Prevalence of Depression among Elderly Women in India: An Intersectional Analysis of the Longitudinal Ageing Study in India (LASI), 2017-2018
2 Department of Public Health, AIPH University, Bhubaneswar, Odisha, India, Email: parampanda55@gmail.com
3 Department of Public Health, State Maternal and EMTCT Consultant in UNICEF, Odisha, India
Received: 29-Mar-2023, Manuscript No. amhsr-23-93421; Editor assigned: 31-Mar-2023, Pre QC No. amhsr-23-93421 (PQ); Reviewed: 17-Apr-2023 QC No. amhsr-23-93421; Revised: 24-Apr-2023, Manuscript No. amhsr-23-93421 (R); Published: 02-May-2023
Citation: Panda P, et al. Prevalence of Depression among Elderly Women in India-An Intersectional Analysis of the Longitudinal Ageing Study in India (LASI), 2017-2018. Ann Med Health Sci Res. 2023;13:543-553
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Epidemiological transition in India shows a shift in disease burden from youth to the elderly. As Life Expectancy increases, a greater burden is placed on the state, society, and families in India. Mental health disorders are insidious, debilitating Non Communicable Diseases (NCDs) that afflict people, their families, and generations down the line. Globally, depression is the leading cause of mental health-related disability. It is estimated that mental illness contributes to 4.7% of Disability Adjusted Life Years (DALYs) in India. It is predicted that by 2026, the elderly's sex ratio will increase to 1,060 feminizing ageing. Research has shown that elderly women in developed countries like the United States are more prone to depression. Chronic morbidities are more common in women than in men, and they may suffer from poor vision, depression, impaired physical performance, and elder abuse. Mostly widowed, economically dependent, lacking proper food and clothing, fearing the future, and lacking proper care, they have difficulty coping with these health problems. There are surprisingly few studies on elderly female depression. Therefore we want to hypothesize the prevalence of depression among women in different regions and demographic groups in India, and what factors may contribute to these differences. Using intersectional analysis with the data from Wave 1 (2017-2018) of the (Longitudinal Ageing Study in India) LASI (N=16,737) we were able to explore the intersecting patterns between different variables and how people are positioned simultaneously and position themselves in different multiple categories based on the type of place of residence, age and level of education. Through the study we further aim to determine the prevalence of depression among elderly female in the age group of 60 in different states using the Chloropleth map. The findings of the study highlight the significance of the place of residence in the development of depression among elderly women, with the rural area being associated with a higher prevalence of depression compared to urban area. When compared to people with higher literacy, those with low literacy were significantly associated with depression. State-wise, there is a huge difference between the prevalence of elderly women depression in rural and urban areas. The study highlights the vulnerability of elderly women to depression. It is possible for the government to develop programs that address the needs of elderly women, both in urban and rural areas, to reduce depression. Multi-factor approaches to mental health, which consider age, literacy, and location, are essential. Programs targeting specific populations can be developed to address depression's root causes.
Keywords
Epidemiological transition; Mental health disorders; Non-Communicable Diseases (NCDs); depression; Disability Adjusted Life Years (DALYs); Elderly women; Prevalence
Introduction
People and their families, and generations down the line, suffer greatly from mental health disorders, an insidious, often debilitating form of Non Communicable Diseases (NCDs) [1]. The greatest mental health-related burden is attributed to depression, which is a leading cause of disability worldwide [2]. Mental health impairment worsens a number of NCDs risk factors, such as poor lifestyle choices resulting in obesity, inactivity, and tobacco abuse, poor health literacy, and a lack of access to health promotion activities [3–5]. As per the WHO Global Burden of Disease Report globally, 4.4% of the population is estimated to be depressed in 2015 [6]. The report also says that around the world, 322 million people are suffering from depression [7]. There is a higher incidence of depression among females (5.1%) than among males (3.6%). It is estimated that this number is growing each year. Even though women live longer than men, research shows they are more prone to certain diseases, which can ultimately shorten their lifespan [8]. Strokes, depression, Alzheimer's, and autoimmune diseases such as multiple sclerosis and rheumatoid arthritis are among them. Most of these people live in the South-East Asia Region and the Western Pacific Region, due to the fact that these regions have much larger populations than the others (which include India and China, for example) [9–15]. According to estimates from 2015, the number of Years Lived with Disability (YLD) related to depression amounted to more than 50 million around the world [7]. In terms of the prevalence of non-fatal health loss, depression disorders are ranked as one of the most significant contributors (7.5% of all YLD) [6].
As per the WHO report for low-and middle-income countries, depression poses a significant public health challenge due to its comorbidity with chronic physical disease [16]. It is estimated that depression has a 2-4 fold higher prevalence in patients with chronic diseases such as cancer, diabetes mellitus, stroke, or cardiovascular disease, and the disease may last longer [16]. Mental disorders such as depression and anxiety contribute to the escalation of non-communicable diseases through non-adherence to treatment [17]. Those with mental disorders may have a harder time accessing healthcare, treatments may require behavioural changes that may be harder for them. Stigma associated with mental disorders is identified as a barrier to access the health facilities [3,18]. According to the findings of a population-based study [19], it was found that older people with multimorbidity are more likely to experience depressive symptoms in later life [19]. Researches have identified that functional health factors acts as a mediator between multimorbidity and depression, especially when it comes to older women and very few have reported it [20]. Also most of the researches have recommended further longitudinal research to understand functional and behavioural health in multimorbidity-depression relationships [20–22]. The WHO says depression is 50% more prevalent in women than in men, and Indians are among the most depressed worldwide [18].
As India is the most populous country and the largest democracy, is now emerging as the sixth-largest economy in the world. It is recently seeing a demographic transition with increase in elderly population. In accordance with the United Nations definition of a "Graying Nation", a country is defined as a greying country where the percentage of people who are over 60 years of age is at least 7% of its total population [23]. There were almost 7.7% of people in India, at the dawn of the millennium, were old, and this figure increased to 8.6% in 2011, and 9.4%, in 2017 [24]. Also most of the researcher have forecasted by seeing the trend that by the year 2050, there will be 20% of the elderly people ( almost 300 million) [25–27].
From 2011 through 2041, India is forecast to gain a demographic advantage due to a larger proportion of the population in the working age group [25]. And after 2041, when the aging burden shall begin, the older population may contribute to second demographic growth by accumulating capital from their savings accumulated during their working years [28]. But this depends on developing financial markets, a healthy older population, and social security, all of which seems to be daunting at the moment. Additionally, due to the epidemiological transition, a large portion of the burden of disease has been shifted from the youth to the elderly [29]. Non Communicable Diseases (NCDs) exceeded 50% in the 30–34 age group and were highest at 78.8% in the 65–69 age group [29]. An increasing Life Expectancy can be attributed to increased longevity and growing society, but it can also be attributed to an increased demand for healthcare facilities, placing an increased burden on the state, society, and families in India [19]. Out-of-pocket health expenses account for more than 70% of health expenditures in India, leaving the older population vulnerable to health problems [30].The Disability Adjusted Life Year (DALY) rate between 1990 and 2016 was the highest for diseases such as diabetes (80.0%), ischaemic heart disease (33.9%), and sense organ diseases (mainly vision and hearing loss disorders 21.7%) [31].
