Perception of Nurses about Palliative Care: Experience from South‑West Nigeria
- *Corresponding Author:
- Dr. Joseph O Fadare
Department of Pharmacology, Ekiti State University, Ado-Ekiti, Nigeria.
E-mail: jofadare@gmail.com
Abstract
Background: Nurses play a major role all over the world in the palliative care team. Aim: The aim of this study was to investigate the knowledge and attitude of nurses toward palliative care in a tertiary level hospital in Nigeria. Subjects and Methods: Setting: This cross‑sectional questionnaire‑based study was carried out among nurses at a tertiary health care facility in Ado‑Ekiti, South‑West Nigeria. A cross‑sectional questionnaire‑based study was carried out. The questionnaire sought information about the sociodemographic profile of respondents, their knowledge of definition and philosophy of palliative care among other things. Descriptive statistics was used to obtain the general characteristics of the study participants, while Chi‑square was used to determine the association between categorical variables. A two‑sided P < 0.05 was considered as significant. Results: A total of 100 questionnaires were returned with a female preponderance among the respondents with F: M ratio of 9:1. Regarding the definition of palliative care, 71.8% (48/66) of the respondents understood palliative care to be about pain medicine, 55% (33/60) thought it to be geriatric medicine, while 90.2% (83/92) felt palliative care is about the active care of the dying. Exactly 80.5% (66/82) respondents agreed that palliative care recognizes dying as a normal process while 84.1% (74/88) respondents were of the opinion that all dying patients would require palliative care. The use of morphine would improve the quality of life of patients according to 68.9% (42/61) of respondents. Conclusion: There are gaps in the knowledge of healthcare workers in the area of palliative care and this call for a review of the current nursing curriculum and practice guidelines in Nigeria.
Keywords
End of life, Nurses’ attitude, Pain management, Palliative care
Introduction
Palliative care is an emerging area of medicine that aims to improve the quality of life of patients with chronic diseases such as cancer, end-stage heart failure, and chronic obstructive airways disease. [1,2] The palliative care team is usually made up of nurses, medical doctors, pharmacists, social workers, spiritual leaders, and psychologists. [3,4] Nurses by the nature of their jobs play a major role in the palliative care team as they are usually in constant touch with patients and their relatives. The knowledge and skills of palliative care among nurses will definitely affect the quality of palliative care being offered in a particular center. In Nigeria, palliative care units has only been established in a few tertiary health care facilities recently [5] and knowledge of nursing staff toward palliative care has not previously been investigated. Previous works relating to palliative in Nigeria have been centered on the history and challenges of palliative care in Nigeria, knowledge and attitude of patients to palliative care and truth-telling for cancer diagnosis and prognosis. [6-8] The aim of this work is to explore nurses’ knowledge and attitudes toward palliative care in an emerging tertiary care center in the South-Western part of Nigeria where a palliative care unit has just commenced operations.
Subjects and Methods
Study setting
This study was carried out among the nursing staff of the Ekiti State University Teaching Hospital, a tertiary level care health facility located in Ado-Ekiti, South-West Nigeria during the month of April, 2013. This center has medical specialists in Internal Medicine, Family Medicine, Surgery, Psychiatry, Pediatrics, Anesthesia and Community Medicine. It also has a large component of nursing staff and an affiliated school of nursing where training at undergraduate and postgraduate levels is being done.
Methods
This study was a questionnaire-based cross-sectional study among the different categories of nurses in the hospital. The nursing staff is classified according to their seniority in ascending order as: Nursing Officer (NO), Senior NO, Principal NO, Assistant Chief NO (CNO), CNO, and Deputy Director of Nursing Services.
Study instrument
The questionnaire was adapted from one used for a similar study carried out in Oman [9] with changes made to reflect local realities. It was pretested among ten nurses in another tertiary healthcare facility in Ekiti State and necessary revisions made before being administered to the participants. The instrument demonstrated a high internal consistency reliability coefficient (Cronbach’s alpha = 0.79).
