hundred and eighty two (69%) subjects had sleep disorders. Dysomnias was the commonest sleep disorder, seen in 230 (56.1%) subjects, of which insomnia constituted the majority (48.7%) followed by snoring (32.2%). Overall the commonest sleep problem was insomnia, with a prevalence of 27.3%. One fifth of the study population had a high risk of obstructive sleep apnoea. Multiple regression analysis showed that older age (45 years and above), been separated, living close to a religious house and chronic medical condition increased the risk of sleep disorder with OR of 2.3, 2.9, 1.9 and 2.4 respectively, p < 0.05. Conclusion: About seven out of every 10 patients presenting to the Family Medicine Clinic of OAUTHC had sleep disorders. Routine screening for sleep disorders is important for early detection and treatment.
Keywords
Sleep disorders; Nigeria; Patients; Practice
Introduction
Sleep problems continue to cause considerable burden across the globe. [1,2]. They are associated with cardiovascular disease, mental health problems, motor vehicle accidents and overall poor quality of life. [3]. Sleep deprivation also increase mortality, errors and absenteeism in work place, decrease in production and deterioration of personal and professional relationships. [4]. Lack of sleep impairs a person’s ability to focus and learn efficiently. [5]. The direct and indirect costs of sleep problems are substantial.3 In Nigeria, several studies have shown that sleep problems constitute a huge burden. [6-8]. Sleep walking was associated with violence and the experience was psychologically disturbing [6] while snoring was associated with obstructive sleep apnoea. [7]. Sleep deficit was identified as a significant cause of road traffic accident. [9]. The overall rate of medical consultation was also higher in patients with sleep disorders than in those without. [10]. Sleep hygiene is poor in most developing countries with sleep problems under diagnosed and in most cases misdiagnosed inspite of the huge individual and societal burden. [11-13]. The fact that sleep disorders are associated with several morbidities, and increased mortality, underscores the importance of sleep problems as indicators of health status. [14].
Studies have shown that General Practitioners and primary care physicians are the most frequently consulted for sleep problem. [14,15]. However information on sleep disorders is largely unavailable in Family Practice in Nigeria, despite that this is the first point of entry for most patients. In order to take care of patients holistically in Family Medicine, sleep-related issues should be frequently discussed and managed. This study was to determine the prevalence and pattern of sleep disorders among patients attending the Family Medicine clinic.
Materials and Methods
Study population and setting
This was a hospital-based cross-sectional descriptive study. The study was carried out at the Family Medicine Clinic of the Obafemi Awolowo University Teaching Hospitals’ Complex (OAUTHC), Ile Ife. The OAUTHC is a tertiary hospital with five hospital units and its headquarters in Ile Ife. The other hospital units are Wesley Guild Hospital, Ilesa, Comprehensive Health Centers at Ile -Ife and Imesi-Ile and multipurpose hospital, Ilesa. The total bed capacity of the hospital is about 800. The hospital serves residents of most of Southwest Nigeria especially Osun, Ondo, Ekiti and Oyo states. Patients from Lagos, Ogun, Edo and Kogi States also patronize it. The hospital has specialist departments including Family Medicine. The Family Medicine Department in Ife hospital unit serves as a primary health facility for people aged 15 years and above. An average of 450 patients was seen in this clinic weekly. Subjects were selected from the pool of patients attending the clinic daily. The sampling frame was 5,850 while sampling interval (k=13) was obtained by dividing the sampling frame by the sample size (5,850/422). The sample size was determined using the Fisher’s formula thus. [16].
n= Z2 pq/d2
q= 1.0-p

n = minimum sample size
p = Prevalence of insomnia among elderly patients in Ibadan (51.9%).10
Z = the standard normal deviation at 95% confidence level (1.96)
d = maximum allowable margin of error which was set at 5% (5% = 0.05).
Therefore, the sample size

10% attrition was added making it 422.
In a day about 90 patients were seen, the first subject was recruited using simple random sampling technique among the first 13. Thirteen pieces of paper which had 12 “No” and only one “YES” written in them were carefully wrapped. The first 13 study participants were asked to pick one and given to the investigator who opened them to check what was picked. Each paper that was picked was subsequently returned before the next study subject picked his or her own. This gave the 13 subjects an equal chance of picking a yes. After the first subject had been picked, a systematic sampling was used to select others choosing every thirteenth patient. Hence seven subjects were recruited daily until the sample size was attained. The study was carried out from June to August 2013. Patients with altered level of consciousness and those who refused to give consent were excluded from the subjects.
Ethical considerations
Ethical clearance was obtained from the hospital’s Ethic and Research Committee. Informed written consent was obtained from each subject. Confidentiality and privacy were ensured by coding all information obtained from respondents and entering it into a personal computer.
Study instruments
Data was collected using an interviewer- administered questionnaire containing the following components:
Pittsburgh sleep quality index (PSQI): It is an international sleep questionnaire which has been validated in Nigeria and is in wide use. [17]. The PSQI is an effective instrument to assess the quality and patterns of sleep in the adult. It differentiates poor from good sleep by assessing responses to the items in the PSQI. The patient self-rated each of the items in the questionnaire, scoring on a 0-3 Likert scale, where 3 reflected the negative extreme on the Likert scale. The sum of all sub scores represented the total sleep quality score, ranging between 0-21, with higher scores representing poorer sleep quality. The individuals were categorized as follows: good sleep quality (less than five) and poor sleep quality (greater than or equal to 5).
The PSQI contains items on insomnias, snoring, nightmares, apnea and others. This is used in this study to identify sleep disorders, in addition to sleep quality. Subjects with a positive response to one or more parameter/item were taken as having the sleep disorder. [18].
