Prevalence and Predictors of Periodontal Disease among Pregnant Women in Mali, West Africa
2 Department of Dentistry Hôpital, Femmes et Enfants Koutiala, Mali, West Africa, Email: carol12@gmail.com
Citation: Rosanna F Hess. Prevalence and Predictors of Periodontal Disease among Pregnant Women in Mali, West Africa. Ann Med Health Sci Res. 2017; 7: 263-270
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Epidemiologic reports on dental or oral health in Mali West Africa are rare. The prevalence of periodontal disease (PD) has not been well established among pregnant women in this sub-Saharan nation. Aim: The purpose of this study was three-fold: to describe oral health self-care behaviors; to measure the prevalence of PD; and to determine predictors of PD among pregnant women in southeastern Mali. Methods and Subjects: In this cross-sectional, correlational study, the Ramfjord Periodontal Index (PDI) and the Community Periodontal Index (CPI) were used to assess levels of PD. Seventy-four pregnant women were surveyed for oral self-care behaviors and examined for PD. Results: Almost all women said they brushed their teeth daily. Years of schooling was a statistically significant predictor of brushing frequency (P=0.005). 81% of the women had never had a professional dental exam. Based on the PDI, 24% were diagnosed with gingivitis and 49% with periodontitis. According to the CPI, 47% had pathological pockets in the periodontium. A history of previous oral/dental problems was a predictor of the severity of periodontal disease (P <.001). Conclusion: The presence of periodontal disease among this sample of Malian women was high; oral hygiene behaviors and use of dental professionals were low. Screening for PD should be included as a routine part of antenatal care. Research is needed in Mali to determine if PD is a risk factor for adverse pregnancy outcomes.
Keywords
Oral hygiene; Periodontal diseases; Pregnant women; Prevalence; Mali; Africa
Introduction
Periodontal disease (PD), which includes gingivitis, an inflammation of the gums, and periodontitis, a more serious inflammation with breakdown of teeth’s supporting tissues[1] may elevate the risk of serious health problems for child bearing women.[2,3] Diseased periodontal tissues may serve as reservoirs of bacteria and these bacteria may move across the placental barrier to the unborn fetus.[4] Preterm birth[5] low birth weight newborns[6-9] increased time to conception[10] and premature rupture of membranes[11] have been attributed to the presence of PD in pregnant women.
Oral health inequities exist in many parts of the world, particularly in low resource countries.[12-14] Research on dental and or oral health in Africa is relatively rare due to low prioritization.[15] Mali, a country of almost 17 million people, faces some of the most challenging health issues in the world; life expectancy at 55 years, maternal mortality at 540/100,000 births, infant mortality at 104/1,000 live births, and female literacy rate at 25%, to name a few.[16] The country lacks national systems to deal with non-communicable diseases such as periodontal disease.[17] Mali is one of 47 countries in the African Region which carries a particular burden of risk factors for poor oral health.[18] The prevalence of gingivitis and periodontitis has not been well established among pregnant women in this sub- Saharan nation. The purpose of this study was three-fold: to describe oral self-care behaviors; to measure the prevalence of PD, and to determine predictors related to PD among pregnant women in southeastern Mali.
Materials and Methods
This was a cross-sectional, correlational study. Ethical approval in Mali where the study was conducted and by the Human Research Committee of Malone University, Canton, Ohio, USA. Data was collected in 2013-2014 in Mali at a non-governmental hospital in a city of approximately 140,000 inhabitants. Over 2500 women attend pre-natal clinics and give birth at the study site hospital each year.
Sampling
Participants were enrolled in the study by convenience sampling. (Sample size calculation is reported below in paragraph on data analysis.) Inclusion criteria were pregnant, in first or second trimester of pregnancy, Malian, attending prenatal clinic at study site hospital. Exclusion criteria were women who were not pregnant, not Malian, and not attending prenatal clinic at the study site hospital. A Malian dental assistant (third author) who worked in hospital’s dental department recruited women over a period of six months. The recruiter announced the study each morning to groups of women waiting for their antenatal appointment. When an individual woman had checked in for her antenatal consultation, the recruiter introduced herself and then used a prepared script to explain the study’s purpose, procedures, and consent form. The woman was assured during the consenting process that the study was voluntary and refusal to take part would in no way affect her prenatal care or other services she received at the hospital. If the woman agreed to participate in the study, she signed a consent form.