In India, mental illness is prevalent and pervasive, especially among older adults living in a distressed socioeconomic situation [29]. Researches have reported due to the social stigma of mental illness in older adults and the lack of trained mental health professionals, the prevalence of mental illness among older adults is higher than the reported figures [32,33].There were 197 million people in India who lived with a mental disorder in 2017. Of those people, 45 million suffered from depression and another 44 million from anxiety [34]. Mental disorders are a major contributor to the total number of DALYs in India, and their share increased from 2.5% in 1990 to 4.7% in 2017 [34]. There is a high incidence of depression among the elderly population of India with females being predominant in the group [35].
As per the census 2011 the majority of older Indian adults live in rural areas, over 70% of whom are illiterate, while over half of them do not have a source of income [36,37]. Quacks, folk healers, or AYUSH practitioners provide health and mental health care to older adults in rural areas, since allopathic doctors and hospitals are far away in urban areas and elderly people often have difficulty approaching hospitals [38]. Though there are scarce research publications available related to depression among elderly population in rural area, but those available shows that as a result of different population characteristics, depression prevalence is slightly but significantly higher in rural areas than in urban areas [39]. However these studies are conducted in a small population. In a study in South India it was revealed that the prevalence of depression varies among rural and urban area [35,40].
In India National Mental Health Policy, 2014 aims to reduce distress, disability, exclusion morbidity and premature mortality associated with mental health problems across the life-span of a person [41]. Nevertheless, a larger part of the policy is focused on ensuring the mental health of the population as a whole, with little emphasis on mental health of the elderly [42]. The reality is, with the presence of mental health disorders and comorbid conditions, the elderly population is more likely to suffer from mental health problems, contributing to a larger burden of dual disease in the country as a whole [43]. Though mental disorders are studied in different parts of India, including in the National Mental Health Survey there has been very limited resource available which highlights the prevalence of state-wise and gender-wise depression its association with Disability-Adjusted Life Years (DALYs).
Researches have revealed that female elders are more likely to suffer from physical and mental disabilities that greatly reduce their quality of life [44]. Studies in the United States have shown that elderly women are more susceptible to depression, experience longer and more persistent depression, and have lower mortality rates once depressed [44,45]. There is no doubt that late-life depression poses a significant public health problem since it is widespread and expensive, associated with disability, re-hospitalization, and even death among those with chronic diseases [46,47]. According to the literature Compared to elderly men, women are more likely to suffer from chronic morbidity, poor vision, cataracts, high blood pressure, back pain/slipped disk, malnutrition, depression, impaired physical performance, and elder abuse, women have difficulty coping with these health problems because they are widowed, economically dependent, lack proper food and clothing, fear the future, lack care, and suffer from progressive health decline [15,48-53]. However, existing policies and programmatic capacities are inadequate and lack gender sensitivity to address the socioeconomic and health needs of women. By utilizing secondary data from Longitudinal Ageing Study of India (LASI), this study fills a gap by identifying the prevalence of common mental disorders like depression in elderly females in India by identifying a number of factors related to it, especially depression, in females in India and its trend with respect to age, economic status, place of residence, marital status, alcohol consumption, tobacco consumption, and physical activity. The study also shows its trend in urban as well as rural areas. It will provide valuable insight to policymakers so that they can develop the necessary policy implications to address the rapidly increasing rate of depression among the female elderly population in India.
Aim and objective
What is the prevalence of depression among women in different regions and demographic groups in India, and what factors may contribute to these differences?
• To determine the extent of depression among women in various regions and demographic groups in India.
• To determine the factors associated with depression among the elderly women in India.
Method
The data from the Longitudinal ageing study in India (LASI) Wave 1 (2017-2018) was used to understand the burden of depression among older women above 60 Years in India and to explore the geographic distribution of depression in India. A public domain LASI dataset was obtained from the Gateway to Ageing Portal once the abstract submission was approved. In light of the fact that the data is secondary data, both national and international forums have approved the use of the data. A number of filters were applied to the data to obtain 16,637 samples from women aged 60 and older. Their distribution was calculated using descriptive statistics by gender, age, place of residence, and education status. The data from the Longitudinal Ageing Study In India (LASI) Wave 1 (2017-2018) was used to understand the burden of depression among the older women above 60 Y in India and to explore the geographic distribution of the depression in India. LASI is the first longitudinal dataset in India to provide a reliable basis for designing policies and programmes for the older population's social, health, and economic wellbeing. LASI uses Computer-Assisted Personal Interview (CAPI) technology, internationally Harmonized/ Gold Standard Survey Protocol, Comprehensive Range of Biomarkers. Multistage stratified area probability cluster sampling design is used for selecting the representative sample in each stage. The eligibility criteria was older adults aged 45 Years and above (including spouses irrespective of age).
The eventual unit of observation of LASI was LASI-Eligible Household (LEH) with at least one-member age 45 and above. LASI adopted a multistage stratified area probability cluster sampling design to arrive at the eventual units of observation. All the 30 Indian States and six Union Territories were selected for the survey. The states were further divided in to Districts, Sub districts, Talukas, Tehsils and Blocks. The samples were selected in four stages, where in the first state was for selection of Primary Sampling Unit (PSU) and second and third stage was for selection of Secondary Sampling Unit (SSU ), and fourth stage was for selection of households. For assessing depression, the tools used are Centre for Epidemiologic Studies Depression (CES-D) to find the symptoms of depression and Composite International Diagnostic Interview-Short Form (CIDI-SF) scale to diagnose major depression. For more details please refer to LASI India Report 2020 at 29.