Epworth Sleepiness Scale (Ess): It was used to assess excessive daytime sleepiness. The questionnaire asked the subject to rate his/her probability of falling asleep on a scale of increasing probability from 0-3 for eight different situations that most people engage in during their daily lives. The scores for the eight questions were added together to obtain a single number. A number in the range 0-9 was considered to be normal while > 9 indicated excessive sleepiness that requires medical advice. ESS has the ability to detect narcolepsy, obstructive sleep apnoea and idiopathic hypersomnia [19] and has been used previously in this environment. [20]. All questionnaires were translated into Yoruba and back translated to English by independent language experts. The Yoruba version was used for subjects who did not speak English.
Obstructive sleep apnoea: The risk of obstructive sleep apnoea was measured by asking subjects about the symptoms of snoring (S), tiredness (T) and obstruction (O) during sleeping. Each of the parameters if present was given a score of one. Their blood pressure (P), BMI (B), age (A), neck circumference (N) and their gender (G) (STOPBANG) were also recorded. A blood pressure >140/90mmHg, BMI >35 kg/m2, age >50 years, neck circumference >40 cm and male gender was also given a score of one each. A total score of three and above was considered a high risk of OSA, less than three was low risk while zero was no risk. [21].
Physical examination: This was done to measure the weight, height and neck circumference. Body mass index was calculated. Weight was measured in light clothing to the nearest 0.5 kg with the (Leaidal, United Kingdom) weighing scale. Accessories such as purses, cell phones and keys were removed before weighing. Height was measured without shoes, head gear or hat using a (Leaidal United Kingdom) stadiometer calibrated in meters and on a smooth platform to the nearest 0.01meter. Body Mass Index (BMI=weight/height2) was calculated and classified according to the WHO criteria for obesity. Underweight was a BMI of <18.4, 18.5 - <25 was normal, Overweight was a BMI of >25 kg/m2 and <30 kg/m2 while obesity was a BMI >30 kg/ m2. [22]. Blood pressure was measured after the participant had been seated for at least 10 minutes. Resting blood pressure was determined by auscultation in the right arm using a (Accoson England) mercury sphygmanometer. The cuff was applied evenly on the bare arm with the lower edge at 2.5 cm above the antecubital fossa. The onset of clear tapping sounds was taken to indicate systolic blood pressure and sound disappearance as the diastolic blood pressure (i.e., first and fifth phases of the korotkoff sounds respectively). Elevated blood pressure was taken as a blood pressure >140/90 mmHg.
Neck circumference was measured using a non-elastic measuring tape. Measurement was taken on bare skin. The patient looked straight ahead with shoulders down (not hunched). Neck circumference was measured at a point just below the larynx (Adams apple) perpendicular to the long axis of the neck to the nearest centimetre. Neck circumference greater than 40 cm was taken as a fat neck with a risk of obstructive sleep apnoea. [20].
Exhaled carbon monoxide was measured by providing subjects with a hand-held (Micro smokerlyser CO monitor) carbon monoxide analyser. The monitor was switched on, subjects were asked to inhaled deeply and held their breath, after a count of 15 seconds they exhaled into the carbon monoxide monitor through its mouth piece. The exhaled carbon monoxide was registered and recorded in parts per million (ppm). A score of < 7 was taken as normal while > 7 was high. [23].
Other aspects of the questionnaire included items on income, alcohol and smoking status. Respondents’ income was categorised into below N18,000.00 and above N18,000.00 according to National minimum wage categorization in Nigeria. [24].
Subjects were classified based on alcohol use, those who had never consumed alcohol at any time and the occasional drinkers. Subjects were simply classified as smokers and non-smokers. Nonsmokers included both ex-smokers and never smoked.
Statistical Analysis
Data was entered into a personal computer and analyzed using Statistical Package Social Science (SPSS) software for windows version 17. Socio-demographic characteristics and other descriptive data were presented using frequency tables. Numerical indices were determined as appropriate. Means and standard deviations were calculated for continuous variables while ratios and proportions were calculated for categorical variables. Associations between sleep disorder, sociodemographic and co-morbid medical conditions were explored by using Pearson’s Chi square test. Association between sleep disorder and continuous variables such as neck circumference, body mass index and carbon monoxide level were analysed using the student t-test. Level of significance was taken as <0.05. Logistic regression analysis was done to determine sociodemographic and medical variables/characteristics predicting sleep disorders.
Results
Four hundred and ten subjects were recruited of which 284 (69.3%) were females. The overall mean age was 48.5+ 16.5 years with individuals aged 45-64 years and above constituting the majority (38.2%). Three hundred and sixteen (77.1%) were Christians, while Yoruba was the dominant ethnic group, 91.2%. Majority, 124 (30.2%) had tertiary education while 256 (62.4%) earned less than N18, 000 monthly. Fifty six (13.7%) and 35 (8.5%) consumed alcohol and smoked cigarette respectively. Other socio-demographic characteristics of the subject were as shown in Table 1.