Sampling
A minimum sample size of 95 was estimated using Fischer’s formula:

(Where N = Minimum sample size, Z = Standard normal deviate usually set at 1.96, P = Proportion of people with a particular characteristic (11% in this case, i.e. 0.11), Q = 1 - P (0.89) and D = Degree of accuracy usually set at 0.05).
However, 120 questionnaires were distributed to make allowance for nonrespondents and to give the study better power.
A random sampling of the nursing staff was done, and the questionnaires were distributed to the participants through various unit heads. The nurses were informed of the voluntariness of participating in the study, and their confidentiality was assured by the absence of identifiers on the questionnaire. They were to be filled during any of the unit activities and returned to a collection point in their unit or department. The time frame for collection of the questionnaire from the unit heads was 1 week, and any questionnaire returned after that period was not included for data analysis. The questionnaire apart from the age, duration of practice and professional position of respondents had sections about knowledge of palliative care, its philosophy, communication issues and medications used among others.
Data analysis
The information obtained from the questionnaire was coded, entered, and analyzed using IBM SPSS version 19 (IBM Corporation, Armonk, NY, USA). Analysis was performed using descriptive statistics was used to obtain the general characteristics of the study participants. Chi-square test was used to determine the level of significance of groups of categorical variables P < 0.05 were considered as significant.
Ethical considerations
Ethical clearance was obtained from the Hospital Research Ethics Committee before the commencement of the study. The filling and submission of the questionnaires by the nurses were taken as their explicit consent.
Result
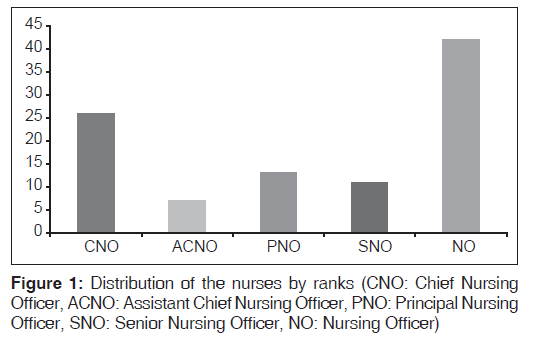
One hundred questionnaires were returned and used for analysis, a response rate of 83.3% (100/120). Females constituted majority 90% (90/100) of the respondents and the mean age was 39.3 (9.9) years with a 95% confidence interval of 37.3-41.3 years. The distribution of the nurses according to their ranks is shown in Figure 1. Almost half of the respondents (46/100) had practiced for more than 10 years, 24% (24/100) for between 5 and 10 years and the remaining 30% for <5 years. Regarding the respondents understanding of palliative care, 71.8% (48/66) knew that it was mainly about pain medicine, while 55% (33/60) felt that it was about geriatric medicine. Eighty-three (90.2%) were convinced that palliative care was about the active care of the dying while 64.6% (42/65) believed that it was synonymous with rehabilitation medicine. There was a statistically significant difference among the various categories of nursing staff in the area of definition of palliative care as active care of the dying (P = 0.04). There was no statistically significant difference in the nurses definition of palliative care as pain medicine (P = 0.51), geriatric medicine (P = 0.51), and rehabilitation medicine (P = 0.35). The responses of participants regarding the philosophy of palliative care and the patients requiring it are shown in Table 1.