Using a questionnaire developed by the research team, the recruiter then asked the participant questions about her age, years of schooling, parity, plus general health and history of oral or dental problems (yes/no). After her antenatal visit was completed the woman was to go to the dental department for the oral exam. There she also answered questions about frequency of brushing, objects used to clean teeth and gums, and her history of professional dental care (yes/no). Data was also collected from the woman’s clinic chart. This included results of blood tests and obstetric history. The information for each woman was written on an individual survey sheet and later transferred to an Excel file.
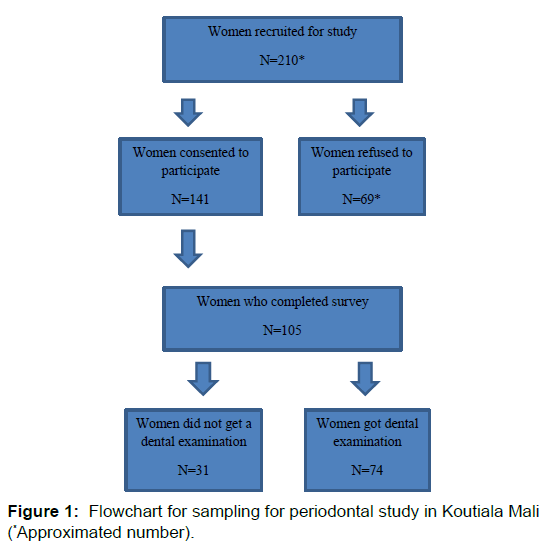
Recruitment for this study was challenging. Figure 1 represents a sampling flowchart. Approximately 50% of the women (exact number is unknown) approached by the recruiter declined the invitation to take part in the study. Their reasons for refusal included fear of dental work, insufficient time to stay that day to have the oral exam, and lack of husband’s knowledge of the study and his consent.
Oral exam indexes and scoring
Women were scored using two indexes. The Ramfjord Periodontal Disease Index (PDI)[19] was used to assess prevalence and severity of gingivitis and periodontitis. This index has three components.
The gingival/periodontal portion is scored as a unit:
0=Normal
1-2-3=Gingivitis
4-5-6=Periodontitis
The plaque component is scored as one unit:
0=No plaque,
1=Plaque exists on some but not on all of the interproximal, buccal, and lingual surfaces of each tooth
2=Plaque found on all interproximal, buccal, and lingual surfaces, but on less than one half of these surfaces
3=Plaque covering more than one half of all interproximal, buccal and lingual surfaces.
On the calculus portion of the index only lingual and facial are assessed:
0=No calculus
1=Supragingival calculus covering not more than 1 mm below the free gingival margin
2=Moderate amounts of supragingival and sub gingival calculus or only sub gingival calculus
3=Abundance of sub gingival and supra gingival calculus.
Each component may be scored separately. Higher scores indicated greater severity of PD. The Community Periodontal Index (CPI) [20] was used to screen for the presence of gingival bleeding, calculus, and pathological pockets in the periodontium.[21]
The CPI scoring criteria was:
0=No periodontal disease
1=Bleeding observed after probing
2=Calculus with plaque seen or felt by probing
3=Shallow (4-5 mm) pathological pocket
4=Deep (6 mm or more) pathological pocket.
A single item was used to measure general health status, with the response choices of excellent (3), good (2), and poor (1). Each woman reported her own general health status. A recent hematocrit was retrieved from each woman’s prenatal record. A woman was classified as anemic if she had a hematocrit of less than or equal to 33%.[22]
Clinical examination
The Malian dental technician examined each woman in the study site hospital’s dental clinic which is equipped with two standard reclining dental chairs and ceiling-mounted dental lights. To score the PDI the technician performed an oral exam with a plane-faced dental mirror and a blunt periodontal assessment probe on six teeth, numbers 12, 16, 24, 32, 36 and 44 (Federation Dentaire International Système de Numeration) and on the buccal, interproximal, and lingual surfaces of the tooth.
The dental hygienist (2nd author) recorded the technician’s findings on the study’s case report form and in the patient’s chart. The hygienist then re-examined the patient using a periodontal probe to verify the technician’s findings and score the CPI. If a woman received a PDI score of 3 or greater, or a CPI score of 3 or greater, she was treated immediately, at no cost to the patient. The treatment included prophylactic antibiotics, dental cleaning and root planning. The participant also received instructions on oral hygiene and proper brushing technique. She was required to demonstrate this technique before leaving the dental department. Each woman was also given a toothbrush and dental floss along with a phone card worth the equivalent of $10US.