| Characteristics | Frequency | |
|---|---|---|
| n | (%) | |
| Sex | ||
| Male | 126 | (30.7) |
| Female | 284 | (69.3) |
| Age group, years | ||
| < 25 | 34 | (8.3) |
| 25 – 44 | 135 | (33.0) |
| 45 – 64 | 157 | (38.2) |
| > 65 | 84 | (20.5) |
| Religion | ||
| Christianity | 316 | (77.1) |
| Islam | 94 | (22.9) |
| Ethnicity | ||
| Yoruba | 374 | (91.2) |
| Others | 36 | (8.8) |
| Marital Status | ||
| Single | 61 | (14.9) |
| Married | 251 | (61.2) |
| Divorced/Separated | 27 | (6.6) |
| Widow | 71 | (17.3) |
| Educational Status | ||
| No formal education | 91 | (22.2) |
| Primary | 84 | (20.5) |
| Secondary | 111 | (27.1) |
| Tertiary | 124 | (30.2) |
| Employment status | ||
| Employed | 314 | (76.6) |
| Unemployed | 10 | (2.4) |
| Retired | 50 | (12.2) |
| Students | 36 | (8.8) |
| Monthly Income | ||
| ≥ N 18,000 | 256 | (62.4) |
| ≤ N 18,000 | 154 | (37.6) |
| Living close to church/mosque | ||
| Yes | 236 | (57.6) |
| No | 174 | (42.4) |
| *Shift work | ||
| Yes | 43 | (13.7) |
| No | 271 | (86.3) |
| Alcohol | 56 | (13.7) |
| Smoking | 35 | (8.5) |
| Family history of sleep disorder | 45 | (11.0) |
Table 1: Distribution of study subjects by socio-demographic factors (N=410).
Anthropometric characteristics of the subjects
Table 2 shows the anthropometric characteristics of the study subjects. A s shown, majority of the respondents have normal measurement, 92%. Similarly, majority, 191 (48.6%) had a normal BMI. While 77 (18.8%) respondents were obese, 33 (8%) were underweight.
| Characteristics | Frequency | |
|---|---|---|
| n | % | |
| Neck circumference | ||
| Normal | 377 | (92.0) |
| Fat | 33 | (8.0) |
| Total | 410 | 100 |
| BMI, kg/m2 | ||
| Underweight | 33 | (8.0) |
| Normal | 191 | (48.6) |
| Overweight | 109 | (26.6) |
| Obese | 77 | (18.8) |
| Total | 410 | 100 |
Table 2 : Anthropometric characteristics of the study subjects.
Prevalence of sleep disorders
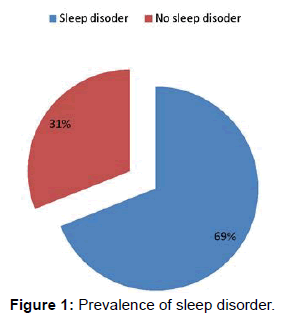
Two hundred and eighty two (69%) subjects had sleep disorders as shown in Figure 1.
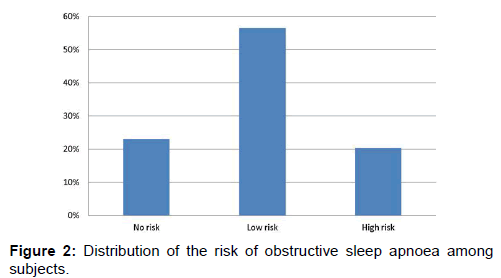
Dysomnias was the commonest sleep disorder, seen in 230 (56.1%) subjects, of which insomnia constituted the majority (48.7%) followed by snoring (32.2%). Overall the commonest sleep problem was insomnia, with a prevalence of 27.3%, as shown in Table 3. One fifth of the study population had a high risk of obstructive sleep apnoea, as shown in Figure 2.
Table 3 shows the distribution of the various types of sleep disorders among the subjects. As shown, dysomnia is the commonest type, seen in 230 (56%), while 26% had parasomnia. The commonest form of dysomnia was insomnia, responsible for 48.7% of dyssomnia cases. Some subjects (26%) had combined dysomnias and parasomnias as shown.
| Types of sleep disorders | Frequency | |
|---|---|---|
| n | % | |
| Dysomnia | ||
| Restless leg syndrome | 4 | 1.7 |
| Apnoea | 8 | 3.5 |
| Excessive sleepiness | 32 | 13.9 |
| Insomnia | 112 | 48.7 |
| Snoring | 74 | 32.2 |
| Total | 230 | 100 |
| Parasomnia | ||
| Nightmare | 17 | 65 |
| Night terror | 9 | 35 |
| Total | 26 | 100 |
| Combined Dysomnias and Parasomnia | 26 | 100 |
Table 3 : Frequency distribution of types of sleep problems among study subjects.
Association between Socio demographics and sleep disorder
Several factors including age group 45-64 years, being separated, divorced and widowed, lack of education, chronic medical condition and quantity of exhaled carbon monoxide were associated with sleep disorders, p < 0.05. There was no association between sleep disorders and sex, religion, anthropometric characteristics, income, shift work and location of accommodation; this is shown in Table 4.