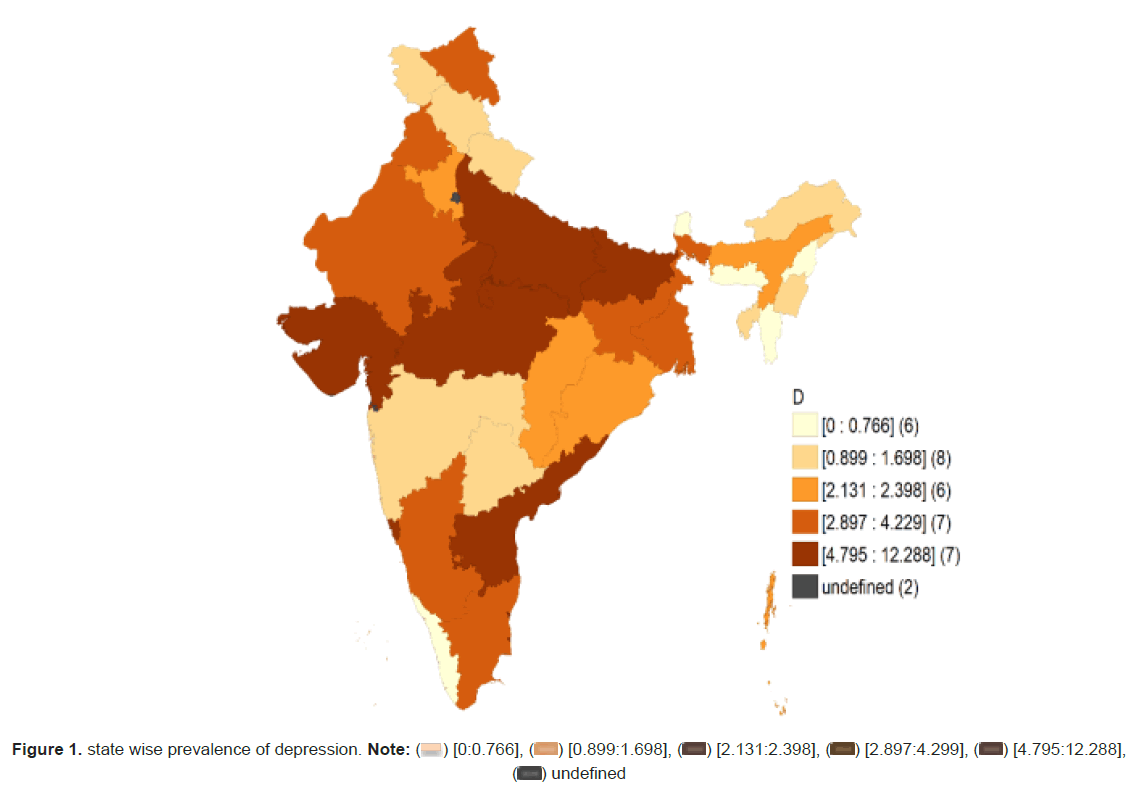
It is a cross sectional study aimed to explore the factors responsible to determine the prevalence among elderly women of 60 and above in India using the intersectional analysis. We were able to explore the intersecting patterns between different variables and how people are positioned simultaneously and position themselves in different multiple categories based on the type of place of residence, age and level of education. Through the study we further aim to determine the prevalence of depression among elderly female in the age group of 60 in different states using the Chloropleth map. Binary Logistic Regression was used to estimate the prime factors associated with depression since depression was a binary yes or no variable. Odds Ratio was calculated using clinical and demographic variables. Unadjusted odd ratio was obtained through the first regression model to control other variables. Our second regression model takes into account other variables depicted in Fig:4 to determine the risk factors for depression with a confidence interval of 0.001. Using intersectional analysis, we explored how people are positioned simultaneously according to their place of residence, their age, and their level of education, as well as how they position themselves in different multiple categories and if conditional probability of depression exists in all categories. Our next step was to compute the prevalence of depression at the state level. To understand the distribution of depression prevalence among Indian states and Union Territories, we have plotted the Choropleth map using the GeoDa software.
Results
Their distribution was calculated using descriptive statistics by gender, age, place of residence, and education status. Binary Logistic Regression was used to estimate the prime factors associated with depression since depression was a binary yes or no variable. Unadjusted odd ratio was obtained through the first regression model to control other variables. Our second regression model takes into account other variables such as age, place of residence, marital status, education, employment, household income, alcohol, tobacco, physical activity, and yoga to determine the risk factors for depression. Using intersectional analysis, we explored how people are positioned simultaneously according to their place of residence, their age, and their level of education, as well as how they position themselves in different multiple categories. To understand the distribution of depression prevalence among Indian states and Union Territories, we have plotted the Choropleth map using the GeoDa software.
The Independent variables used in the study are age, which was categorised as 60-64, 65-69, 70-74 and more than 75, place of residence, marital status, education status of the participants, employment status, household income, alcohol consumption and tobacco consumption, physical activity and Yoga. Depression is the outcome variable. The variable is Nominal variable and reported as Yes for those who were having the Depressive mood and no for those who don’t. The survey used the Composite International Diagnostic Interview-Short Form (CIDI-SF) scale. The tool was used by the non-clinician but trained on the specific tool to collect the information. The tool has been found as reliable for collecting the data on depression by the nonclinician and the tool was easy to understand and implement. The tool was used by the trained professional in their local language to maintain the reliability and validity of the data.
Table 1 shows the demographic characteristics of the study participants. A total of 14553 women aged 60 and above had participated in the survey. Participants below the age of 60 was not included in the analysis. Women in the age group of 60-64 age group were 33.6% and the proportion of the participants decrease with the increase in the age and women in the age group of more than 75 years were 24.4%. This increase in the proportion of the participants would be because of the increase in the life expectancy because of the accessibility of the health care facility. Majority of the study participants 63.8% belong to the rural area. Majority of the women are married 90.2%. Most of the women 46.2% had some basic schooling and 31.6% had completed the education of 10 year and more. The employment status of the study participants highlights that 60.7% of the women are working. The household income of the study participants highlights that almost all the categories of the wealth almost are in equal proportion. Women who are consuming alcohol was 3.9%, 19% consume tobacco and only 12.2% of the study participants do the exercise regularly.
| N | Percentage | ||
|---|---|---|---|
| Age | 60-64 | 4183 | 25.30% |
| 65-69 | 5142 | 31.10% | |
| 70-74 | 3240 | 19.60% | |
| more than 75 | 3985 | 24.10% | |
| Place of residence | Rural | 10763 | 65.10% |
| Urban | 5770 | 34.90% | |
| Current marital Status of the person | Currently Married | 6325 | 43.5 |
| Widowed | 7853 | 54% | |
| Divorced/separated/Deserted | 372 | 2.50% | |
| Education | less than 5 years | 3231 | 22.20% |
| 5 to 9 years | 6724 | 46.20% | |
| more than 10 years | 4599 | 31.60% | |
| Currently working N= 7380 | Yes | 2427 | 32.9 |
| No | 4953 | 67.1 | |
| Household income | Poorest | 3521 | 22.80% |
| Poorer | 3700 | 22.60% | |
| Middle | 3225 | 19.70% | |
| Richer | 3012 | 18.40% | |
| Richest | 2521 | 15.40% | |
| Alcohol | Yes | 621 | 4.30% |
| No | 13932 | 96.10% | |
| Tobacco | Yes | 3364 | 23.10% |
| No | 11189 | 76.90% | |
| Physical activity | Yes | 1294 | 8.90% |
| No | 13259 | 91.10% |
Table 1: Demographic characteristics of the study participants.
Figure 1 shows that the prevalence of depression was highest i.e., more than 25% were in Punjab 25.4%, Uttar- Pradesh 34.5%, Madhya-Pradesh 25.10%, Gujarat 26%. The state wise data will provide the insight to the policy makers that which state are having the more burden of depression and will help them in understanding the pattern and plan the effective and successful strategies to mitigate the problem.