Statistical analysis
Data analysis was computed using IBM Statistical Package for Social Sciences Version 22®. Data are presented as descriptive statistics (frequencies and means) and inferential statistics (t-tests, ANOVA, and Chi-square test). We hypothesized that higher brushing frequency would result in lower PDI and CPI scores. Statistical significance was set at P<0.05. Two separate simultaneous multiple regression analyses were conducted to determine predictors of brushing frequency and predictors of PD. Power analysis was performed to estimate a minimum sample size for multiple regression analyses;[23] 5 predictors, an effect size of 0.15, an alpha of 0.05, and a power of 0.80, yielded a sample size of 79 for the predictor model for brushing frequency; 6 predictors, a medium effect size of 0.15, an alpha of 0.05, and a power of 0.80 yielded a sample size of 84 for the predictor model for severity of periodontal disease. One hundred and five pregnant Malian women completed the survey questions. Of those, thirty one women did not have the oral exam. Data analysis was conducted on the remaining 74 women.
Results
Description of sample
In this sample of 74 pregnant women, the mean age was 25 (6.03), with a range of 16-38 years. The mean years of schooling was 3.9 (4.65); almost 50% (32/74) of the sample had no formal education. Gravida ranged from 1 to 11 pregnancies with a mean of 3.0 (2.18); 60% (44/74) of the sample was multiparous. Years of schooling and gravida were inversely correlated (Pearson r=- 0.358; P=0.003). Sixty four women (87.7%) self-reported good health. Hematocrit levels ranged from 16 to 39%; over 75% of the participants were anemic at enrolment [Table 1].
| Variables | N (%)* |
|---|---|
| Age Range 16-38 Mean (SD) 25.2 (6.03) 16-23 24-31 32-38 |
33 (44.6) 30 (40.5) 11 (14.9) |
| Years of Schooling Range 0-17 Mean (SD) 3.9 (4.65) 0 years of schooling 1-6 years of schooling 7+ years of schooling |
32 (46.4) 18 (26.1) 19 (27.5) |
| General Health (self-report) Excellent Good Poor |
1 (1.4) 64 (87.7) 8 (11.0) |
| Gravida Range 1 - 11 Mean (SD) 3.0 (2.18) Primiparous Multiparous 2 - 4 pregnancies Grand multipara 5 - 11 pregnancies |
20 (27.4) 44 (60.3) 9 (12.3) |
| Enrolment Hematocrit Range 16-39% Mean (SD) 31.96 (4.95) 16-33 (considered anemic) 33 > (considered not anemic) |
35 (76.1) 11 (23.9) |
*If not equal n=74, due to missing data
Table 1: Description of sample: Demographic frequencies (n=74).
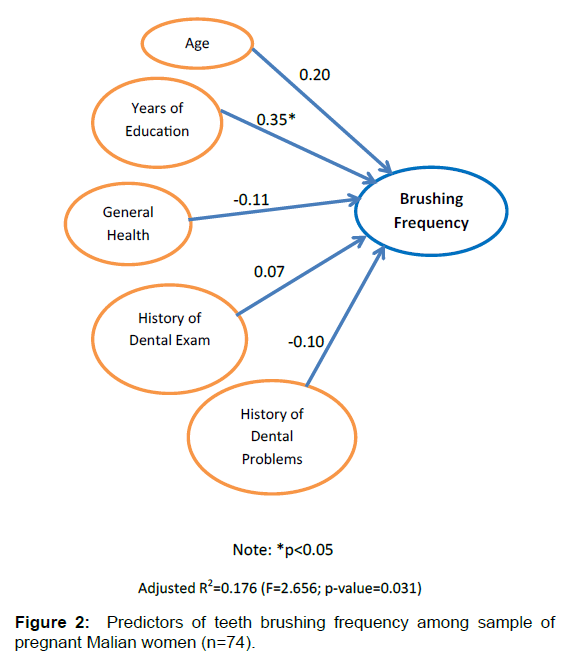
Oral self-care
99% indicated they brushed their teeth at least once a day or more. Almost 80% of the women indicated they used toothpaste and a toothbrush to clean their teeth. Years of education and frequency of tooth brushing were significantly correlated (Pearson r=0.316; P=0.008). 81% said they had never had a dental or oral exam performed by a dental professional. Older women (over the age of 32 years) were less likely to have had an exam done by a dental professional (P=0.129). Ninety one percent of those who had no formal schooling had never been to a dental professional. 62.2% (46/74) of the women indicated that they had previously experienced oral or dental problems but only 10 said they had gone to a professional dentist for care [Table 2]. The regression analysis revealed that years of education was a statistically significant predictor of brushing frequency (t=2.880; P=0.005) despite a sample size smaller than the one calculated for the regression analysis. Age, history of a professional dental exam, general health status, and history of periodontal problems were not significant predictors. This model was statistically significant (F=2.656; P=0.031) and explained 17.6% of the variance, indicating there are other factors that predict brushing frequency [Figure 2].