| Characteristics | N | (%) | Sleep disorders | X2 | df | p - value | |||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | ||||||||
| n | (%) | n | (%) | ||||||
| Age group | |||||||||
| < 25 | 34 | (8.3) | 17 | (50.0) | 17 | (50.0) | |||
| 25 - 44 | 135 | (33.0) | 83 | (61.5) | 52 | (38.5) | 14.4 | 3 | 0.001 |
| 45 - 64 | 156 | (38.0) | 120 | (77.0) | 36 | (23.0) | |||
| >65 | 85 | (20.0) | 62 | (73.0) | 23 | (27.0) | |||
| Sex | |||||||||
| Male | 126 | (30.7) | 85 | (67.0) | 41 | ( 33.0) | |||
| Female | 284 | (69.3) | 197 | (69.0) | 87 | (31.0) | 0.4 | 1 | 0.7 |
| Religion | |||||||||
| Christian | 316 | (77.1) | 220 | (69.0) | 96 | (31.0) | |||
| Islam | 94 | (22.9) | 62 | (66.0) | 32 | (34.0) | 0.45 | 1 | 0.5 |
| Ethnicity | |||||||||
| Yoruba | 374 | (91.2) | 257 | (68.7) | 117 | (31.3) | |||
| Others | 36 | (8.8) | 25 | (69.4) | 11 | (30.6) | 0.01 | 1 | 0.9 |
| Marital status | |||||||||
| Single | 61 | (14.9) | 29 | (47.5) | 32 | (52.5) | |||
| Married | 251 | (61.2) | 170 | (67.7) | 81 | (32.3) | |||
| Divorced/separate | 27 | (6.5) | 21 | (77.8) | 6 | (22.2) | 23.8 | 3 | 0.002 |
| Widow | 71 | (17.1) | 62 | (87.3) | 9 | (12.7) | |||
| Educational status | |||||||||
| No formal | |||||||||
| education | 91 | (22.2) | 75 | (82.0) | 16 | (18.0) | |||
| Primary | 84 | (20.5) | 63 | (75.0) | 21 | (25.0) | |||
| Secondary | 111 | (27.1) | 76 | (69.0) | 35 | (31.0) | 20.6 | 3 | 0.001 |
| Tertiary | 124 | (30.2) | 68 | (54.8) | 56 | (45.2) | |||
| Employment | |||||||||
| Employed | 314 | (76.6) | 218 | (69.4) | 96 | (30.6) | |||
| Unemployed | 96 | (23.4) | 64 | (66.7) | 32 | (33.3) | 1.37 | 1 | 0.24 |
| Income | |||||||||
| ≥N 18,000 | 256 | (62.4) | 178 | (69.5) | 78 | (30.5) | |||
| ≤ N 18,000 | 154 | (37.6) | 104 | (67.5) | 50 | (32.5) | 0.18 | 1 | 0.67 |
| *Shift work | |||||||||
| Yes | 43 | (13.7) | 28 | (65.0) | 15 | (35.0) | |||
| No | 271 | (86.3) | 175 | (64.6) | 96 | (35.5) | 0.01 | 1 | 0.95 |
*Shift workers n=314
Table 4: Association between socio - demographic factors and sleep disorders.
Association between sleep disorders, anthropometric characteristics and medical condition
The mean neck circumference and BMI of subjects with and without sleep disorders were not significantly different as shown in Table 5 (p>0.05). Majority of subjects with chronic medical conditions 259 (78.7%) had sleep disorder compared with those who had acute medical conditions. This association was found to be statistically significant, (p<0.001), as shown in Table 5.
| Mean NC (SD) | Mean BMI kg/m2 | Medical conditions | ||||
|---|---|---|---|---|---|---|
| Acute | Chronic | |||||
| Sleep disorder | N | Mean | N | Mean | N (%) | N (%) |
| Yes | 282 | 35(13.5)* | 282 | 25.2(19.4)* | 23(28.3%) | 259(78.7%) ** |
| No | 128 | 34.5(13.6) | 128 | 24.2 (20.3) | 58(71.7) | 70(22.3%) |
NC: Neck circumference; BMI: Body mass index; * p value more than 0.05, ** p value less than 0.001
Table 5: Association between Sleep disorders nthropometric characteristics and medical conditions.
The median (range) carbon monoxide (CO) level of subjects with sleep disorders, 5 ppm (3-10 ppm) was significantly higher than the median (range) level for subjects without sleep disorders, 3 ppm (2-9 ppm), p-value <0.001.
Association between sleep quality and sleep disorder
As shown in Table 6, sleep quality was poor in 130 (46.0%) subjects with sleep disorder compared with 25 (19.5%) subjects without sleep disorder. This association was found to be statistically significant, (p value=0.001).
| Sleep disorder | N | % | Sleep quality | X2 | df | p value | |||
|---|---|---|---|---|---|---|---|---|---|
| Good | % | Poor | % | ||||||
| Yes | 282 | (69.0) | 152 | (54.0) | 130 | (46.0) | |||
| No | 128 | (31.0) | 103 | (80.5) | 25 | (19.5) | 26.43 | 1 | 0.001 |
| Total | 410 | 100 | |||||||
Table 6: Association between sleep disorders and sleep quality.
Multiple regressions of factors affecting sleep disorder
Table 7 shows the multiple regression results of factors affecting sleep disorders. Subjects’ characteristics which were moderately significantly associated with sleep disorder at p value <0.25 were included in the logistic regression. Marital status, education and employment status, living close to a church or mosque and level of exhaled CO were significant determinants of the occurrence of sleep disorder (p< 0.05). Individuals who were 45-64 years and 65 years and above had 2.3 and 2.4 risk of having sleep disorders respectively compared with younger age groups. Similarly divorce/separation or widowhood was associated with a significant risk of sleep disorder compared with single status, OR 2.9 and 3.3 respectively. Being unemployed and retired was associated with higher risk of sleep disorder compared with students, OR 1.9 and 2.9 respectively. Individuals with no formal education, primary education and secondary education had increased risk of sleep disorders compared with those with tertiary education, OR 2.7, 2.4 and 1.8 respectively. Having chronic medical condition was associated with an increased risk of having sleep disorder than acute medical conditions, OR 2.4.
