Prevalence and Predictors of Erectile Dysfunctions among Men on Antiretroviral Therapy in South‑western Nigeria
- *Corresponding Author:
- Dr. Oluwatosin Adediran Adeoye
Department of Community Medicine
LAUTECH Teaching Hospital
Ogbomoso, Oyo State, Nigeria
E-mail: tosinadeoye2002@yahoo.com
Citation: Adebimpe WO, Omobuwa O, Adeoye OA. Prevalence and predictors of erectile dysfunctions among men on antiretroviral therapy in South-Western Nigeria. Ann Med Health Sci Res 2015;5:279-83.
Abstract
Background: Erectile dysfunctions (EDs) are common presentations among men on anti‑retroviral therapy, many of who had a course to discontinue anti‑retroviral drugs or search for alternative treatments. Aim: This study assessed the prevalence and predictors of ED among men on anti‑retro viral therapies (ART) in a Nigerian population. Subjects and Methods: It was a descriptive cross‑sectional survey among 234 HIV‑positive men on anti‑retroviral therapy selected using stratified sampling method after excluding for co‑morbidities. Research instrument was semi‑structured interviewer administered questionnaire, and data were analyzed using the SPSS software version 17.0 (Chicago IL, USA), while binary logistic regression and Chi‑square test were used to demonstrate association between selected categorical variable. Results: Mean age of respondents was 37.1 (1.6) years, 85.6% have not missed their medications, self‑reported adherence was reported as good among 213 [(90.8 %) 213/234], though calculated adherence was 90% among as many as 201 [(85.6%) 201/234]. Pattern of EDs revealed weak erection among 42 [(37.8%) 42/111], 15 [(13.5%) 15/111] said they could no longer achieve erection, 33 [(29.7%) 33/111] said they could not maintain erections, while 27 [(24.3%) 27/111] presented with loss of libido. Delayed and premature ejaculations were reported among 24 [(21.6%) 24/111] and 8 [(7.2%) 8/111] respectively. About 14% (33/234) of respondents said that anti‑retroviral drugs could have caused their ED while 78% (183/234) said it should not. A statistically significant association exists between having weak erections and age above 65 years and calculated the adherence <95%, while none exists between having weak erections and missing pills. Conclusion: Anti‑retroviral drugs are common causes of EDs. Concerns of clients should always be addressed most especially issues that may compromise adherence.
Keywords
Adherence, Anti-retroviral therapy, Erectile dysfunction
Introduction
Studies have shown an association between anti-retro viral therapies (ART) and different degrees of sexual dysfunction in men.[1-3] The highest rates of dysfunction are associated with Indinavir and the lowest with Nevirapine.[2] Among people living with HIV/AIDS (PLWHA) on ART, sexual dysfunctions have been reported in form of erectile dysfunction (ED) (9–74%), ejaculatory disturbances (36–42%), and low sexual desire (24–73%).[3] Ejaculatory dysfunction has been shown to be associated with the use of didanosine, as well as other protease inhibitors.[3,4]
These sexual dysfunctions could be of psychogenic or organic etiology.
There is also a subdivision into mental, hormonal, pharmacological, and other morbid conditions. Hypogonadism was one of the most frequent causes of sexual dysfunction before the advent of highly active anti-retroviral therapy (HAART), and it still remains the most common endocrine disorder of HIV-infected men.[5] After receiving the diagnosis of HIV infection, it is common for people to experience negative moods, show less interest in sex and decrease the frequency of sexual activity. Depression is one of the important mental factors associated with sexual dysfunctions.[1,6]
In addition, HIV-infected individuals use many other medications that could also be associated with decreased sexual responses. Medications such as ketoconazole, fluconazole, ganciclovir, megestrol, methadone, and antipsychotics including antidepressants may decrease testosterone levels and cause sexual dysfunctions.[7] Sexual dysfunction has an impact on the quality of life and very often leads to negative attitudes on the part of the individual, including poor adherence to antiretroviral (ARV) regimens and to safer sex strategies.[8-10]
Huge data gap exists on pattern of ED in Nigeria most especially among PLWHA. Even among few studies done outside Nigeria, most emphasis were laid on 2nd line ART and clients on salvage therapy, with little or no emphasis on clients on first line ART which constitutes majority of HIV-positive Nigerians on ART addressed by this study. Despite few prevalence figures reported, the pathophysiology of sexual dysfunction in the HAART era is still not completely understood. We investigated the prevalence of ED in a cohort of HIV-infected people on ART, to identify risk factors for developing ED among HIV-infected men especially in developing countries where many socio-economic factors influence clients’ management and outcomes.