| Variables | N (%) |
|---|---|
| Number of times brushed teeth each day One time or less per day 2 or more times per day |
33 (44.6) 41 (55.4) |
| Used to clean teeth and gums* Tooth paste and brush Wooden stick Both stick and brush Other (wooden stick with brush) |
56 (76.7) 4 (5.5) 1 (1.4) 12 (16.4) |
| History of professional dental exam? Yes No |
14 (18.9) 60 (81.1) |
| History of oral/dental problems** Yes No |
46 (62.2) 28 (37.8) |
* If not equal n=74, due to missing data
Table 2: Frequencies of self-reported oral care (n= 74).
Prevalence of periodontal disease
Scores on the PDI ranged from 0-6 with a mean of 2.58 (1.8). Scores on the CPI ranged from 0-4 with a mean of 2.00 (1.5). A strong, positive, statistically significant correlation exists between the PDI and the CPI scores (Pearson r=0.94; P<0.001). Based on the PDI, 73% of the women had PD; 24% were diagnosed with gingivitis and 48.6% with periodontitis. 42% (31/74) of these pregnant women had 50% or more of all the surfaces of their teeth covered in plaque. Almost 50% (36/74) had an abundance of supra and subgingival calculus. Based on the CPI score, 47% had pathological pockets in their gums [Table 3].
| Variables | N (%) |
|---|---|
| Ramfjord Periodontal Disease Index Frequencies: Gingival and Periodontal Component: Normal Gingivitis Periodontitis Plaque component No plaque Plaque – not on all surfaces Plaque on all surfaces <50% Plaque on all surfaces >50% Calculus component Absence of calculus Supra-gingival calculus <1mm Moderate amount supra and subgingival calculus or subgingival calculus only Abundance of supra and subgingival calculus |
20 (27.0) 18 (24.3) 36 (48.6) 1 (1.4) 25 (33.8) 17 (23.0) 31 (41.9) 2 (2.7) 21 (28.4) 15 (20.3) 36 (48.6) |
| Community Periodontal Index CPI Frequencies No periodontal disease Bleeding on probing Calculus with plaque Pathological pocket 4-5 mm Pathological pocket >6 mm |
24 (32.4) 0 (0)* 15 (20.3) 22 (29.7) 13 (17.6) |
* Bleeding occurs when there is inflammation, presence of calculus, and pathological pockets. There were no women (0%) who had only bleeding during probing.
Table 3: Frequencies of periodontal status evaluated by the PDI and the CPI (n=74).
Further analysis of demographic characteristics, oral self-care behaviors, the PDI, and the CPI was conducted to compare means on several variables [Table 4]. Age was not significantly correlated to the PDI score (P=0.44) or the CPI score (P=0.30). Based on the PDI, women in the oldest age group (32-38 years) had the highest PDI and CPI scores. Well over two-thirds of the women in each age group needed professional plaque removal and deep scaling / root planing. Years of schooling and the PDI score (P=0.05) showed a significant relationship but this was not the case for the CPI (P=0.107). Women with zero years of schooling had higher PDI and CPI means than women with any number of years of schooling.
| Variable | PDI Score Mean* (SD) | P value | CPI Gingival Periodontal Component Mean* (SD) |
P value |
|---|---|---|---|---|
| Age 16-23 24-31 32-28 |
2.58 (1.89) 2.60 (1.94) 2.73 (1.85) |
0.97 |
1.94 (1.41) 2.03 (1.61) 2.09 (1.75) |
0.95 |
| Years of Schooling 0 years 1-6 years 7+ years |
3.22 (1.72) 2.72 (1.96) 2.16 (1.67) |
0.12 |
2.47 (1.39) 2.00 (1.57) 1.74 (1.53) |
0.21 |
| Gravida Primiparous 1-4 pregnancies 6-10 pregnancies |
2.30 (1.75) 2.73 (1.99) 2.56 (1.74) |
0.75 |
1.85 (1.35) 2.07 (1.63) 1.89 (1.54) |
0.85 |
| General Health status Poor Good Excellent |
3.88 (0.35) 2.42 (1.95) 4.00 (0.00) |
0.09 |
3.25 (0.71) 1.83 (1.55) 3.00 (0.00) |
0.04* |
| Hematocrit < 34% (anemic) >33% (not anemic) |
2.34 (1.75) 2.82 (1.89) |
0.44 |
1.69 (1.43) 2.18 (1.47) |
0.32 |
| Times brush teeth/day Once Two or more |
2.91 (1.86) 2.37 (1.85) |
0.22 |
2.24 (1.46) 1.80 (1.57) |
0.22 |
| History of dental visits Yes No |
2.29 (1.98) 2.68 (1.86) |
0.51 |
1.98 (1.48) 2.07 (1.53) |
0.85 |
| History of oral /dental problems Yes No |
3.96 (0.70) 0.39 (0.74) |
< 0.01* |
3.04 0.29 |
< 0.01* |
* T-tests and ANOVAs were used to measure differences of means
Table 4: Mean scores (SD) on PDI and CPI for several variables.