| Yes (%) | No (%) | Don’t know (%) | χ2 | 95% CI | |
|---|---|---|---|---|---|
| Philosophy of palliative care | |||||
| Affirms life | 40 (62.5) | 17(26.6) | 7 (10.9) | 0.28 | 0.21-0.39 |
| Recognizes dying as a normal process | 66 (80.5) | 14(17.1) | 2 (2.4) | 0.24 | 0.12-0.28 |
| Hastens death | 8 (13.8) | 48(82.8) | 2 (3.4) | 0.03 | 0.00-0.06 |
| Prolongs life | 67 (90.5) | 5(6.8) | 2 (2.7) | 0.02 | 0.00-0.05 |
| Palliative care is needed for | |||||
| All dying patients | 74 (84.1) | 14(15.9) | 0 | 0.89 | 0.85-0.97 |
| Metastatic cancer with uncontrolled pain | 66 (88) | 8 (10.75) | 1 (1.3) | 0.09 | 0.07-0.21 |
| End stage heart failure | 44 (71) | 17 (27.45) | 1 (1.6) | 0.12 | 0.08-0.22 |
| Debilitating illness like rheumatoid arthritis | 50 (82) | 9 (14.7) | 2 (3.3) | 0.34 | 0.21-0.39 |
CI: Confidence interval
Table 1: Nurse’s knowledge of the philosophy of palliative care
Fifty-nine respondents (79.7%) recognized delirium as a major nonpain symptom seen in palliative medicine, while breathlessness was also chosen by 80% (56/65) of the participants (statistically significant difference with a P < 0.001 and P < 0.01, respectively). Regarding the communication of prognosis to the patient, 83.9% (68/80) of the nurses felt that is the right thing to do and 92.2% (70/76) of respondents acknowledged that patient wishes should always be respected. Apart from medical doctors, nurses, pharmacists and social workers, religious leaders were also recognized by 89.2% (74/83) of respondents as part of the palliative care team. Advanced medical directive was recognized as a document through which the patient states his preferences about future medical practices by 85.6% (77/90) of respondents while 67.2% (39/57) of the nurses knew that it was synonymous with the term “living will”. The respondents’ knowledge about the use of morphine and pentazocine in palliative care is shown in Table 2. Pain and symptom management, clear decision-making and preparation for death were identified as components of a good death by 90.1% (73/81), 89.6% (61/67) and 90.2% (74/82) respondents respectively.
| Yes (%) | No (%) | Don’t know (%) | χ2 | 95% CI | |
|---|---|---|---|---|---|
| Morphine | |||||
| Causes death in all dying patients | 11 (17.5) | 49 (77.8) | 3 (4.7) | 0.42 | 0.29-0.46 |
| Improves quality of life | 42 (68.9) | 13 (21.3) | 6 (9.8) | 0.75 | 0.71-0.87 |
| Relieves all kinds of pain | 78 (89.7) | 7 (8) | 2 (2.3) | 0.03 | 0.00-0.06 |
| Relieves breathlessness in heart failure | 23 (37.7) | 32 (52.5) | 6 (9.8) | 0.31 | 0.28-0.47 |
| Pentazocine | |||||
| Causes death in all dying patients | 10 (16.7) | 42 (70) | 8 (13.3) | 0.01 | 0.001-0.09 |
| Improves quality of life | 49 (75.4) | 12 (18.55) | 4 (6.1) | 0.82 | 0.82-0.94 |
| Relieves all kinds of pain | 84 (87.5) | 10 (10.4) | 2 (2.1) | 0.03 | 0.002-0.08 |
| Relieves breathlessness in heart failure | 22 (33.8) | 38 (58.5) | 5 (7.7) | 0.04 | 0.00-0.06 |
CI: Confidence interval
Table 2: Nurse’s knowledge about use of opioid analgesics
Discussion
The knowledge of respondents regarding the definition, philosophy and potential beneficiaries of palliative care was surprisingly very good considering that palliative care is a relatively new branch of medicine in Nigeria. The preponderance of female nurses among our study population reflects the general trend of gender distribution in the nursing profession. Regarding the definition of palliative care, majority (90.2%) of the nurses in our study knew that palliative care was about the active care of the dying, higher than 60.3% found in a study among medical undergraduates in Oman. [9] One of the major objectives of palliative care is to affirm life while recognizing death as a normal process. In a study among nurses in Lebanon, 84.6% of them recognized this objective, a finding at variance from 62.5% found among our respondents. [10] The belief that palliative care is mainly for cancer patients was again reflected in our study. However, it is interesting to note that 88% of the nurses felt that all dying patients would require palliative care. This is more than 34.2% found in the earlier cited study among medical undergraduates in Oman. [9] The importance of palliative care in other chronic conditions like end stage heart failure and HIV/AIDS has been emphasized in various studies. [11,12] The contribution of palliative care to better