Subjects and Methods
Study design
The study was a descriptive cross-sectional survey carried out in Osogbo, Osun State.
Study area
Osogbo is the capital of Osun State in South-western Nigeria. HIV treatment, care and support in the capital city, takes place in the secondary (State Government Hospital) and tertiary (State Government University Teaching Hospital) health care levels. Primary health care centers were mainly for HIV counseling and testing services, and were excluded from this study. HIV prevalence in the city was 2.5%, a bit lower than the national average put at 4.1%.
Study population
Target population constitutes HIV positive men accessing treatment in some selected health facilities. Eligible men would have been on ART for at least 1-year. In addition, men on medications that could influence erectile functions (such as ketoconazole, fluconazole, ganciclovir, megestrol, methadone, and antipsychotics including antidepressants) were totally excluded from this study. Co-morbidities such as hypertension and diabetes that could also serve as confounders were also excluded among study participants through past medical history. Using Leslie Fischer’s formula for calculation of sample size for the population < 10,000, a sample size of 221 was estimated, and this was increased to 240 to account for non-response. A total of 250 questionnaires were taken to the field.
There were two eligible facilities in Osogbo, Asubiaro General Hospital, which is secondary, and LAUTECH Teaching Hospital which is tertiary in nature, and both have about 2000 registered clients on ART. Questionnaires were equally shared among the 2 facilities. On a bi-weekly clinic day per facility, a list or sampling frame of all eligible men was obtained from the triage nurse. A systematic sampling of one in three eligible men on the list was done, and this continued until the questionnaires allocated for that day got exhausted. Apart from pre-testing and training of data collectors, data validity were further ensured by translating and back-translating the questionnaire between English and the native Yoruba languages-to assist further understanding among the illiterate and semi-literate respondents. Study period was from January 2013 to June 2013.
Data were collected by trained research assistants using pre-tested interviewer administered semi-structured questionnaires. Interviews were conducted under strict confidentiality and privacy in the post-test counseling rooms of the clinics. Details of the study and its objectives were explained to all respondents and participation voluntary, informed consent was obtained from each participant. Ethical clearance was obtained from Osun State University, Osogbo ethical review committee. Permission was also obtained from the Project Coordinators of the respective HIV/ART program as well as the Medical Director of the health facilities used.
Questionnaires were manually sorted out and data obtained were entered into the computer. Statistical Package for social Sciences (SPSS) version 17 (Chicago IL, USA) was used to analyze the double-entered data that were also checked for outlier values to ensure its validity. Frequency tables were generated, and relevant summary measures calculated. The Chi-square test was used to demonstrate an association between categorical variables while level of significance for the statistical tests was considered at P < 0.05.
Results
Mean age of respondents was 37.1 (1.6) years, 88.2% (207/234) were married, and 74.8% (175/234) had up to secondary school level education as seen in Table 1. Table 2 showed that about 85.6% (201/234) have not missed their medications, self-reported adherence was reported as good among 90.8% (213/234), though calculated adherence was 90% among as many as 85.6% (201/234).
