Pellagra: A Possible Dermatological Complication of HIV Infection: A Case Report
Department of Internal Medicine, ESUT Teaching Hospital, Parklane, Enugu, Nigeria
- *Corresponding Author:
- Okafor Umezurike
Department of Internal Medicine
ESUT Teaching Hospital
Parklane, Enugu, Nigeria
Tel: +2348033130014
E-mail: umehughes@yahoo.com
Citation: Samuel E, et al. Pellagra: A Possible Dermatological Complication of HIV Infection: A Case Report. Ann Med Health Sci Res. 2020;10:823-825
This is an open access article distributed under the terms of the Creative Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non‑commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
HIV infection is global disease with more prevalence in low/middle income countries including Nigeria. It is associated with many complications and manifestations which may be infective or non-infective. The non-infective manifestations include pellagra which results from deficiency of niacin and tryptophan. HIV/AIDS causes pellagra through poor intake, absorption or metabolism of niacin/or tryptophan. Pellagra has characteristics presentations of dermatitis, diarrhea and dementia. We report a case of a 32 year old woman who was being managed for HIV infection, presented with pellagra. She responded well to niacin replacement therapy. The aim of this case report is to highlight HIV infection as a cause of pellagras.
Keywords
Pellagra; Niacin; Dermatitis; Diarrhea; Dementia
Introduction
Pellagra is a disorder that results from inadequate dietary intake or impaired absorption of niacin and/or tryptophan, manifested by a characteristic dermatitis. It usually presents as a clinical triad of diarrhea, dermatitis and dementia. [1,2] The dermatitis occurs mainly in exposed areas of the skin, beginning as a pruritic skin erythema and later causing a broad band of dermatitis around the neck. The diarrhea is usually profuse, may be bloody and occasionally associated with glossitis and stomatitis. Dementia is a late complication, however patients with pellagra also presents with other neuropsychological manifestations including anxiety, depression, tremulousness, hyporeflexia and in severe cases encephalopathy. [2-4]
Pellagra was first described among the poor peasants of the Asturias province of Spain in 1735 by Don Gasper cassal, a Spanish court physician; however the term pellagra was derived from the Italian words “PELLE AGRA” meaning rough skin. It was considered to be an infectious disease until the early 20th century when Joseph Goldberger succeeded in proving that the disease was caused by nutritional deficiency. [2-4] It is caused by cellular deficiency of niacin or its precursor tryptophan. Niacin is an essential component of several coenzymes involved in several metabolic pathways and its deficiency is associated with other vitamin deficiencies like thiamine, riboflavin and pyridoxine.
In HIV, oxidation of tryptophan along the kynurenine pathway, and chronic inflammation, is considered to be the main cause of tryptophan depletion and hence niacin deficiency. In addition, malnutrition as a result of mal-absorption and chronic diarrhea in patients with HIV may also contribute to the disease. In South Africa, tryptophan deficiency has been associated with lower CD4 counts and patients not yet on ART. [5] HIV infection induces pellagra like state; plasma tryptophan levels are decreased in patients with HIV infection and high dose nicotinamide treatment may successfully reverse this HIVinduced metabolic abnormality. [6] Thus it has been hypothesized that, HIV infection induces niacin depletion and therapeutic niacin would be a secondary preventive measure for pellagra in patients with HIV infection [6]. Isoniazide and pyrazinamide use in prophylaxis and/treatment of tuberculosis in HIV patients has been associated with development of pellagra. [7]
Pellagra is becoming a rare disease with improvement in diet and global fortifications of food, however with emergence of HIV and its antecedent complications including Pellagra, there should be high index of suspicion in HIV patients with photosensitive dermatitis. Thus the aim of this case report is to bring to the fore pellagra as a complication of HIV.