management of HIV/AIDS patients have been demonstrated in Uganda. In a study carried out in India, only 19.3% of medical undergraduates knew that patients with end stage heart failure are candidates for palliative care, lower than 71% in our study. [13] The communication of bad news (diagnosis or prognosis) to patients has always been a controversial issue. According to ethical norms, competent patients have a right to have all information regarding their medical condition. This is not so in practice because of the influence of many factors such as culture, religion and patient’s peculiarities. [14,15] In this study, 83.9% of the nurses thought that the patient should be informed of their prognosis, the same response from a Lebanese study among nurses. [10] The knowledge of advanced medical directives among participating nurses was encouraging despite the fact that it is a relatively new concept in developing countries like Nigeria. The use of opioid analgesics like morphine in patients with chronic life-threatening conditions has always been associated with a lot of misconceptions. [16,17] Our study showed that 17.5% of respondents felt that the use of morphine would hasten death while 89.7% believed that morphine relieves all kinds of pain. A study among general practitioners in Italy showed that 22.2% feared that opioids would shorten the patient’s lifespan while 32.5% were afraid of the side-effects of the drug. [18] Bernardi et al. in their study also found significant gaps in the knowledge of Italian oncology nurses about opioid use in patients. [19] Another study among nurses in Turkey showed that they have inadequate knowledge about the management of cancer pain while the most frequent errors in a Brazilian study among healthcare workers were related to the use of opioids. [20,21]
The knowledge of nurses about palliative care depends a lot on training both at undergraduate and postgraduate levels. Adriaansen et al. found out that attendance of postqualification courses in palliative care by nurses has a positive effect especially in the area of pain and symptom management. [22] Studies among nurses have reported improved confidence in pain management after interventions such as educational programs, [23,24] Efforts to integrate palliative care into the nursing undergraduate curriculum in an Australian university have been described by Ramjan et al. [25] The implications of the study findings for nursing practice in Nigeria is the need for a practice-based palliative care training program, especially in the area of its philosophy, the group of patients requiring palliative care and the use of opioid analgesics in this group of patients.
Future research directions in the area of palliative care nursing in Nigeria should focus on pre- and post-interventional studies in the use of opioids in palliative care.
Study limitations
The bias of the respondents towards certain issues and incidence of skipped questions are some limitations encountered in this study. To address this, respondents were asked not to disclose their identities and were re-assured that the study was strictly for research. While the results of our study may not be generalizable for the whole country, it may reflect the situation in similar tertiary healthcare institution in Nigeria.
Conclusion
While the level of knowledge of Nigerian nurses regarding the definition and philosophy of palliative care is impressive, there are significant gaps in other areas. The need for continuous medical education for nurses and more importantly the undergraduate nursing curriculum should be reviewed to include this emerging branch of medicine.
Acknowledgment
The authors are grateful to all the nursing staff who participated in this study and the authorities of the Ekiti State University Teaching Hospital, Ado-Ekiti, Nigeria who supported the study.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Harding R, Higginson IJ. Palliative care in sub-Saharan Africa. Lancet 2005;365:1971-7.
- Smith AK, Thai JN, Bakitas MA, Meier DE, Spragens LH, Temel JS, et al. The diverse landscape of palliative care clinics. J Palliat Med 2013;16:661-8.
- Smith TJ, Coyne PJ, Cassel JB. Practical guidelines for developing new palliative care services: Resource management. Ann Oncol 2012;23 Suppl 3:70-5.
- Soyannwo OA. Palliative care and nursing. Afr J Med Med Sci 2009;38 Suppl 2:67-70.