| Variable | Frequency (n=234) | Percentage |
|---|---|---|
| Age group (years) | ||
| 20-39 | 78 | 33.3 |
| 40-59 | 135 | 57.7 |
| 60-79 | 21 | 9.0 |
| Marital status | ||
| Single | 12 | 5.3 |
| Married | 207 | 88.2 |
| Divorced/separated | 15 | 6.5 |
| Education level | ||
| None | 25 | 10.7 |
| Primary | 74 | 31.6 |
| Secondary | 76 | 32.5 |
| Tertiary | 59 | 25.2 |
| Occupation | ||
| Student | 6 | 2.6 |
| Trader | 40 | 17.1 |
| Farmer | 19 | 7.9 |
| Artisan | 80 | 34.2 |
| Professionals | 15 | 6.6 |
| Civil servants | 55 | 23.7 |
| Unemployed | 19 | 7.9 |
| Religion | ||
| Christian | 132 | 56.6 |
| Islam | 96 | 40.8 |
| Traditional | 3 | 1.3 |
| Others | 3 | 1.3 |
Table 1: Sociodemographic characteristics of respondents
| Variable | Frequency (n=234) | Percentage |
|---|---|---|
| Missed medications | ||
| In the last 6 months | 15 | 6.6 |
| In the last 1-month | 9 | 3.9 |
| In the last 1-week | 9 | 3.9 |
| None | 201 | 85.6 |
| Self-reported adherence | ||
| Good | 213 | 90.8 |
| Bad | 9 | 3.9 |
| Can’t say | 12 | 5.3 |
| Calculated adherence | ||
| <90 | 43 | 18.4 |
| 90-95 | 188 | 80.3 |
| >95 | 3 | 1.3 |
| Duration of | ||
| commencement of ART | ||
| 1-5 years | 194 | 82.9 |
| >5 years | 40 | 17.1 |
| ART regimen | ||
| 1st line | 234 | 100.0 |
| 2nd line | 0 | 0 |
| ART: Anti-retroviral therapy |
Table 2: Pattern of adherence to ART
Pattern of EDs as shown in Table 3 revealed weak erection among 37.8% (42/111), 13.5% (15/111) said they could no longer achieve erection, 29.7% (33/111) said they could not maintain erections, while 24.3% (27/111) presented with loss of libido.
| Variable (n=111 with multipleresponses) | Frequency(n=111) | Percentage |
|---|---|---|
| My erection is now weaker thanbefore | 42 | 37.8 |
| Cannot achieve erection again | 15 | 13.5 |
| Could not sustain erection for longduring sexual intercourse | 33 | 29.7 |
| Loss of libido | 27 | 24.3 |
| Getting more difficult to achieveorgasm during sexual intercourse | 12 | 10.8 |
| Delayed ejaculation | 24 | 21.6 |
| Premature ejaculation | 8 | 7.2 |
Table 3: Pattern of sexual dysfunction
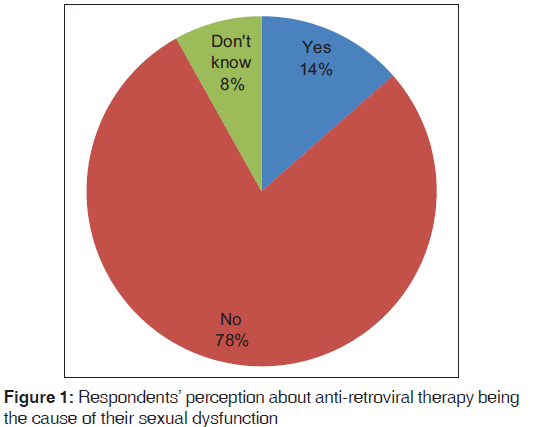
Delayed and premature ejaculations were reported among 21.6% (24/111) and 7.2% (8/111), respectively. Figure 1 showed that about 14% (33/234) of respondents said that ARVs could have caused their ED while 78% (183/234) said it should not. Table 4 showed statistically significant association (P < 0.01) between having weak erections and age above 65 years, and calculated adherence < 95%, while none exists between having weak erections and missing pills (P = 0.17).