Gravida was not significantly correlated to the PDI score (P=0.43) or the CPI score (P=0.42). Multiparous women (1-4 pregnancies) had the highest PDI and CPI scores. Women selfreported their overall health status as poor, good, and excellent. Differences of means per level of health on the CPI were statistically significant (P=0.04); women who reported good health had the lowest mean. Women who self-reported with poor health (n=8) had the highest means on the PDI and the CPI.
The hematocrit (HCT) levels in this sample of pregnant women ranged from 16 to 39%, with a mean of 31.96% (4.95) The correlations between HCT and PDI and HCT and CPI scores were not statistically significant (P=0.74; 0.77 respectively). Women who were not anemic women had a higher percentage of deep periodontal pockets than women who were anemic (63.6% and 34.3% respectively).
Analysis revealed that women who brushed their teeth once a day had higher levels of gingivitis and periodontitis than those who brushed at least twice a day (76.7% and 68.3% respectively). Those who brushed only once a day had more plaque buildup and a higher percentage of deep pathological pockets. But the hypothesis that frequency of brushing each day would result in lower index scores was not statistically supported (P=0.22; 0.29 respectively on the PDI and the CPI). Eighty-one percent of the participants (60/74) never had a professional dental exam; and 75% of those women (45/60) had gingivitis or periodontitis. Women who had been to a dental office had a slightly lower combined percentage of shallow and deep pathological pockets (42.8%) than those who had never visited one (48.3%). Differences of means on the PDI and CPI were not statistically significant when comparing women with or without a history of professional dental care (P=0.48 and 0.85 respectively). Sixtytwo percent (42/74) of the women who received an oral screening in this study reported that they had previously suffered from oral and or dental problems. Differences of means between women with self-reported history of PD were statistically significant (P<0.001) on the PDI and the CPI.
A simultaneous multiple regression analysis was conducted to determine predictors of PD as measured by the Ramfjord PDI. Age, years of schooling, general health status, brushing frequency, previous professional dental exam, and previous oral/dental problems were regressed on the PDI score. This model was statistically significant (F=68.993; P<0.001), explaining 85.9% of the variance. Despite a sample size smaller than the one calculated for the regression analysis, a statistically significant predictor of the severity of PD was found; history of previous oral/dental problems was a significant predictor of the severity of PD (t=19.298; P<0.001) [Table 5].
| Variables | B | Std. Error | Beta | t | P-value |
|---|---|---|---|---|---|
| Age | 0.015 | 0.02 | 0.049 | 1.005 | 0.319 |
| Years of schooling | 0.002 | 0.02 | 0.006 | 0.109 | 0.913 |
| History of periodontal problems | 3.591 | 0.19 | 0.931 | 19.298 | .000* |
| History of professional dental exam | 0.02 | 0.24 | 0.004 | 0.085 | 0.932 |
| Brushing frequency | -0.06 | 0.13 | -0.02 | -0.458 | 0.649 |
| General health status | 0.118 | 0.25 | 0.023 | 0.471 | 0.639 |
*Statistically significant p<0.05
Table 5: Matrix of predictors of severity of periodontal disease in pregnant Malian women (n=74) using simultaneous multiple regression analysis.
Discussion
The objectives of this study were to assess oral self-care among pregnant women and establish a prevalence of PD while determining predictors of PD. Results of analysis produced several important findings. One major finding was that 81% of these pregnant Malian women had never had a professional dental exam. Another major finding was that 73% (54/74) of the women had PD based on the PDI and 47% had either shallow or deep periodontal pockets in their gums according to the CPI. This PD prevalence rate among pregnant Malian women is higher than the 33% found among pregnant women in Lagos Nigeria [24] but comparable to the 67% found in Uganda.[9] Of note is that the Nigerian and Ugandan women were more highly educated than the Malians.