Table 2 regression was done to know the risk factors associated with the depression. First of all, unadjusted odds ratio was calculated to know the association between the independent and outcome variables then another model was obtained to know the risk factors. To run the regression some variables like the Age was categorised as 60-70, 71-80 and more than 81 to maintain the homogeneity similarly, place of residence was categorised as Rural and Urban were urban was considered as the reference category, Marital status was re categorised in to Married, Widowed and separated and married was considered as reference category. Education was categorised in to illiterate and literate and literate was considered as the reference category. Wealth quintile was categorised in to Poor, Middle and Rich. Participants belong to the rich category was considered as the reference category.
| Adjusted Odds Ratio | Un-Adjusted Odds Ratio | ||||||
|---|---|---|---|---|---|---|---|
| Name of the Variable | Categories of the variable | Odds Ratio | Confidence Interval | P value | Odds Ratio | Confidence Interval | P value |
| Age | 60-70 | 1 | |||||
| 71-80 | 0.97 | 0.89-1.05 | 0.62 | 0.82 | 0.74-0.88 | 0.001 | |
| More than 81 | 0.83 | 0.76-0.90 | 0.001 | 0.57 | 0.51-0.62 | 0.001 | |
| Place of Residence | Rural | 1.32 | 1.23-1.44 | 0.71 | 1.26 | 1.15-1.336 | 0.001 |
| Urban | 1 | 1 | |||||
| Marital Status | Married | 1 | 1 | ||||
| Widowed/Seperated | 1.7 | 1.56-1.85 | 0.001 | 1.53 | 1.40-1.65 | 0.001 | |
| Education | Illiterate | 1.23 | 1.10-1.37 | 0.002 | 1.03 | 0.93-1.15 | 0.06 |
| Literate | 1 | 1 | |||||
| Currently working status | Yes | 1 | 1 | ||||
| No | 1.2 | 1.12-1.30 | 0.001 | 1 | .91-1.07 | 0.048 | |
| Wealth Quintile | Poor | 1.16 | 1.03-1.30 | 0 | 1.2 | 1.09-1.36 | 0.001 |
| Middle | 1.09 | 0.97-1.21 | 0.01 | 1.06 | .95-1.19 | 0 | |
| Rich | 1 | 1 | |||||
| Tobacco consumption | Yes | 1.2 | 1.10-1.30 | 0.001 | 1.2 | 1.10-1.30 | 0.001 |
| No | 1 | ||||||
| Alcohol consumption | Yes | 1.16 | 1.04-1.29 | 0 | 1.1 | .98-1.22 | 0.47 |
| No | 1 | ||||||
| Physical Activities | Yes | 0.94 | 0.83-0.98 | 0.01 | 1.01 | 0.94-1.09 | 0 |
| No | 1 | 1 | |||||
Table 2: Multivariate logistic regression of sociodemographic and associated risk factors.
The Table 3 highlight that participants reside in the rural areas had higher odds of developing depression in the unadjusted odds ratio and was insignificant but while adjusted for the other variable the odds of developing depression was 1.26 (1.15- 1.336) p<0.05. Also, the odds of developing the depression among the widowed/separated was 1.53 (1.40-1.65) times more chance of developing depression when compared with the married participants. People with the low level of the literacy was significantly associated with the development of depression when compared with the people with the higher literacy and is statically significant with p<0.05. this would be because people with higher literacy have better cognitive level and had more knowledge and take precaution or visit the doctors early and get the treatment. As a result, it was explored that the participants belong to the poor wealth quintile have higher odds of developing depression then the people belong to the rich wealth quintile. The odds decrease with the increase in the wealth quintile. Also, the behavioural risk factors like the consumption of tobacco had 1.20 times more chance of developing depression then the participants who don’t consume tobacco and is statically significant with p<0.05. Even when adjusted for the other variable the odds is greater than 1 which means consumption of tobacco was a risk factor similarly consumption of alcohol was a risk factor but while adjusting for the other variable the direction of the relationship was change and is statically significant with p value less than 0.05. Doing physical activity was a protective factor but while adjusting for the other variable the direction of the relationship changes and it became the risk factors1.01(0.94-1.09) with p Less than 0.05.
| Place of residence | ||||
|---|---|---|---|---|
| State | Rural | Urban | ||
| Count | Column N % | Count | Column N % | |
| Jammu & Kashmir | 30 | 1.40% | 11 | 1.30% |
| Himachal Pradesh | 34 | 1.60% | 3 | 0.30% |
| Punjab | 102 | 4.80% | 25 | 2.80% |
| Chandigarh | 1 | 0.00% | 22 | 2.50% |
| Uttarakhand | 44 | 2.10% | 6 | 0.70% |
| Haryana | 45 | 2.10% | 19 | 2.20% |
| Delhi | 3 | 0.10% | 41 | 4.70% |
| Rajasthan | 78 | 3.70% | 12 | 1.40% |
| Uttar Pradesh | 310 | 14.60% | 59 | 6.70% |
| Bihar | 162 | 7.60% | 18 | 2.00% |
| Sikkim | 0 | 0.00% | 0 | 0.00% |
| Arunachal | 27 | 1.30% | 2 | 0.20% |
| Nagaland | 11 | 0.50% | 1 | 0.10% |
| Manipur | 18 | 0.80% | 9 | 1.00% |
| Mizoram | 4 | 0.20% | 5 | 0.60% |
| Tripura | 42 | 2.00% | 9 | 1.00% |
| Meghalaya | 20 | 0.90% | 0 | 0.00% |
| Assam | 59 | 2.80% | 13 | 1.50% |
| West Bengal | 79 | 3.70% | 44 | 5.00% |
| Jharkhand | 99 | 4.70% | 22 | 2.50% |
| Odisha | 63 | 3.00% | 8 | 0.90% |
| Chhatisgarh | 57 | 2.70% | 8 | 0.90% |
| Madhya Pradesh | 129 | 6.10% | 45 | 5.10% |
| Gujarat | 95 | 4.50% | 54 | 6.10% |
| Daman & Diu | 14 | 0.70% | 28 | 3.20% |
| Dadra&Nagar Haveli | 18 | 0.80% | 9 | 1.00% |
| Maharashtra | 123 | 5.80% | 72 | 8.20% |
| Andhra Pradesh | 78 | 3.70% | 24 | 2.70% |
| Karnataka | 94 | 4.40% | 50 | 5.70% |
| Goa | 37 | 1.70% | 35 | 4.00% |
| Lakshadweep | 3 | 0.10% | 12 | 1.40% |
| Kerala | 47 | 2.20% | 45 | 5.10% |
| Tamil Nadu | 92 | 4.30% | 93 | 10.60% |
| Puducherry | 24 | 1.10% | 40 | 4.60% |
| Andaman&Nicobar | 19 | 0.90% | 11 | 1.30% |
| Telangana | 63 | 3.00% | 24 | 2.70% |
Table 3: Prevalence of the depression based on the rural and urban.