Case Presentation
A 32-year-old unemployed woman who was newly diagnosed of living with human immunodeficiency virus (HIV) presented to the emergency with diarrhea and fever of 5 and 1 month respectively. The diarrhea was non mucoid, non-bloody, about 200 ml per void and with a frequency of about 5 times daily. There was no tenesmus, dyschezia and the colour was normal. The diarrhea has been recurrent with the current episode starting about 3 weeks before presentation. There was no associated nausea, vomiting, abdominal pain or distension but had anorexia. Her diet was mainly staple food of rice, yam, beans and cassava based meals.
She also had a low grade fever of a month duration, intermittent but not associated with rigors, chills or night sweat. She had weakness, dizziness and weight loss. She developed pruritic rashes mainly around her neck, upper chest wall, and both legs. She was not allergic to any allergen including drugs. She was noticed to be forgetful and occasionally delusional but there were no seizures or impairment of consciousness. She commenced highly active antiretroviral therapy 3 weeks before presentation. Has received treatment for the diarrhea and also the HAART from another hospital.
She is married but childless; neither takes alcohol nor tobacco in any form. She does not have hypertension and diabetes mellitus.
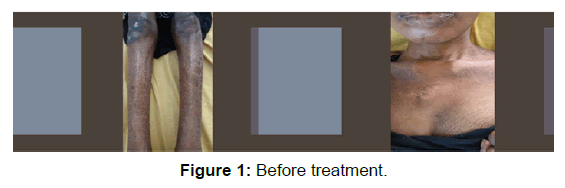
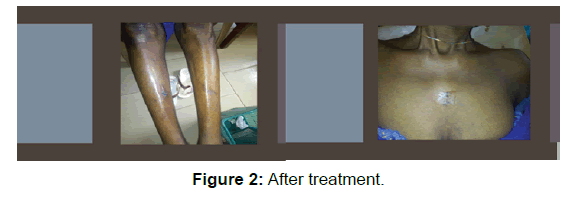
On clinical examination, she was chronically ill looking, cachectic, not in respiratory distress, febrile (temperature of 37.8°C), pale, anicteric, but not dehydrated and does not have significant peripheral lymphadenopathy and edema. She had hyper pigmented scaly (fish like) rashes intersperced with normal skin on the chin, neck, upper part of the chest (cassals necklace), both legs and feet. They were non papular and nonerythematous. There was no abnormality detected in the other systems examined including the abdomen.
An impression of HIV/AIDS complicated by pellagra and septicemia was made. Laboratory investigations showed normocytic normochromic anemia, and neutrophilia, CD4 cell count was 190/ul, urine and stool analysis were normal. The liver function test, serum electrolyte, urea and creatinine, the abdominopelvic ultrasound and chest X ray were also normal.
She was commenced on antibiotics (cefuroxime), oral nicotinamide 100 mg twice daily and other haematinics. The HAART regimen was sustained. Patient had good response to the treatment as the diarrhea and fever abated by the 3rd day, rashes noted to be resolving by the end of 1st week and patient became stable, started gaining weight and was discharged to medical outpatient by the 3rd week on tabs nicotinamide, haematinics and HAART. She has been regular to follow up, adherent to medication and has remained stable [Figure 1 and Figure 2].
Discussion
Patients living with HIV are at risk of developing wide array of complications affecting almost all the organs in the body. The complications were dominated by opportunistic diseases (infections and malignancies) during the pre HAART era. With improvement in the understanding and management of the infection, morbidity and survival has improved. However this has been associated with emergence of novel complications including pellagra as reported in the index case.
Pellagra, a disease associated with low level of vitamin B3 (niacin), is characterized by dermatitis, diarrhea, dementia and without proper intervention ultimately leads to death. [1,3,4,8] Our patient presented with dermatitis, diarrhea and early stages of dementia. The dermatitis is usually photosensitive, and mainly induced by ultra violet light, it presents as macular rashes affecting mainly the exposed areas of the skin as in the index patient where the rashes were mainly on the legs, forearm, hands, neck and shoulder. Diarrhea is a common presentation in patients with HIV and can be due to infective and non-infective causes. Pellagra has been implicated as a cause of diarrhea in HIV infected patients. Diarrhea in pellagra usually results from loss of brush border cells which with other rapidly dividing cells in the body is affected in these patients. Neurological manifestations in pellagra are usually a late presentation and range from restlessness to dementia. Our patient presented with delusion and forgetfulness which recovered completely following treatment.