Age, years of schooling, gravida, history of professional dental exam, brushing frequency, and hematocrit level were not statistically associated with PD in this study. A small sample size may have precluded finding statistical significance. The fact that older Malian women had higher levels and more severe periodontitis is similar to women in Nigeria.[25] An increased prevalence of periodontitis among older women may be due to the consequences of years of untreated disease or to the natural loss of periodontal tissue.[26]
The high prevalence of PD among Malian women with fewer years of schooling is another important finding. This is consistent with findings in other studies where lower PD severity was related to higher education levels.[25-27] Women in Mali have a low functional literacy rate (25%).[28] Low functional and health literacy levels are related to poorer health outcomes and less access to health services.[29,30] Since oral diseases are socially determined,[13,31] people with a higher education are more likely to have more opportunities to learn about oral hygiene and, if equated with a higher economic status, are more able to afford preventative and curative dental care.[32]
Results revealed that more frequent brushing did not improve PDI or CPI scores. This may be due to faulty brushing techniques and the duration of brushing, rather than the number of times per day a woman brushed her teeth.[33] Dental staff should instruct patients on proper technique and duration at each dental visit and seek opportunities outside the dental clinic to promote oral and dental self-care. Since women with fewer years of education brushed less frequently than women with more schooling, oral health promotion outreaches should be conducted in settings where poorly educated women can be reached.
In this study, women who had previously received professional dental care had slightly better scores on the CPI and the PDI than those who had not, but even among these women the prevalence of PD was high. The percentage of Malian pregnant women who had not previously had a professional dental exam (81%) is higher than among Nigerian pregnant women (63%) where previous dental exams were significantly related to education level.[24] Previous dental exams and years of schooling were not significantly correlated in this Mali study.
Seventy-six percent (35/74) of the women in this study were anemic early in their pregnancy compared to 68% of pregnant women in Benin.[34] Chronic periodontitis may be a cause of anemia in the general population.[35] Pregnant women may be anemic for a variety of reasons: hemodynamic changes, iron deficiency, poor nutrition, parasitic infections such as malaria and helminth infestations, and chronic diseases including chronic periodontitis. Periodontitis and anemia were independent predictors of low birth weight infants in a study in Pakistan.[36] Curiously among the Malian women it was the non-anemic ones who had the highest PD score on the CPI. This finding is the reverse of results found among pregnant women in India where severest PD levels were associated with lower hemoglobin levels.[37] Further research, with a larger sample size, is needed to clarify these Malian findings.
Recommendations
Almost three-quarters of the screened pregnant Malian women had such severe PD that their teeth were immediately cleaned by the dental staff who then recommended professional followup dental care and further treatment. High PD levels even among women who said they brushed more frequently may indicate that brushing techniques are incorrect or that brushes and or toothpaste are of poor quality. A focus on oral health is needed at the primary health care level.[18] As a part of antenatal education, dental and nursing staff could teach pregnant women, particularly those with few years of schooling, the importance of oral hygiene and proper brushing techniques. Midwives, nurses, and obstetricians should strongly recommend a periodontal exam to all pregnant women as part of routine antepartum care.[13,31,38]
Numerous studies have linked PD to adverse pregnancy outcomes, particularly pre-term births and pre-eclampsia [7]. Now that we know that the prevalence of PD in some pregnant women in Mali is high, research is needed to determine if its severity is a risk factor related to the high rate of preterm births and low birth weight babies in this country.[39]
Though identifying them was not a purpose of this study, barriers to dental care in this region of Mali became evident, particularly during the recruitment and examination processes. Lack of knowledge of the benefits of oral / dental care, fear of the examination itself, financial constraints, poor access to dental facilities, and cultural dynamics such as the need for spousal permission to seek health care are all contributing factors to the lack of oral/dental care among Malian women. These barriers undoubtedly contribute to the low rate of oral self-care and the high prevalence of PD in this population. Studies are needed to determine barriers to the utilization of dental services in this and the wider Malian population and to determine successful strategies to overcome these barriers. Dental health must be made a health care priority at the national, local, and community level to see improvements in levels of PD.