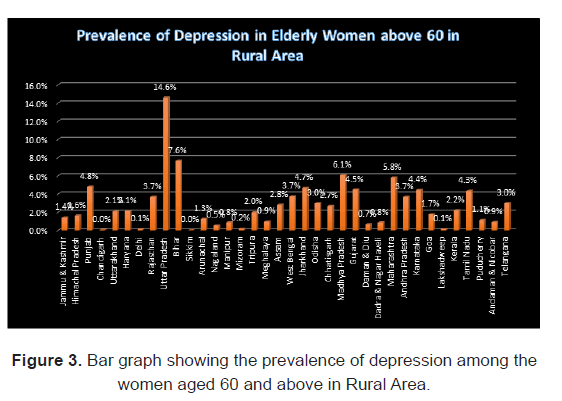
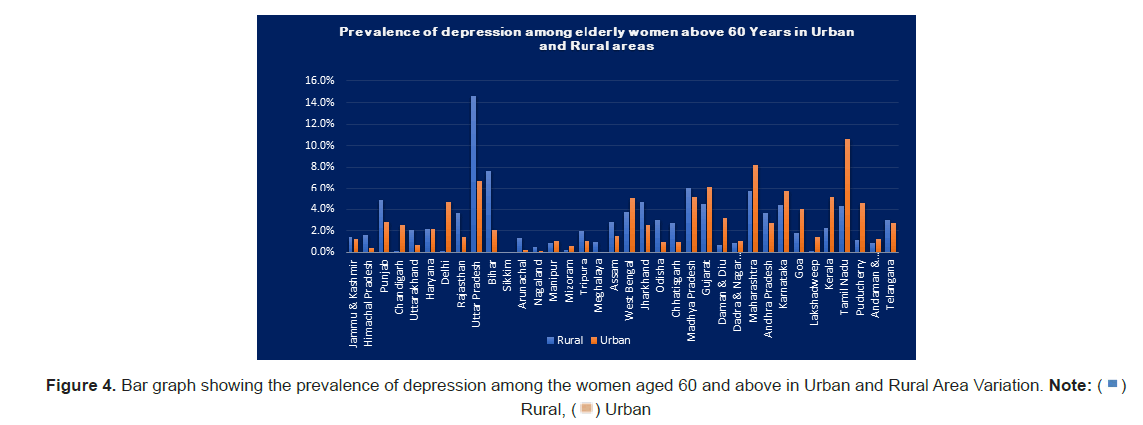
It was found that rural was the dominant and rural area like Uttar Pradesh, Bihar, Madhya Pradesh, Maharashtra, Himachal Pradesh, Punjab, Uttarakhand, Rajasthan, Uttar Pradesh, Bihar, Arunachala Pradesh, Nagaland, Tripura, Meghalaya, Assam, Jharkhand, Odisha and Chhattisgarh had prevalence more than 75%.
State with the urban area where depression was more than 75% had Tamil Nādu, Maharashtra, Madhya Pradesh, Delhi and Lakshadweep.
To explore the intersecting pattern of the women aged 60 and above, reside in rural or urban, and the type of the education was intersected to explore the different pattern.
The Table 4 highlight that the prevalence of the most of the participants from the rural places had depression. Women aged 65 to 69 being illiterate and from the rural part was 20.5% similarly if the elderly women were more than 75 age and from rural was 18.9% and if the same condition was from the urban then the prevalence was 13%. Only type of the place of the residence reduces the 6-point prevalence. The data also revealed that there has been an increased in the trend of prevalence with the increase in the age and being reside in the rural area. Also, if the participants are from the urban area, then the trend was reverse and there has been decreasing point in prevalence of depression among the participants with age more than 60 years (Figure 2). Similarly, if the women were literate and age more than 75 and belong to the rural the prevalence was 28.6% and in the same scenario if the women was literate, age more than 75 and belong to the urban then the prevalence of depression was reduced to 14 point which was just half the prevalence of depression if the women reside in the rural part. The intersectional analysis highlights that type of place is the major factor for the development of depression however the cause was not established which was beyond the scope of this analysis.
| Intersectional variable | Depression |
|---|---|
| Illiterate, age 60-64 Rural | 16.90% |
| Illiterate, age 60-64 Urban | 15.50% |
| Illiterate, age 65-69 Rural | 20.50% |
| Illiterate, age 65-69 Urban | 13.90% |
| Illiterate, age 70-74 Rural | 19.60% |
| Illiterate, age 70-74 Urban | 17.50% |
| Illiterate, age more than 75 Rural | 18.90% |
| Illiterate, age more than 75 Urban | 13% |
| Literate, age 60-64 Rural | 13% |
| Literate, age 60-64 Urban | 10.60% |
| Literate, age 65-69 Rural | 14.50% |
| Literate, age 60-64 Urban | 10.80% |
| Literate, age 70-74 Rural | 10% |
| Literate age 70-74 Urban | 11.10% |
| Literate, age more than 75 Rural | 28.60% |
| Literate age more than 75 Urban | 14.20% |
Table 4: Intersectional analysis based on the education status, age and type of the residence of the elderly women aged 60 and above LASI 2017-1018.
Discussion
The study participants consisted of 16,737 women aged 60 and above, with participants under the age of 60 excluded from the analysis. The demographic characteristics of the participants were analysed and several important findings were observed. The age group of 60-64 years was the largest with 33.6% of the participants, while the proportion of participants decreased as age increased, with 24.4% of the participants aged over 75 years. This increase in the proportion of older participants is likely due to improved access to healthcare and increased life expectancy (Figure 3).
The majority of the study participants, 63.8%, were from rural areas, and 90.2% were married. A significant proportion, 46.2%, had received basic schooling, while 31.6% had completed at least 10 years of education. The employment status of the participants showed that 60.7% were working, with household income being relatively equal among the different wealth categories. The study also found that a small proportion of the participants, 3.9%, consumed alcohol, while 19% consumed tobacco, and only 12.2% reported regularly exercising. These findings are similar to the results of the 54, which reported that a majority of women in India reside in rural areas, have low levels of education and employment, and engage in unhealthy behaviours such as tobacco and alcohol consumption [54].
It is important to note that these findings provide important insights for policymakers and public health practitioners, highlighting the need for targeted interventions to address the health needs of older women in India, particularly those in rural areas. Further research is needed to understand the impact of demographic and socioeconomic factors on health and wellbeing in this population, and to develop effective strategies to address the challenges faced by older women in India.
The findings of the study on depression levels and aging are similar to the Global Adult Tobacco Survey (GATS) 55, which also found that tobacco use is associated with increased levels of depression [55]. GATS also found that individuals with higher levels of education and those who are employed are less likely to use tobacco and have lower levels of depression. Similarly, the study found that physical activity is associated with lower levels of depression, while GATS found that individuals who are physically active are less likely to use tobacco. However, GATS did not specifically address the relationship between wealth quintiles and depression levels. The study's finding that depression levels were higher among rural participants compared to urban participants is not addressed in GATS. The findings of the study are consistent with other reports regarding depression and risk factors [56,57]. The study found that depression levels increased with age from 60 to over 75 years, which is similar to other studies that have shown that older adults are at increased risk for depression [35,58]. Additionally, the study found that depression levels were higher among individuals who consumed alcohol or tobacco, which is also in line with other reports that have linked substance use with increased risk for depression [59,60].
However, the study also found some unique findings. For example, the study found that a higher proportion of rural participants reported increased levels of depression compared to urban participants, which is not typically reported in other studies. Additionally, the study found that regularly engaging in physical activity was associated with lower levels of depression, but after adjusting for other variables, physical activity became a risk factor, which is also not a commonly reported finding.