| Parameters | P value | Odds ratio | 95%CI |
|---|---|---|---|
| Age | |||
| *< 25 | 1 | ||
| 25 – 44 | 0.9 | 1.4 | 0.6 - 1.9 |
| 45 – 64 | 0.001 | 2.3 | 1.08 -  3.3 |
| > 65 | 0.002 | 2.4 | 1.1 -  3.9 |
| Educational status | |||
| *Tertiary | 1 | ||
| No formal education | 0.01 | 2.7 | 1.5 - 5.0 |
| Primary | 0.04 | 2.4 | 1.3 - 4.5 |
| Secondary | 0.02 | 1.8 | 1.0 - 3.1 |
| Marital status | |||
| * Single | 1 | ||
| Married | 0.57 | 1.6 | 0.2 - 3.3 |
| Divorced/Separated | 0.001 | 2.9 | 1.4 - 6.9 |
| Widow | 0.001 | 3.3 | 1.6 - 8.7 |
| Employment status | |||
| * Students | 1 | ||
| Employed | 0.06 | 1.6 | 0.9 - 2.2 |
| Unemployed | 0.002 | 1.9 | 1.1 - 5.9 |
| Retired | 0.001 | 2.9 | 1.5 - 3.8 |
| Living close to Church/Mosque | |||
| *No | 1 | ||
| Yes | 0.001 | 1.8 | 1.05 - 3.0 |
| Alcohol | |||
| *No | 1 | 0.2 - 2.4 | |
| Yes | 0.06 | 1.6 | |
| Family history of sleep disorder | |||
| *No | 1 | ||
| Yes | 0.14 | 1.5 | 0.9 - 2.6 |
| Medical condition | |||
| * Acute | 1 | ||
| Chronic | 0.001 | 2.4 | 1.5 - 5.7 |
| Level of exhaled CO | |||
| * Normal | 1 | ||
| High | 0.02 | 2.9 | 1.9 - 4.8 |
| Neck circumference | |||
| *Normal | 1 | ||
| Fat | 0.3 | 0.7 | 0.2 - 1.5 |
| Body Mass Index | |||
| *Normal | 1 | ||
| Abnormal | 0.08 | 0.7 | 0.45 - 1.1 |
Table 7: Multiple regression of factors affecting sleep disorder.
A high level of CO was associated with about thrice the risk of sleep disorders, compared with the normal level of exhaled CO. Chronic medical condition had increased risk of sleep disorders compared with acute, OR 2.4. Living close to a church or mosque also had increased risk of sleep disorders compared with those who were not, OR 1.8. However alcohol intake, family history of sleep disorders and anthropometric parameters did not predict the occurrence of sleep disorder, (p > 0.05).
Discussion
This study reported a prevalence of 69% for sleep disorders, with dysomnia as the commonest form of sleep disorder. Insomnia was the commonest sleep disorder while 20% of the subjects have high risk for OSA. Age, sex, marital status and duration of medical condition were associated with sleep disorder.
The prevalence of sleep disorder in this study is comparable to 71% obtained among blacks in a Family Medicine set up in the United States [25]. but higher than 55% reported by Alattar et al. [19]. in a Family Practice setting in North Carolina some ten years before. The difference observed in these two studies may be due to the rising incidence of sleep disorder and the effect of ethnicity as patients of different races were recruited by Alattar et al. compared with this study where the population was homogenous and black. Even though the black race has a higher prevalence of sleep disorders compared with Caucasians, [25]. the prevalence of sleep disorder is rising globally.
The commonest form of sleep disorder in this study was dysomnias with a prevalence of 56.1%. This finding corroborates a previous report by Ansari et al. [26]. which showed that dysomnias were the commonest form of sleep disorder with a prevalence of 70.9%. In this study, insomnia was the commonest form of dysomnias. It accounted for 48.7% of dysomnias, (and 27.3% overall), followed by snoring, seen in 32.2%. Other forms of dysomnias were generally low in prevalence. The prevalence of insomnia obtained in this study was higher than the 18.6% reported by Panda et al. [27] in a community based study of apparently healthy populations in India but lower than findings in Ibadan where 51.9% of patients had insomnias. [28]. It is also lower than 60% reported among patients seen in a primary care setting in Malaysia. [29]. The difference could be due to instruments used. A self-administered questionnaire was used in the study in Malaysia while an interviewer administered questionnaire was used in this study. The prevalence rate obtained in this study is reflective of the demographics as the middle aged and the elderly constituted the majority. Insomnias are commoner in these segments of the population. [30]. Despite this geographic variations in the prevalence of insomnias, it has been observed that insomnia is the commonest sleep complaint in primary care settings globally. [29,31]. This observation is corroborated by the findings of this study.
About a third of the respondents reported a history of snoring. This is comparable to the 31.6% reported among adults in Abuja [7] but lower than the 50% reported in an older population in Osogbo. [32]. Age is a known predisposing factor for snoring, as the occurrence of snoring increases with age. [7].
OSAs is a medical problem with great public health impact. [33]. It is a risk factor for road traffic accidents and poor productivity. [34]. It is characterized by habitual snoring and un-refreshing night sleep with marked daytime sleepiness. [34]. In this study about 20% had a high risk of OSA. This is similar to 19% reported by Adewole et al. [35]. in Abuja but slightly higher than 17.4% reported in Sagamu in adult population of an Ear, Nose and Throat outpatient clinic. [36]. It is also higher than 14.1% reported by Akkoyunlu et al. [37]. in his study among long distance driver in Turkey. The difference observed in these studies could be due to the different instruments that were used. The Berlin sleep questionnaire was used by Sogebi et al. [36]. and its said to be more cumbersome than the STOPBANG which is easily administered. [38]. While PSG was used in the study by Akkoyunlu et al. [37]. which is the gold standard for diagnosing OSA. Questionnaires based studies commonly overestimate OSAs, 46 this might have accounted for the differences observed in these studies. Polysomnograhy which is the gold standard for diagnosis is not readily available; a simple screening tool (STOPBANG) which was employed in this study could be used to screen for high risk individuals in order to offer appropriate help in the clinic setting.