Limitations
This study, maybe the first of its kind, indicates a high prevalence of PD among these pregnant Malian women. But convenience sampling, the use of one recruitment site, a high rate of refusal to participate, and an elevated rate of attrition among enrolled participants, makes it impossible to generalize these findings to all pregnant women in Mali. Convenience sampling may have led to sampling bias. Pregnant women attending antenatal clinics elsewhere or not at all may have different levels of education and more or less access to dental care facilities leading to different PD prevalence rates. Women living in urban areas versus semi-urban or rural regions, and with a different socio-economic status (e.g. income level, type of employment) were not measured in this study. These variables should be included in future studies in Mali particularly because poverty is an important factor contributing to ill health in general and to oral/dental health in particular.[18,31] Convenience sampling may have led to an over-representation of primiparous women. There were a much higher percentage of primiparous women compared to multiparous women in this sample. This is probably because fewer multiparous women in the study site region attend antenatal clinic. More research is needed to overcome these limitations.
Conclusion
Periodontal disease among this sample of pregnant Malian women is high; oral hygiene behaviors and use of dental professionals is low. Attendance at an antenatal clinic indicates that women are interested in good health for themselves and their unborn children. To improve general well-being, and to potentially reduce the risk of adverse pregnancy outcomes, oral hygiene should be taught to all pregnant women during the antepartum period and these women should be offered a periodontal exam as a part of antenatal care.
Acknowledgements
We appreciate the Malian women who agreed to be a part of this research study as well as members of the staff at the Hôpital Femmes et Enfants, Koutiala Mali, who encouraged this project. We also acknowledge with sincere thanks Ratchneewan Ross, PhD, RN, Cone Health Endowed Professor, UNC Greenboro, NC, for her help in study design, statistical analysis, and manuscript critique, and Dr. Jeffrey Amstutz, DDS and Mrs. Darla Lyons, RDH for reading and critiquing this manuscript.
Conflict of Interest
All authors declare no conflict of interest.
REFERENCES
- Periodontal Disease Fact Sheet. American Academy of Periodontology. 2017;https://www.perio.org/newsroom/periodontal-disease-fact-sheet
- Anil S, Alrowis RM, Chalisserry EP, Chalissery VP, Al-Moharib HS, Al-Sulaimani AF. Oral health and adverse pregnancy outcomes. Emerging Trends in Oral Health Sciences and Dentistry. INTECH (intechopen.com) 2015; 631-662.
- Keshava A, Chidambar YS, Zope S, Naduwinmani S, Preetham J. Periodontitis as a risk factor for preterm low birth weight infants: A clinico-epidemiological evaluation. J Basic Clin Repro Sci 2014;3:88-92.
- Zi MY, Longo PL, Bueno-Silva B, Mayer MP. Mechanisms involved in the association between periodontitis and complications in pregnancy. Front Public Health 2015;2:290.
- Muwazi L, Rwenyonyi CM, Nkamba M, Kutesa A, Kagawa M, Mugyenyi G, et al. Periodontal conditions, low birth weight and preterm birth among postpartum mothers in two tertiary health facilities in Uganda. BMC Oral Health 2014;14:1.
- Cisse DM, Diouf AF, Diadhiou MF, Tal-Dia A. Periodontal disease of pregnant women and low weight newborn in Senegal: A case-control study. Open J Epidem 2015;5:1.
- Ide M, Papapanou PN. 2013. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes– A systematic review. J Clin Periodontol 2013;40:s14.
- Walia M, Saini N. Relationship between periodontal diseases and preterm birth: Recent epidemiological and biological data. Int J Appl Basic Med Res 2015;5:2.
- Wandera M, Astrøm AN, Okullo I, Tumwine JK. Determinants of periodontal health in pregnant women and association with infants' anthropometric status: A prospective cohort study from Eastern Uganda. BMC Pregnancy Childbirth 2012;12:1.
- Nwhator SO, Opeodu OI, Ayanbadejo PO, Umeizudike KA, Olamijulo JA, Alade GO, et al. Could periodontitis affect time to conception? Ann Med Health Sci Res 2014;4:817-822.
- Stadelmann PFM, Eick S, Salvi GE, Surbek D, Mohr S, Bürgin W, et al. Increased periodontal inflammation in women with preterm premature rupture of membranes. Clin Oral Investig 2015;19:1537-1546.
- Petersen PE, Ogawa H. The global burden of periodontal disease: Towards integration with chronic disease and dental control. Periodontol 2000 2012;60:15-39.
- Sgan-Cohen HD, Evans RW, Whelton H, Villena RS, MacDougall M, Williams DM. IADR-GOHIRA® Steering and Task Groups. IADR global oral health inequalities research agenda (IADR-GOHIRA®): A call to action. J Dent Res 2013;92:209-211
- Williams DM, Sheiham A, Honkala E. Addressing oral health inequalities in the Africa and Middle East Region. J Dent Res 2015;94;875-877.