The study's findings on the associations between depression and education, wealth quintile, and marital status are also consistent with other reports. Education, wealth, and marital status have all been linked with mental health, and the study's findings provide further support for these relationships [27,61].
Overall, the study adds to the growing body of literature on depression and its risk factors, particularly in older adults. Further research is needed to better the findings of this study that rural areas have a higher prevalence of depression compared to urban areas aligns with previous studies and reports on the topic. This disparity could be due to factors such as lack of access to healthcare, lower socio-economic status, and cultural stigma surrounding mental health in rural areas [60,62]. However, it's worth noting that while the study found that depression levels were higher in rural areas, there were also some urban areas like Chandigarh, Delhi and Lakshadweep where depression levels were higher. This indicates that the relationship between urbanization and depression levels is complex and not straightforward. Further research is needed to fully understand the factors contributing to the higher levels of depression in both rural and urban areas. understand the complex relationships between depression, demographics, and risk factors. The findings of the study highlight the significance of the place of residence in the development of depression among elderly women, with the rural area being associated with a higher prevalence of depression compared to the urban area. The results show that the prevalence of depression among illiterate women in the rural area was 20.5% for women aged 65-69, and 18.9% for women over 75 years of age, compared to a prevalence of 13% for women over 75 years of age in the urban area. This shows a reduction of 6 points in the prevalence of depression in the urban area compared to the rural area which is in line with the other studies (Figures 4 and 5) [23,35].
Additionally, the study found that the trend of depression prevalence increased with age in the rural area and decreased with age in the urban area. Similarly, the prevalence of depression was found to be higher among literate women over 75 years of age in the rural area (28.6%) compared to urban area (14%) which was just half the prevalence in rural area. The intersectional analysis indicates that the type of place of residence is the major factor for the development of depression, although the underlying cause was not established in the study.
The strength of this study lies in its use of intersectional analysis, which considers the intersection of multiple factors, such as age, literacy, and place of residence, in the development of depression. This provides a more nuanced understanding of the complex relationships between these factors and the development of depression.
However, the weakness of this study is that the underlying cause of the relationship between place of residence and depression was not established. Further research is needed to understand the specific factors that contribute to the higher prevalence of depression in the rural area and the protective effect of urban residency on depression. Additionally, the study is limited by the small sample size and the lack of data on other possible risk factors for depression.
Overall, the study provides important insights into the relationship between place of residence and depression among elderly women and highlights the importance of considering multiple factors in the analysis of mental health outcomes.
Policy implications and recommendations based on this study
• Addressing the need for mental health services in rural areas: The study highlights that women living in rural areas are more susceptible to depression as compared to their urban counterparts. Thus, it becomes imperative for the government to focus on providing mental health services in rural areas to help reduce the prevalence of depression.
• Literacy and mental health awareness programs: The study shows that illiterate women are more prone to depression. Hence, promoting literacy and creating mental health awareness programs can help in reducing the incidence of depression.
• Focus on elderly women: The study highlights that elderly women are more susceptible to depression. The government can focus on creating programs that cater to the needs of elderly women, both in urban and rural areas, to reduce the incidence of depression.
• Intersectional approach to mental health: The study highlights the importance of an intersectional approach to mental health, which considers multiple factors such as age, literacy, and place of residence. The government can use this approach to develop programs that target specific populations and address the root causes of depression.
Conclusion
In conclusion, the study analysed the prevalence of depression among elderly women aged 65 to 69 and more than 75 in rural and urban areas. The results showed that the prevalence of depression among rural elderly women was higher compared to urban elderly women. However a disparity among states was found. The trend of prevalence increased with age among rural women and decreased with age among urban women. Additionally, the intersectional analysis showed that the type of place of residence was the major factor for the development of depression.
The study highlights the need for mental health policies and interventions to address the higher prevalence of depression among elderly rural women. This may involve providing access to mental health services, creating community support systems, and raising awareness about mental health in rural areas. Furthermore, there is a need for further research to understand the underlying causes of depression among rural elderly women.
While the intersectional analysis provides a useful insight into the complex relationship between demographic factors and mental health, it is important to acknowledge its limitations. The study did not establish the cause of depression, and it was beyond the scope of this analysis. Moreover, the study relied on self-reported data, which may be subject to bias.
In summary, the study provides valuable information on the prevalence of depression among elderly women in rural and urban areas and the importance of considering the intersection of demographic factors in understanding mental health. The results of this study can inform policy and practice to improve mental health outcomes among elderly women, especially those living in rural areas.
Limitations
• The sample size: The study may not accurately reflect the prevalence of depression in the entire population due to the limited sample size.
• Lack of control groups: The study does not have control groups to compare the results, which limits its validity.
• Cross-sectional design: The study is cross-sectional, which means that it only provides a snapshot of the situation at a particular time. Hence, it cannot be used to establish causal relationships between the variables studied.
• Uncontrolled variables: The study does not control for other variables that may impact depression such as socioeconomic status, physical health, and access to healthcare services.
References
- Pryor L, Silva MAD, Melchior M. Mental health and global strategies to reduce NCDs and premature mortality. Lancet Public Health. 2017;2:e350–e351.
[Crossref], [Google Scholar], [Pubmed]
- Minas H, Tsutsumi A, Izutsu T, Goetzke K, Thornicroft G. Comprehensive SDG goal and targets for non-communicable diseases and mental health. Int J Ment Health Syst.2015; 9:12.
[Crossref], [Google Scholar], [Pubmed]
- Stein DJ, Benjet C, Gureje O, Lund C, Scott KM, et al. Integrating mental health with other non-communicable diseases. BMJ. 2019; 364:l295.
[Crossref], [Google Scholar], [Pubmed]
- Devlin MJ, Yanovski SZ, Wilson GT. Obesity: What mental health professionals need to know. Am J Psychiatry. 2000;157:854–866.
[Crossref], [Google Scholar], [Pubmed]
- Beauchamp MR, Puterman E, Lubans DR. Physical inactivity and mental health in late adolescence.JAMA Psychiatry. 2018;75:543-544.
[Crossref], [Google Scholar], [Pubmed]
- WHO. Depression. 2015.
- Grover S, Malhotra N. Depression in elderly: A review of Indian research. J Geriatr Ment Health. 2015; 2:4.
[Crossref], [Google Scholar]
- Keeratisiroj O, Kitreerawutiwong N, Mekrungrongwong S. Development of Self-Active Aging Index (S-AAI) among rural elderly in lower northern Thailand classified by age and gender. Sci Rep. 2023; 13:2676.
[Crossref], [Google Scholar], [Pubmed]
- Mental health and global strategies to reduce NCDs and premature mortality
- Kim H, Jeong W, Kwon J, Kim Y, Park EC, et al. Association between depression and the risk of Alzheimer’s disease using the Korean National Health Insurance Service-Elderly. Sci Rep.2021;11: 22591.
[Crossref], [Google Scholar], [Pubmed]
- Vaughn CB, Jakimovski D, Kavak KS, Ramanathan M, Benedict. Epidemiology and treatment of multiple sclerosis in elderly populations. Nat Rev Neurol. 2019;15:329–342 .