In this study parasomnias were observed only in 12.6% of respondents. Anecdoctal evidence suggests that lots of people attach spiritual importance and significance to most parasomnias and may not really see it as a sleep disorder. This may account for the low rate obtained in this study. Inspite of this, nightmare was the commonest parasomnia found in this study. This is consistent with reports by Bjorvatn et al. [39]. who reported a prevalence of 19.4% for nightmare and 2.7% for sleep terror.
We observed that 62% of the respondents had good sleep quality. This is higher than the 30.8% reported in a Family Practice setting in Ilorin [40] and 58% reported by Alebiosu et al. [41]. in Sagamu. In this study, a heterogeneous group of patients was studied unlike the studies in Ilorin and Sagamu which involved patients with depression and hypertensive disorders. In this study the prevalence of smoking or alcohol was quite low which may also explain the higher sleep quality obtained in this study. [42]. As shown in this study, individuals with sleep disorders had poor sleep quality. Better sleep quality is known to be associated with improved quality of life. More attention should be paid to educating patients on good sleep hygiene and the need to avoid stimulant use.
On multiple regression analysis, predictors of sleep disorder in this study included age, marital and educational status, employment and level of exhaled CO. Other factors found to predict sleep disorders in this study include, living close to a church or mosque and the presence of a chronic medical condition.
Age is a known risk factor for sleep disorder. In this study individuals in the age group 45-64 years were more affected followed by those who were 65 years and above with odds ratio of 2.3 and 2.4 respectively. This finding is similar to the report by Alatar [19]. in a family practice set up and is consistent with earlier reports. [43,44]. Studies comparing sleep in older adults to younger adults found that older adults spent less time in deeper stages of sleep (N3 or slow-wave sleep). A meta-analysis including approximately 65 studies representing 3,577 (age 5 to 102 years) participants suggested that with increasing age, time spent in lighter stages of sleep increased while time spent in REM and slow-wave sleep decreased. [44]. All these contribute to increase the occurrence of sleep disorders with increasing age. Considering the impact that sleep disturbance can have on health, it is important to pay special attention to sleep quality among elderly populations.
Marital status was also found to be a predictor of sleep disorder. As shown in this study, widows had increased risk of sleep disorder with an odd ratio of 3.3 followed by those who are divorced or separated with odds ratio of 2.9 compared to singles. Taken together, this may be indicative that loneliness caused by widowhood, divorce or separation may be a responsible factor. The pain of divorce or separation and grieve for the loss of a spouse is frequently associated with poor sleep, especially insomnia. This is corroborated by studies from Korea and Britain. [45,46].
Noise is one of the key environmental factors that affect sleep. [47]. Individuals living in a noisy neighbourhood are likely to have sleep disorders compared with those who are not. [48]. Where an individual lives is also influenced by socio economic status which is influenced to a large extent by the educational attainment and income. [49]. In this study, living close to a church or mosque and lower educational status were associated with increased risk of sleep disorder. Night noise from religious houses especially during night vigils generate high sound levels which decrease sleep intensity and increase arousal. Omlin et al. [50]. reported an increase in Electroencephalographic awakening in individuals living within 120m distance from churches in Zurich due to church bell noise. This is a common situation in Nigeria where religious houses are usually sited close to residential buildings. Lower educational status has a direct bearing on income, location and type of accommodation. [51]. These may explain the higher occurrence of sleep disorder among such groups as also reported by Arber et al. [46].
In this study higher level of exhaled CO was associated with poor sleep. Exhaled CO level can be used to determine smoking status. [23]. It can also be used to estimate the degree of air pollution in a given locality. [52]. After controlling for smoking status, levels of exhaled CO has a direct relationship with both indoor and outdoor air pollution. [21]. Both indoor and outdoor air pollution have been implicated as a cause of poor sleep as shown by Zhang et al. [52]. In an environment like ours where there is increased use of diesel or premium motor spirit generator to provide alternative source of energy for lightening, the exhaust from such generator is associated with indoor and outdoor pollution which may affect sleep. The medical consequences associated with both indoor and outdoor air pollution, such as chronic obstructive lung disease, can also disrupt sleep continuity and have a negative impact on sleep architecture. [53,54].
In this study, chronic disease conditions were associated with more than twice the risk of sleep disorders compared with acute medical conditions. The increased occurrence of sleep disorders in chronic disease conditions may be related to the psychological impact of the disease. [55,56]. Similarly some of the drugs used for treatment may on a long term affect sleep patterns or cause structural changes that increases predisposition to or accelerate progression of sleep disorder. [57,58].
Sleep disorder was also associated with employment status in this study, with the unemployed and the retiree having 1.9 and 2.9 risk of developing sleep disorder. Unemployment is linked to less education and more likely to live in overcrowded areas with air pollution while the retiree are more likely to be in the older age group, more likely to be separated or widowed and more likely to have chronic medical condition. All these have been linked to poor sleep as supported by Lalluka [59] and Ogbolu et al. [60].
Some limitations of this study like being a single center cohort analysis and non- availability of PSG to confirm or detect some other sleep disorder must be acknowledged. The variation of sleep disorder across different ethnic groups could also not be determined because the subjects were mainly from one Ethnic group. Further studies in the future will take note of these and should also determine the impact of sleep disorder on quality of life. However inspite of these limitations, this study have provided important data on the prevalence of sleep disorders among family practice patients.