- Onyeka TC, Velijanashvili M, Abdissa SG, Manase FA,
- Kordzaia D. Twenty-first century palliative care: A tale of four nations. Eur J Cancer Care (Engl) 2013;22:597-604.
- Onyeka TC. Palliative care in enugu, Nigeria: Challenges to a new practice. Indian J Palliat Care 2011;17:131-6.
- Nwankwo KC, Ezeome E. The perceptions of physicians in southeast Nigeria on truth-telling for cancer diagnosis and prognosis. J Palliat Med 2011;14:700-3.
- Adenipekun A, Onibokun A, Elumelu TN, Soyannwo OA. Knowledge and attitudes of terminally ill patients and their family to palliative care and hospice services in Nigeria. Niger J Clin Pract 2005;8:19-22.
- Jahan F, Shibli HS, Qatan RS, Al Kharusi AA. Perception of undergraduate medical students in clinical years regarding palliative care. Middle East J Age Ageing 2013;10:22-31.
- Abu-Saad Huijer H, Dimassi H. Palliative care in Lebanon: Knowledge, attitudes and practices of physicians and nurses. J Med Liban 2007;55:121-8.
- Shah AB, Morrissey RP, Baraghoush A, Bharadwaj P, Phan A, Hamilton M, et al. Failing the failing heart: A review of palliative care in heart failure. Rev Cardiovasc Med 2013;14:41-8.
- Kell ME, Walley JD. Palliative care for HIV in the era of antiretroviral therapy availability: Perspectives of nurses in Lesotho. BMC Palliat Care 2009;8:11.
- Bogam RK, Kumbhar SM, Sahu SB, Marie AS, Sagare SM, Chowdhury YS. Knowledge of palliative care among undergraduate medical students in rural medical college of Maharashtra. Natl J Community Med 2012;3:666-9.
- Windsor JA, Rossaak JI, Chaung D, Ng A, Bissett IP, Johnson MH. Telling the truth to Asian patients in the hospital setting. N Z Med J 2008;121:92-9.
- Tavakol M, Murphy R, Torabi S. Educating doctors about breaking bad news: An Iranian perspective. J Cancer Educ 2008;23:260-3.
- Murnion BP, Gnjidic D, Hilmer SN. Prescription and administration of opioids to hospital in-patients, and barriers to effective use. Pain Med 2010;11:58-66.
- Salvato C, Aretini G, Serraglia D, Terrazzani G, Debetto P, Giusti P, et al. Opioid prescription for terminally ill outpatients in a district of northern Italy: A retrospective survey. Pharmacol Res 2003;48:75-82.
- Bernardi M, Catania G, Lambert A, Tridello G, Luzzani M. Knowledge and attitudes about cancer pain management: A national survey of Italian oncology nurses. Eur J Oncol Nurs 2007;11:272-9.
- Yildirim YK, Cicek F, Uyar M. Knowledge and attitudes of Turkish oncology nurses about cancer pain management. Pain Manag Nurs 2008;9:17-25.
- de Freitas GR, de Castro CG Jr, Castro SM, Heineck I. Degree of knowledge of health care professionals about pain management and use of opioids in pediatrics. Pain Med 2014;15:807-19.
- Adriaansen MJ, van Achterberg T, Borm G. Effects of a postqualification course in palliative care. J Adv Nurs. 2005;49:96-103.
- Shipman C, Burt J, Ream E, Beynon T, Richardson A, Addington-Hall J. Improving district nurses’ confidence and knowledge in the principles and practice of palliative care. J Adv Nurs 2008;63:494-505.
- Hansen L, Goodell TT, Dehaven J, Smith M. Nurses’ perceptions of end-of-life care after multiple interventions for improvement. Am J Crit Care 2009;18:263-71.
- Ramjan JM, Costa CM, Hickman LD, Kearns M, Phillips JL. Integrating palliative care content into a new undergraduate nursing curriculum: The University of Notre Dame, Australia – Sydney experience. Collegian 2010;17:85-91.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.