[Crossref], [Google Scholar], [Pubmed]
- Boots AMH. The influence of ageing on the development and management of rheumatoid arthritis. Nat Rev Rheumatol. 2013;9:604–613.
[Crossref], [Google Scholar], [Pubmed]
- Rajadurai J, Lopez EA, Rahajoe AU, Goh PP, Uboldejpracharak Y, et al. Women’s cardiovascular health: Perspectives from South-East Asia. Nat Rev Cardiol. 2012; 9:464–477.
[Crossref], [Google Scholar], [Pubmed]
- Maiti S, Akhtar S, Upadhyay AK, Mohanty SK. Socioeconomic inequality in awareness, treatment and control of diabetes among adults in India: Evidence from National Family Health Survey of India (NFHS), 2019–2021. Sci Rep. 2023; 13:2971.
[Crossref], [Google Scholar], [Pubmed]
- Fan Y, He D. Self-rated health, socioeconomic status and all-cause mortality in Chinese middle-aged and elderly adults. Sci Rep. 2022;12:9309.
[Crossref], [Google Scholar], [Pubmed]
- Anwar N, Kuppili PP, Balhara YPS. Depression and physical noncommunicable diseases: The need for an integrated approach. WHO South-East Asia J. Public Health. 2017; 6:12–17.
[Crossref], [Google Scholar], [Pubmed]
- Chawla S, Gour N, Goel PK, Rohilla R. Depression and its correlates among geriatric people: A community based study from Southern Haryana, India. Indian J Community Fam Med. 2018; 4:49.
[Crossref], [Google Scholar], [Pubmed]
- Bohra N, Srivastava S, Bhatia MS. Depression in women in Indian context. Indian J Psychiatry. 2015; 57:S239–S245.
[Crossref], [Google Scholar], [Pubmed]
- Jayasankar P, Manjunatha N, Rao GN, Gururaj G, Mathew Varghese, et al. Epidemiology of common mental disorders: Results from “National Mental Health Survey” of India. Indian J Psychiatry. 2016; 64:13.
[Crossref], [Google Scholar], [Pubmed]
- Ansari S, Anand A, Hossain B. Multimorbidity and depression among older adults in India: Mediating role of functional and behavioural health. PLOS ONE. 2022;17: e0269646.
[Crossref], [Google Scholar], [Pubmed]
- Jiang C, Zhu F, Qin T. Relationships between chronic diseases and depression among middle-aged and elderly people in China: A Prospective study from CHARLS. Curr Med Sci. 2020;40:858–870.
[Crossref], [Google Scholar], [Pubmed]
- Triolo F. The complex interplay between depression and multimorbidity in late life: Risks and pathways. Mech Ageing Dev. 2020; 192:111383.
[Crossref], [Google Scholar], [Pubmed]
- Sahni B, Bala K, Kumar T, Narangyal A. Prevalence and determinants of geriatric depression in North India: A cross-sectional study. J Fam Med Prim Care. 2020; 9:2332–2336.
[Crossref], [Google Scholar], [Pubmed]
- Sahoo SS. Depression and quality of life among elderly: Comparative cross-sectional study between elderly in community and old age homes in Eastern India. J Educ Health Promot. 2022;11:301.
[Crossref], [Google Scholar], [Pubmed]
- Ram U, Ram F. Demographic transition in india: insights into population growth, composition, and its major drivers. Global Public Health. 2021.
[Crossref], [Google Scholar]
- Rogers WA, Mitzner TL. Envisioning the future for older adults: Autonomy, health, well-being, and social connectedness with technology support. Futures. 2017; 87:133–139.
[Crossref], [Google Scholar], [Pubmed]
- Freeman A. The role of socio-economic status in depression: Results from the COURAGE (aging survey in Europe). BMC Public Health. 2016; 16:1098.
[Crossref], [Google Scholar], [Pubmed]
- Jain N, Goli S. Potential demographic dividend for India, 2001 to 2061: A macro-simulation projection using the spectrum model. Sn Soc Sci. 2022; 2:171.
[Crossref], [Google Scholar], [Pubmed]
- Crossref
- Dey S, Nambiar D, Lakshmi JK, Sheikh K, Reddy KS. Health of the elderly in india: challenges of access and affordability. Aging in Asia: Findings From New and Emerging Data Initiatives (National Academies Press (US). 2012.
- Naveen KHS, Goel AD, Dwivedi S, Hassan MA. Adding life to years: Role of gender and social and family engagement in geriatric depression in rural areas of Northern India. J Fam Med Prim Care. 2020; 9:721.
[Crossref], [Google Scholar], [Pubmed]
- Conner KO. Mental health treatment seeking among older adults with depression: The impact of stigma and race. Am J Geriatr Psychiatry. 2010; 18:531–543.
[Crossref], [Google Scholar], [Pubmed]
- Depla MFIA, De Graaf R, Van Weeghel J, Heeren TJ. The role of stigma in the quality of life of older adults with severe mental illness. Int J Geriatr Psychiatry. 2005; 20:146–153.
[Crossref], [Google Scholar], [Pubmed]
- Sagar R. The burden of mental disorders across the states of India: The Global Burden of Disease Study 1990–2017. Lancet Psychiatry. 2020;7:148–161.
[Crossref], [Google Scholar], [Pubmed]
- Pilania M. Prevalence of depression among the elderly (60 years and above) population in India, 1997–2016: a systematic review and meta-analysis. BMC Public Health. 2019; 19:832.
[Crossref], [Google Scholar], [Pubmed]
- Registrar General I. Census of India 2011: Provisional population totals-India data sheet. Off Regist Gen Census Comm. India Indian Census Bur.2011.
- Tiwari SC, Pandey NM. Status and requirements of geriatric mental health services in India: An evidence-based commentary. Indian J Psychiatry. 2012;54:8–14.
[Crossref], [Google Scholar], [Pubmed]
- Krishnakumar. The old and the ignored. 2008
- Probst J. Rural-urban differences in depression prevalence: Implications for family medicine. Fam Med. 2006;38:653–60.
[Google Scholar], [Pubmed]
- Poongothai S, Pradeepa R, Ganesan A, Mohan V. Prevalence of depression in a large urban south indian population—the chennai urban rural epidemiology study (Cures–70). PLOS ONE. 2009; 4: e7185.
[Crossref], [Google Scholar], [Pubmed]
- National Health Mission. National Mental Health Programme (NMHP). 2020.
- Gupta S, Sagar R. National Mental Health Policy, India (2014): Where have we reached?. Indian J. Psychol Med. 2022;44, 510–515.
[Crossref], [Google Scholar], [Pubmed]
- press information bureau government of india ministry of health and family welfare. Mental Health Policy. 2016.
- Buvneshkumar M, John KR, Logaraj MA. Study on prevalence of depression and associated risk factors among elderly in a rural block of Tamil Nadu. Indian J Public Health. 2018; 62:89.
[Crossref], [Google Scholar], [Pubmed]
- Barry LC, Allore HG, Guo Z, Bruce ML, Gill TM. Higher burden of depression among older women: the effect of onset, persistence, and mortality over time. Arch Gen Psychiatry. 2008; 65:172–178.