Conclusion
In conclusion, sleep problems appear to be a big burden among Family practice patients attending OAUTHC, therefore for any intervention to be effective, family physicians must be involved at the very earliest time. Attention should also be placed on sleep hygiene and sleep education.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Ram S, Seirawan H, Kumar SKS, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep breath 2010; 14: 63-70.
- Leger D, Poursain B, Neubaer D, Uchiyama M. An International survey of sleeping problems in the general population. Current Medical Research 2008; 1: 307-317.
- Plantinga L, Rao MN, Schillinger D. Prevalence of self-reported sleep problems among people with diabetes in the United States, 2005-2008. Prev Chronic Dis 2012; 9: 110244.
- Kim JY, Kim JH, Lee HW, Choi KG. Prevalence of shift work sleep disorder and its impact on health and working. J Korean sleep Res Soc 2005; 2: 39-46.
- Gais S, Lucas B, Born J. Sleep after learning, aids memory recall. Learn mem. 2006; 13: 259-262.
- Mume CO. Prevalence of sleepwalking in an adult population. Libyan J Med 2010; 5: 2143.
- Adewole OO, Adeyemo HO, Ayeni F, Anteyi EA, Ajuwon ZO, Erhabor GE. Prevalence and correlates of snoring among adults in Nigeria. Afr Health Sci. 2008; 2: 108-113.
- Oluwole OSA. Lifestyle prevalence and incidence of parasomnias in a population of young adults Nigerians. J Neurol 2010; 257: 1141-1147.
- Aworemi JR, Abdul-Azeez IA, Oyedokun AJ, Adewoye JO. Efficacy of drivers’ fatigue on road accident in selected south-western states of Nigeria. International Business Research 2010; 3: 225-232.
- Blay SL, Andreoli SB, Gastal LG. Prevalence of self-reported sleep disturbance among older adults and the association of disturbed sleep with service demand and medical conditions. International Psychogenetics 2008; 3: 582-592.
- Bixler KO, Kales A, Soldatos CR, Kales JD, Healey S. Prevalence of sleep disorders in Los Angeles metropolitan area. Am J Psychiatry 1979; 136: 1257-1262.
- Ohayon MM. Prevalence and co morbidity of sleep disorders in general population. Rev Pract 2007; 14: 1521-1528.
- Ohayon MM, Schenck CK. Violent behaviour during sleep: Prevalence, comorbidity and consequences. Sleep Med. 2010; 9: 941-946.
- Wallander M, Johansson S, Ruigomez A, Rodiriguer G, Jones R. Morbidity associated with sleep disorders in a primary care: A Longitudinal cohort study. Primary care companion J Clin Psychiatry. 2007; 5: 338-345.
- Morin CM, Le Blanc M, Daley M., Gregoire JP, Merette C. Epidemiology of insomnia: Prevalence, self-help treatments, consultations and determinants of help seeking behaviour. Sleep Medicine 2006; 72: 123-130.
- Araoye OM. Research methodology and Statistics for health and social sciences. Ilorin. Nathadex Publishers 2003. 115-118.
- Aloba OO, Adewuya AO, Ola BA, Mapayi BM. Validity of the Pittsburgh sleep quality index (PSQI) among Nigerian University students. Sleep Med 2007; 8:266-270.
- Alattar M., Hamington JJ, Mitchell CM, Sloane, P. Sleep problems in primary care: a North Carolina family Practice Research Network (NC-FP-RN) study. J Am Board Fam 2007; 20: 365-375.
- Buysse DJ, Rynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep Quality index (PSQ1): A new instrument for psychiatric research and practice. Psychiatry Research 1989; 2:193-213.
- Adeosun SO, Asa SO, Babalola OO, Akanmu MA. Effects of night reading on daytime sleepiness sleep quality and academic performance of undergraduate pharmacy students in Nigeria. Sleep Biol Rhythms 2008; 6:91-94.
- Ankichetty S, Chung F. Considerations for patients with Obstructive sleep apnea undergoing ambulatory surgery. Curr Opin Anesthesiol 2011; 24: 605-611
- Body Mass Index. Centers for disease control and prevention. https//www.cdc.gov. (Assessed 24th April 2017).
- Laugesen M, Epton M, Frampton C, Glover M, Lea RA. Hand-rolled smoking patterns compared with factory made. Cigarette smoking in New Zealand men. BMC Public health 2009; 9: 194
- Nigeria Minimum Wage, Labour Law, and Employment Data Sheet. http://www.minimum-wage.org/international/en/Nigeria. (Assessed 24/7/2014)
- Pigeon WR, Heffner K, Duberstein P, Fiscella K, Moynihan J, Chapman BP. Elevated sleep disturbance among blacks in an Urban Family Medicine Practice. J. Am Fam Med 2011; 2: 161-168.
- Ansari AA. Descriptive study of sleep disorders in Psychiatry patients - A cross sectional study online http: // hdl.handle.net/123456789/1708. (Accessed 30/5/14).
- Panda S, Taly AB, Sinha S, Gururaj G, Girish N, Nagaraja D. Sleep-related disorders among a healthy population in South India. Neurol India 2012; 60: 68-74.
- Lasisi AO, Gureje O. Prevalence of insomnia and impact on quality of life among community elderly with tinnitus. Ann Otol Rhinol Laryngol. 2011; 4: 226-230.
- Zailinawati A, Mazza D, Teng CL. Prevalence of insomnia and its impact on daily functioning amongst Malaysian primary care patients. Asia Pacific Family Medicine 2012; 11: 9.
- Aikens JE, Rouse ME. Help-seeking for insomnia among adult patients in primary care. J Am Board Fam Pract 2005; 4: 257-260.