- Naidoo S, Dimba E, Yengopal V, Folayan MO, Akpata ES. Strategies for oral health research in Africa and the Middle Eastern Region. Adv Dent Res 2015;27:43-49.
- Countries of the world. Mali People 2016;http://www.theodora.com/wfbcurrent/mali/mali_people.html
- Mali. Noncommunicable diseases (NCD) country profiles, World Health Organization 2014;http://www.who.int/nmh/countries/mli_en.pdf?ua=1
- World Health Organization. Promoting oral health in Africa: Prevention and control of oral diseases and noma as part of essential noncommunicable disease interventions. (2016).http://www.who.int/iris/handle/10665/205886
- Ramfjord SP. The Periodontal Disease Index. J Periodontol 1967;38:602-610.
- Ainamo J, Barmes D, Beagric G, Cutress T, Martin J, Sardo‑Infirri J. Development of the WHO Community Periodontal Index of Treatment Needs (CPITN). Int Dent J 1982;32:281‑291.
- Cutress TW, Ainamo J, Sardo-Infirri J. The Community Periodontal Index of Treatment Needs (CPITN) procedure for population groups and individuals. Int Dent J 1987;37:222-233.
- Gaillard R, Eilers PH, Yassine M, Hofman A, Steegers EA, Jaddoe VW. Risk factors and consequences of maternal anaemia and elevated haemoglobin levels during pregnancy: A population based prospective cohort study. Paediatr Perinatal Epidemiol 2014;28:213-226.
- Polit DE, Beck CT. Nursing research: Generating and assessing evidence for nursing practice. (9th edition), 2012. Philadelphia, Wolters Kluwer / Lippincott Williams & Wilkins, USA.
- Soroye M, Ayanbadejo P, Savage K, Oluwole A. Association between periodontal disease and pregnancy outcomes. Odontostomatol Trop 2015;38:5-16.
- Onigbinde OO, Sorunke ME, Braimoh MO, Adeniyi AO. Periodontol status and some variables among pregnant women in a Nigeria tertiary institution. Ann Med Health Sci Res 2014;4:852-857.
- Piscoya MDBDV, Ximenes RADA, Silva GMD, Jamelli SR, Coutinho SB. Periodontitis-associated risk factors in pregnant women. Clinics 2012;67:27-33.
- Azofeifa A, Yeung LF, Alverson CJ, Beltrán-Aguilar E. Oral health conditions and dental visits among pregnant women and nonpregnant women of childbearing age in the United States, National Health and Nutrition Examination Survey, 1999-2004. Prev Chronic Dis 2014;11:140212.
- The World Factbook. Africa: Mali. https://www.cia.gov/library/publications/the-world-factbook/geos/ml.html
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97-107.
- Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes. A review of the literature. J Gen Intern Med 2004;19:1228-1239.
- Chidzonga MM, Carneiro LC, Kalyanyama BM, Kwamin F, Oginni FO. Determinants of oral diseases in the African and Middle East Regions. Adv Dent Res 2015;27:26-31.
- Ogunbodede EO, Kida IA, Madjapa HS, Amedari M, Ehizele A, Mutave R, et al. Oral health inequalities between rural and urban populations of the African and Middle East Region. Adv Dent Res 2015;27:18-25.
- Ganss C, Schlueter N, Preiss S, Klimek J. Tooth brushing habits in uninstructed adults—frequency, technique, duration and force. Clin Oral Invest 2009;13:203-208.
- Ouédraogo S, Koura GK, Bodeau-Livinec F, Accrombessi MM, Massougbodji A, Cot M. Maternal anemia in pregnancy: Assessing the effect of routine preventive measures in a malaria-endemic area. Amer J Trop Med Hygiene 2013;88:292-300.
- Shetty MK, Thomas B, Shetty AV. Comparative evaluation of hemoglobin level in anemic patients with chronic periodontitis before and after treatment. J Interdiscip Dent 2014;4:24.
- Khan NS, Ashraf RN, Noor S, Rahman M, Mashhadi SF, Rashid Z, et al. Association of maternal periodontitis with low birth weight in newborns in a tertiary care hospital. J Ayub Med Coll Abbottabad 2016;28:120-125.
- Kothiwale SV, Desai BR, Kothiwale VA, Gandhi M, Konin S. Periodontal disease as a potential risk factor for low birth weight and reduced maternal haemoglobin levels. Oral Health Prev Dent 2014;1:83-90.
- Trivedi S, Lal N, Singhal R. Periodontal diseases and pregnancy. J Orofacial Sci 2015;7:67.
- Mali S. Profile of preterm and low birth weight prevention and care. Every Preemie Scale no date.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.