| Variables | Weak erection | χ2 | P | |||
| Age >65 years | 4 (18.4) | 129.1 | 0.001 | |||
| Missed pills in the last 6 months | 1 (4.0) | 3.503 | 0.17 | |||
| Calculated adherence <95% | 15 | (6.6) | 17.4 | 0.001 | ||
| Duration of ART >1-year | 34 (17.4) | 2.074 | 0.15 | |||
| Binary logistic regression | ||||||
|---|---|---|---|---|---|---|
| Had weak erections | ||||||
| OR | 95% CI | P | ||||
| Lower Upper | ||||||
| Age (constant = <40) | 2.5 | 0.558 | 2.353 | 0.35 | ||
| Education level(constant = secondary and above) | 1.1 | 0.658 | 7.941 | 0.06 | ||
| Missed medications(constant = not in the last 6 months) | 4.7 | 1.140 | 1.939 | <0.001 | ||
| Self-reported adherence(constant = good) | 0.2 | 0.031 | 1.058 | 0.05 | ||
| Calculated adherence(constant = <90%) | 5.1 | 2.009 | 13.094 | <0.001 | ||
| Duration of commencement ofART (constant >15 years) | 0.3 | 0.007 | 0.109 | <0.001 | ||
Table 4: Association between weak erections and some selected socio-demographic and treatment variables on bivariate and binary logistics regression
Respondents with age >40 years are two and a half times more likely to develop ED compared to respondents with age < 40 years (P = 0.35; odds ratio [OR] =2.5; 95% confidence interval [CI] =0.56–2.35). There is no observed difference between the different education levels of respondents coming-up with weak erections (P = 0.08; OR = 1.1; 95% CI = 0.66–1.94). Respondents who have also missed their pills were about four and a half times more likely to have weak erections compared to those who have not missed their medication in the last 6 months (P = 0.01; OR = 44.7; 95% CI = 1.14–19.39). However, respondents with longer duration of being on ART (>5 years) are three times more likely to develop EDs compared to those who had been on ART for < 5 years (P < 0.01; OR = 0.3; 95% CI = 0.01–0.11). Respondents with calculated adherence level above 90% were five times more likely to have developed weak erections compared to those with poor adherence (< 90%), in which case (P < 0.01; OR = 5.1; 95% CI = 2.01–13.09). Thus, poor adherence to ART, longer duration of being on ART, missing of ART medications and older age are predictors of having EDs or weak erection on binary logistic regression analysis.
Discussion
Mean age of respondents was 37.1 (1.6) years, 207 (88.2%) were married, 175 (74.8%) had up to secondary school level education, About 80% of respondents never missed their anti-retroviral drug between the last 1-week up to 6 months preceding the study, but only 3 (1.3%) of all the respondents had optimal calculated adherence (>95%), 80% of them had their calculated adherence in the range of 90–95%. Being male has been shown to be significantly associated with non-adherence to ART.[11]
Almost half of the respondents reported having (or experiencing) various symptoms suggestive of ED. This is in congruence with previous studies.[1,12-18] A study carried out in Spain demonstrated a high prevalence of ED in HIV-infected men and also highlighted the self-perception of respondents about their body changes and mental health with all sexual function domains.[13] This study also showed that almost a quarter of the respondents that reported sexual dysfunction said they had totally lost sexual libido
The causes of sexual dysfunction vary from endocrinological, psychogenic, neurogenic, arteriogenic or iatrogenic.[18] Numerous medications are also known to cause sexual dysfunction and studies have suggested that a decrease in sexual interest and ED were found in individuals who are on HAART,[1,3,18] especially if their regimens contain Protease Inhibitors.[3,18] This study also showed that respondents who are on ART could have weak erection in spite of their adherence. Almost 20% of respondents >65 years of age were found to significantly have weak erection. Older age is one of the risk factors for ED.[1,19]
This study has demonstrated sexual dysfunctions among PLWHA. Further research may be needed to improve the description of the development of sexual dysfunctions in such individuals so as to identify pathophysiological mechanisms and to study the management/treatment of this disorder. The recovery of the sexual function, associated with a good adherence to safe sex practices, will improve the quality of life of the PLWHAs.
Findings from binary logistic regression in this study proved wrong the notion that there is no age difference among those HIV positive clients having ED and those not having it. Atrophy of old age could also explain this phenomenon. Similarly, statistical difference exists to prove any alternative hypothesis supporting that there is a difference between adherence pattern and duration of taking ART among those who developed ED compared to those not having ED. Thus, clinicians working in ART clinics should be wary of all possible implications of weak erections among clients on ART most especially those in the middle age or older age groups. It is important that clinicians take priority in ensuring that medications of those who had been on ART for long are reviewed from time to time to prevent this menace of ED among HIV-positive men.
Though this study evidently excluded drugs that may serve as cofounders, and employed oral (and some common laboratory tests) methods to exclude possible common organic causes of ED as stated, a need for further sophisticated methods of excluding remote causes may be necessary in future studies.
Conclusion
Antiretroviral are common causes of EDs among HIV-positive men on ART. Many of such men may have contemplated missing their ARV drugs or seek alternative care elsewhere when these menstrual abnormalities are getting unbearable. Stakeholders in Art care should always strive to address concerns of clients, most especially issues that may compromise ARV adherence.