- Terzano MG, Parrino L, Cirignotta F, Ferini-Strambi L, Gigli G, Rudelli G. Studio Morfeo: Insomnia in primary care, a survey conducted on the Italian population. Sleep Med 2004; 5:67-75.
- Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidermiology of insomnia: A longitudinal study in a UK population. Sleep 2007; 30: 274-280
- Rakel RE. Clinical and societal consequences of obstructive sleep apnoea and excessive daytime sleepiness. Postgrad Med 2009; 121:86-95.
- Al-Lawati NM, Patel SR, Ayas NT. Epidemiology, risk factors, and consequences of obstructive sleep apnoea and short sleep duration. Prog Cardiovasc Dis 2009; 51:285-293.
- Adewole OO, Hakeem A, Ayeni F, Anteyi E, Ajuwon Z, Erhabor G. Obstructive sleep apnoea among adults in Nigeria. J Natl Med Assoc. 2009; 101:720-725.
- Sogebi OA, Ogunwale A. Risk factors of obstructive sleep apnoea among Nigerian outpatients. Braz J Otorhinolaryngol. 2012; 6: 27-33.
- Akkoyunli ME, Altin R, Kart L, Atalay F, Ornek Y, Bayram M. Investigation of OSAS prevalence among long distance drivers from Zonguldak, Turkey. Multidisciplinary Respiratory Medicine Journal 2013; 8:10.
- Senthilvel E, Auckley D, Dasarathy J. Evaluation of sleep disorders in the primary care setting: History taking compared to Questionnaire. J Clin Sleep Med. 2011; 1: 41-48.
- Bjorvatn B, Gronli J, Pallesen S. Prevalence of different parasomnias in the general population. Sleep med 2010; 11: 1031-1034.
- Shittu RO, Issa BA, Olanrewaju GT, Odeigah LO, Sule AG, Sanmi MA, et al. Association between subjective sleep quality, hypertension, depression and BMI in a Nigerian Family practice setting. J Sleep Disorders Ther 2014; 2:234-239.
- Alebiosu OC, Ogunseni OO, Familoni OB, Adebayo PB, Ayodele OE. Quality of sleep among hypertensive patients in a semi-urban Nigerian community: a prospective study. Postgrad Med J.2009; 1: 166-172.
- Lemma S, Patel SV, Tarekegn YA, Tadesse MG, Berhane Y, Gelaye B. The epidemiology of sleep quality, sleep patterns, consumption of caffeinated beverages, and Khat use among Ethiopian college students. Sleep Disorders. 2012; 58; 11-21.
- Roepke SK, Ancoli-Israel S. Sleep disorders in the elderly. Indian J Med Res 2011; 131: 302-331.
- Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep 2004; 27.
- Park S, Cho MJ, Chang SM, Bae JN, Jeon HJ, Cho SJ, et al. Relationships of sleep duration with socio-demographic and health-related factors, psychiatric disorders and sleep disturbances in a community sample of Korean adults. J Sleep Res. 2010; 4: 567-77.
- Arber S, Bote M, Robert S. Gender and socio-economic patterning of self-reported sleep problems in Britain. Social Science & Medicine 2009; 68: 281-289.
- Kohlhuber M, Bolte G. Influence of environmental noice on sleep quality and sleeping disorders-implications for health. Bundesqesunheisblatt Gesundheitsforschung Gesundheitsschutz 2011; 54: 1319-1324
- Kohlhuber M, Bolte G. Influence of environmental noice on sleep quality and sleeping disorders-implications for health. Bundesqesunheisblatt Gesundheitsforschung Gesundheitsschutz 2011; 54: 1319-1324.
- Hume K. Sleep disturbance due to noise: current issues and future research. Noise health 2010; 12: 70-76.
- Omlin S, Brimk M. Awakening effects of church bell noise; Geographical extrapolation of the results of a polysomnographic field study. Noise Health 2013; 15:332-341.
- Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. Sleep disparity in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health 2010; 10:475.
- Zhang Q, Li L, Smith M, Guo Y, Whitlock G, Bian Z, et al. Exhaled carbon monoxide and its associations with smoking, indoor household air pollution and chronic respiratory diseases among 512000 Chinese adults. International Journal of Epidemiology 2013; 1–12.
- Kutty K. Sleep and chronic obstructive pulmonary disease. Curr Opin Pulm Med 2004; 10:104-112.
- Lewis DA. Sleep in patients with asthma and chronic obstructive pulmonary disease. Curr Opin Pulm Med 2001; 7:105-112.
- Mume CO, Olawale KO, Osundina AF. Excessive daytime sleepiness, nocturnal sleeps duration and psychopathology among Nigerian University students. South African Journal of Psychiatry 2011; 17: 108-111.
- Mume CO. Nightmare in schizophrenic and depressed patients. Eur J Psychiat 2009; 23.
- Aurora RR, Punjabi NM. Obstructive sleep apnoea and type 2 Diabetes: A bidirectional association. Lancet Respir Med 2013; 1: 329-339.
- Woods L, Craig TJ. The importance of rhinitis on sleep, daytime somnolence, productivity and fatigue. Curr Opin Pulm Med 2006; 12: 390-396.
- Lalluka T, Sares-Jaske L, Kronholm E, Saaksjavvi K, Lundvist A, Partonen R, et al. Socio-demographic and socio-economic differences in sleep duration and insomnia related symptoms in Finish adults. BMC Public Health 2012; 12: 565.
- Ogbolu RE, Avia OF, Famuyiwa OO, Erinfolami AR. A study of insomnia among psychiatry out patients in Lagos Nigeria. J sleep disorders Ther 2012; 1: 104.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.