There are various causes of pellagra and usually classified as either primary (dietary deficiency of niacin/tryptophan) or secondary (inability to utilize the niacin in the diet). Both primary and secondary causes of pellagra is prevalent in patients with HIV/AIDS. [5,9] These patients are usually ill with associated malaise, anorexia, nausea and occasionally vomiting which limit dietary intake. Also dietary deficiencies occur when the diet lacks niacin/tryptophan containing food like liver and other animal product. The index patient was anorexic, ill-looking and had malaise and her meals lacked niacin rich food. Mal-absorption is a common presentation in patients with HIV/AIDS and this leads to impaired absorption of niacin and tryptophan leading to development of pellagra. [10] Our patient, who is diagnosed of HIV infection, was unemployed, from a low socioeconomic and had diarhoea with associated malabsorption. All these could have contributed to her development of pellagra. Features of other aetiologies of pellagra including alcoholism, inflammatory bowel disease, celiac disease, Hartnup disease and carcinoid syndrome were not found in our patient. Thus this patient developed pellagra as a complication of HIV infection which responded well to replacement of the niacin.
Conclusion
The prevalence of pellagra was thought to be decreasing however with the emergence of HIV and its associated complications of malnutrition, there should be high index of suspicion of pellagra in HIV/AIDS patients presenting with photosensitivity dermatitis. Response to therapy is good especially when commenced early, however delay in diagnosis and treatment can be debilitating and usually fatal.
Finally, health workers in resource poor countries attending to HIV/AIDS patients should be equipped with clinical knowledge to be able to diagnose pellagra early amidst lack of diagnostic facilities.
Competing Interests
The authors declare that they have no competing interests.
References
- Piqué-Duran E, Pérez-Cejudo JA, Cameselle D, Palacios-Llopis S, García-Vázquez O. Pellagra: A clinical, histopathological, and epidemiological study of 7 cases. Actas Dermosifiliogr. 2012;103: 51-58.
- Malfait P, Moren A, Dillon JC, Brodel A, Begkoyian G, Etchegorry MG, et al. An Outbreak of Pellagra Related to Changes in Dietary Niacin among Mozambican Refugees in Malawi. International Journal of Epidemiology, 1993;22: 504-511.
- World Health Organization. The Management of nutrition in major emergencies. 2000.
- Hegyi J, Schwartz RA, Hegyi V. Pellagra: Dermatitis, dementia, and diarrhea. Int J Dermatol. 2004;43: 1-5.
- Bipath P, Levay PF, Viljoen M. Tryptophan depletion in context of the inflammatory and general nutritional status of a low-income South African HIV-infected population. J Health Popul Nutr. 2016;35: 5.
- Murray M. Niacin as a potential AIDS preventive factor. Med Hypotheses. 1999;53: 375-379
- Kipsang JK, Choge JK, Marinda PA, Khayeka-Wandabwa C. Pellagra in isoniazid preventive and antiretroviral therapy. ID Cases. 2019;17: e00550.
- James W, Berger TG, Elston D. Andrew’s diseases of the skin: Clinical dermatology. London: Saunders/Elsevier, UK. 2011.
- Del Pozo J, Martínez W, Regueiro MV. Pellagra and HIV infection. Actas Dermosifiliogr 2000;91: 157-162.
- Ahmadu BU, Emmanuel P, Manchan DB. Pellagra, a re-emerging disease: a case report of a girl from community ravaged by insurgent. PAMJ 2019;33: 195.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.