[Crossref], [Google Scholar], [Pubmed]
- Dhar HL. Gender, aging, health and society. J Assoc Physicians India. 2011; 49:1012–1020.
[Google Scholar], [Pubmed]
- Beekman AT. Emergence and persistence of late life depression: A 3-year follow-up of the Longitudinal Aging Study Amsterdam. J. Affect. Disord. 2001;65:131–138.
[Crossref], [Google Scholar], [Pubmed]
- Meher T, Muhammad T, Gharge S. The association between single and multiple chronic conditions and depression among older population in India: A comparative study between men and women. Int J Geriatr. Psychiatry. 2022; 37.
[Crossref], [Google Scholar], [Pubmed]
- Marmamula S. Impact of an intervention for avoidable vision loss on visual function in the elderly–The Hyderabad Ocular Morbidity in Elderly Study (HOMES). Eye. 2022; 1–7.
[Crossref], [Google Scholar], [Pubmed]
- Xu X,Yang H. Elderly chronic diseases and catastrophic health expenditure: An important cause of Borderline Poor Families’ return to poverty in rural China. Humanities and Social Sciences Communications. 2022; 9:291.
[Crossref], [Google Scholar]
- Sia A, Tam WWS, Fogel A, Kua EH, Khoo K. Nature-based activities improve the well-being of older adults. Scientific Reports. 2020; 10:18178.
[Crossref], [Google Scholar], [Pubmed]
- Nair S, Sawant N, Thippeswamy H, Desai G. Gender issues in the care of elderly: A narrative review. Indian J Psychol Med. 2021; 43:S48–S52.
[Crossref], [Google Scholar], [Pubmed]
- Ahmed T, Vafaei A, Auais M, Guralnik J, Zunzunegui MV. Gender roles and physical function in older adults: cross-sectional Analysis of the International Mobility in Aging Study (IMIAS). PLoS ONE. 2016; 11:e0156828.
[Crossref], [Google Scholar], [Pubmed]
- National Family Health Survey. National Family Health Survey. 2022.
- Global Adult Tobacco Survey. Global Adult Tobacco Survey. 2020.
- Dhamnetiya D. Trends in incidence and mortality of tuberculosis in India over past three decades: A joinpoint and age–period–cohort analysis. BMC Pulm Med. 2021;21:375.
[Crossref], [Google Scholar], [Pubmed]
- Sathiyamoorthy R, Kalaivani M, Aggarwal P, Gupta SK. Prevalence of pulmonary tuberculosis in India: A systematic review and meta-analysis. Lung India. 2020; 37: 45.
[Crossref], [Google Scholar], [Pubmed]
- Dao ATM, Nguyen VT, Nguyen HV, Nguyen LTK. Factors associated with depression among the elderly living in urban vietnam. BioMed Res. Int. 2018:1–9.
[Crossref], [Google Scholar], [Pubmed]
- Dogan-Sander E, Kohls E, Baldofski S, Rummel-Kluge C. More depressive symptoms, alcohol and drug consumption: increase in mental health symptoms among university students after one year of the COVID-19 pandemic. Front Psychiatry. 2021:12.
[Crossref], [Google Scholar], [Pubmed]
- Quittschalle J. Association of alcohol and tobacco consumption with depression severity in the oldest old. results from the age different old age cohort platform. Int J Environ Res Public Health. 2021;18:7959.
[Crossref], [Google Scholar], [Pubmed]
- Ettman CK, Cohen GH, Galea S. Is wealth associated with depressive symptoms in the United States? Ann Epidemiol. 2020;43:25-31.e1.
[Crossref], [Google Scholar], [Pubmed]
- Cohen AK. Association of adult depression with educational attainment, aspirations, and expectations. Prev Chronic Dis. 2020:17.
[Crossref], [Google Scholar], [Pubmed]

 ) [0:0.766], (
) [0:0.766], ( ) [0.899:1.698], (
) [0.899:1.698], ( ) [2.131:2.398], (
) [2.131:2.398], ( ) [2.897:4.299], (
) [2.897:4.299], ( ) [4.795:12.288],
(
) [4.795:12.288],
( ) undefined
) undefined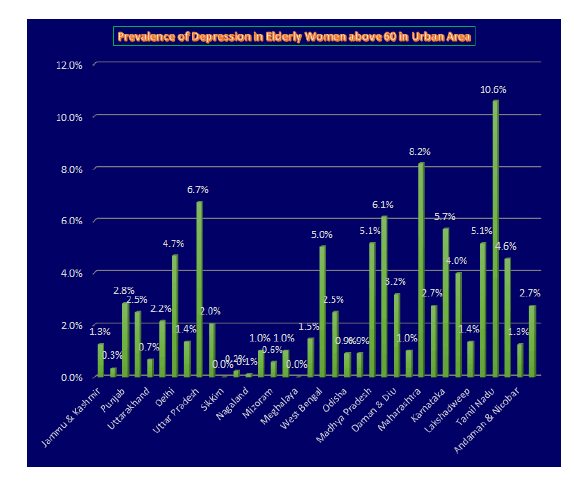
 )
Rural, (
)
Rural, ( ) Urban
) Urban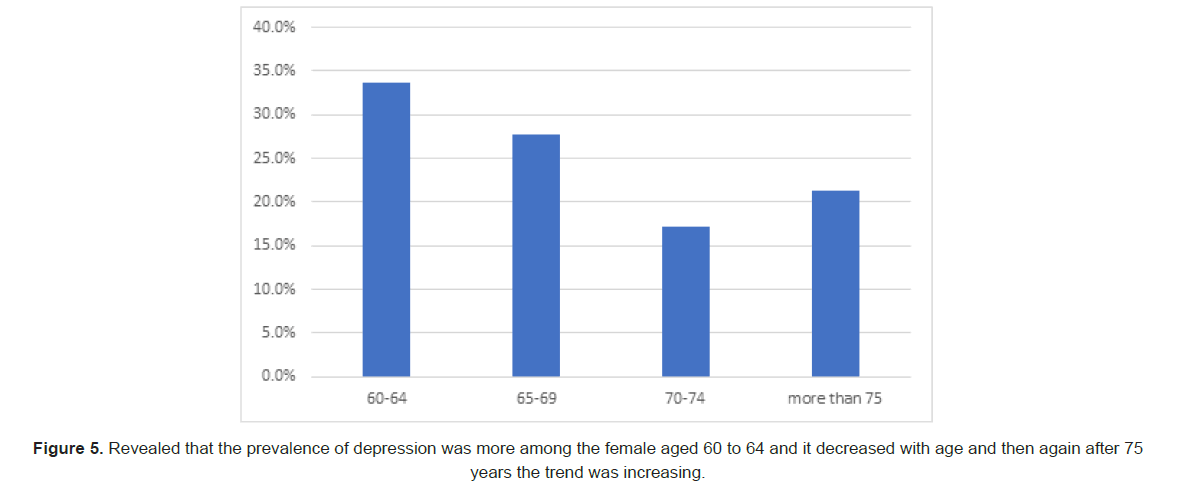



 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.