References
- Asboe D, Catalan J, Mandalia S, Dedes N, Florence E, Schrooten W, et al. Sexual dysfunction in HIV-positive men is multi-factorial: A study of prevalence and associated factors. AIDS Care 2007;19:955-65.
- Hofbauer LC, Heufelder AE. Endocrine implications of human immunodeficiency virus infection. Medicine (Baltimore) 1996;75:262-78.
- Collazos J, Martínez E, Mayo J, Ibarra S. Sexual dysfunction in HIV-infected patients treated with highly active antiretroviral therapy. J Acquir Immune Defic Syndr 2002;31:322-6.
- Hijazi L, Nandwani R, Kell P. Medical management of sexual difficulties in HIV-positive individuals. Int J STD AIDS 2002;13:587-92.
- Nancy FC, Mary B, Braden H, Christopher A, April T, Carolyn B, et al. A review of hypogonadism and erectile dysfunction among HIV-infected men during the pre-and post-HAART eras: Diagnosis, pathogenesis, and management. AIDS Patient Care STDS 2005;19:655-71.
- Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry 2001;158:725-30.
- Daniell HW. Hypogonadism in men consuming sustained-action oral opioids. J Pain 2002;3:377-84.
- Trotta MP, Ammassari A, Murri R, Monforte Ad, Antinori A. Sexual dysfunction in HIV infection. Lancet 2007;369:905-6.
- Trotta MP, Ammassari A, Murri R, Marconi P, Zaccarelli M, Cozzi-Lepri A, et al. Self-reported sexual dysfunction is frequent among HIV-infected persons and is associated with suboptimal adherence to antiretrovirals. AIDS Patient Care STDS 2008;22:291-9.
- Trotta MP, Ammassari A, Cozzi-Lepri A, Zaccarelli M, Castelli F, Narciso P, et al. Adherence to highly active antiretroviral therapy is better in patients receiving non-nucleoside reverse transcriptase inhibitor-containing regimens than in those receiving protease inhibitor-containing regimens. AIDS 2003;17:1099-102.
- Lallemand F, Salhi Y, Linard F, Giami A, Rozenbaum W. Sexual dysfunction in 156 ambulatory HIV-infected men receiving highly active antiretroviral therapy combinations with and without protease inhibitors. J Acquir Immune Defic Syndr 2002;30:187-90.
- Moreno-Pérez O, Escoín C, Serna-Candel C, Picó A, Alfayate R, Merino E, et al. Risk factors for sexual and erectile dysfunction in HIV-infected men: The role of protease inhibitors. AIDS 2010;24:255-64.
- Guaraldi G, Luzi K, Murri R, Granata A, Paola MD, Orlando G, et al. Sexual dysfunction in HIV-infected men: Role of antiretroviral therapy, hypogonadism and lipodystrophy. Antivir Ther. 2007;12: 1059-65.
- Karlovsky M, Lebed B, Mydlo JH. Increasing incidence and importance of HIV/AIDS and gonorrhea among men aged >/=50 years in the US in the era of erectile dysfunction therapy. Scand J Urol Nephrol 2004;38:247-52.
- World Bank. Country Summarie: Nigeria; www.worldbank. org/en/country/Nigeria/2008.
- Okonko IO, Okerentuga PO, Akinpelu AO. Prevalence of HIV among attendees of ARFH centre in Ibadan, Southwestern Nigeria. Middle East J Sci Res 2012;11:7-12.
- Sasaki Y, Kakimoto K, Dube C, Sikazwe I, Moyo C, Syakantu G, et al. Adherence to antiretroviral therapy (ART) during the early months of treatment in rural Zambia: Influence of demographic characteristics and social surroundings of patients. Ann Clin Microbiol Antimicrob 2012;11:34.
- Schrooten W, Colebunders R, Youle M, Molenberghs G, Dedes N, Koitz G, et al. Sexual dysfunction associated with protease inhibitor containing highly active antiretroviral treatment. AIDS 2001;15:1019-23.
- Olugbenga-Bello AI, Adeoye OA, Adeomi AA, Olajide AO. Prevalence of erectile dysfunction (ED) and its risk factors among adult men in a Nigerian community. Niger Postgrad Med J 2013;20:130-5.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.