Prevalence of Multilocular Radiolucencies among Patients Visiting a Chennai-Based Dental Institution
Received: 20-Oct-2022, Manuscript No. AMHSR-22-77873; Editor assigned: 24-Oct-2022, Pre QC No. AMHSR-22-77873 (PQ); Reviewed: 07-Nov-2022 QC No. AMHSR-22-77873; Revised: 22-Feb-2023, Manuscript No. AMHSR-22-77873 (R); Published: 01-Mar-2023, DOI: 10.54608.annalsmedical.2023.93
Citation: Sangavi R, et al. Prevalence of Multilocular Radiolucencies among Patients Visiting a Chennai-Based Dental Institution. Ann Med Health Sci Res. 2023;13:496-499
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Multilocular lesions are unusual in that they can be cystic or cancerous. The clinical, radiological, and histological views of these lesions are all different. The goal of this research was to look into the clinical and radiographic indings of multilocular lesions in panoramic pictures or other advanced imaging techniques like CT or CBCT tomography.
Aim of the study: The aim of this study is to evaluate the prevalence of multilocular radiolucencies among patients visiting a Chennai based dental institution.
Materials and methods: Retrospective analysis of all the cases (Patients referred for panoramic radiographs) was retrieved among the overall data of patients visiting Saveetha dental college, a Chennai based institution. The data was entered in excel spreadsheets and the collected data was analysed using SPSS software version 19. Chi square test was used to statistically evaluate the results.
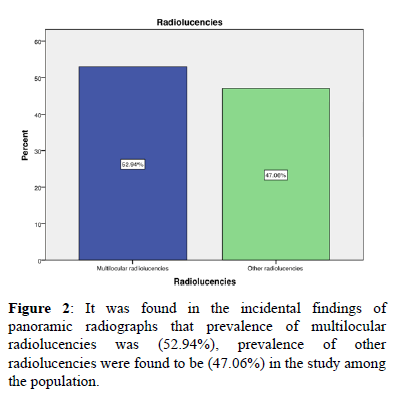
Results: It was found in the incidental indings of panoramic radiographs that prevalence of multilocular radiolucencies was (52.94%), prevalence of other radiolucencies were found to be (47.06%) in the study among the population.
Conclusion: Women were more likely to have ameloblastoma, OKC, and CGCG. Ameloblastoma, OKC, CGCG, and myxoma had comparable age distributions as previous studies. Ameloblastoma, OKC, CGCG, and myxoma were shown to be more prevalent in the mandible. The most prevalent effect on surrounding structures was swelling.
Keywords
Multilocular lesions; Cone beam computed tomography; Panoramic radiography
Introduction
Disease and disorders affecting the facial skeleton are manifold. The unique feature of facial skeleton is such that there are innumerable pathological conditions which are usually asymptomatic and more destructive, thus necessitating a thorough diagnostic approach. Among all the investigatory modalities available, radiograph still plays a vital role as it provides an accurate picture of the morphological characteristic alterations in total. This article highlights one such characteristic radiographic appearance, the multilocular radiolucency and its prevalence. In a previous study, maxilla lesions have a wide range of pathologic views with similar imaging views, getting to know each of the lesions is very important. A wide spectrum of benign and malignant tumours can cause multilocular radiolucencies in the mandible. Multilocular lesions come in a wide range of sizes, as well as treatment options. Dentists may thoroughly investigate the radiographic features of the area following the first diagnosis to identify the size and characteristics of lesions considering the high occurrence of cysts and tumours in the maxilla and mandible. The features of such lesions can occasionally be sufficiently pathognomonic that a specific tumour can be detected early on. Furthermore, radiographs might often result in the incorrect diagnosis of lesions that have already been diagnosed. As per studies conducted, multilocular radiolucency is a lesional appearance on radiographs caused by erosion, bosselation, or scalloping of the endosteal surface near the advancing margin of the lesion, resulting in the characteristic multiple loculated look. Based on the size and number of loculations, multilocular lesions in the jaw can take on a variety of shapes, including honey comb, soap bubble, tennis racket, and scalloped. Moving forward, we can deduce that benign lesions including cysts, odontogenic and non-odontogenic tumors including OKC, ameloblastoma, central giant cell granuloma, cherubism, odontogenic myxoma, aneurysmal bone cyst, central hemangioma and other vascular lesions, and malignant tumors including metastatic tumors and central mucoepidermoid carcinoma can be viewed with multilocular radiopacity will. Several studies have reported that in the early stages of the disease, the general dentist would extract teeth due to misdiagnosis, which would help spread the lesion throughout the bone and therefore made it difficult to remove the tumor in one operation. Therefore, better knowledge and understanding of the radiological findings can lead to early diagnosis, avoiding delays and thus improving the prognosis of the disease. In consideration to the different biological behavior of these lesions, which leads to different surgical interventions, it is important to achieve a correct diagnosis and differential diagnosis of these lesions, since it leads to the selection of the appropriate treatment plan and ultimately accelerates the treatment process and the progression and recurrence of the lesion. Therefore, the purpose of this study was to investigate the prevalence of lesions with multilocular radiographic views in patients [1-8].
Materials and Methods
The present study is a retrospective study carried out in a hospital setting under a specific population predominantly South Indian population. It is a single centred study with a small sample size. It was carried out under institutional review board approval. In this study, data of the patients were collected by complete analysis of the data of 500 patients between June 2020 to March 2021 from a patient management software (DIAS). Data including patients name, age, gender, panoramic radiographs used in patients with incidental findings of dental anomaly were collected and for further analysis the collected data was cross verified by another examiner. The collected data was tabulated using Excel Spreadsheets and the data was analysed using SPSS software version 19. The statistical study used in the study was Chi square test with p value less than 0.005 and confidence interval of 95% [9-14].
Results and Discussion
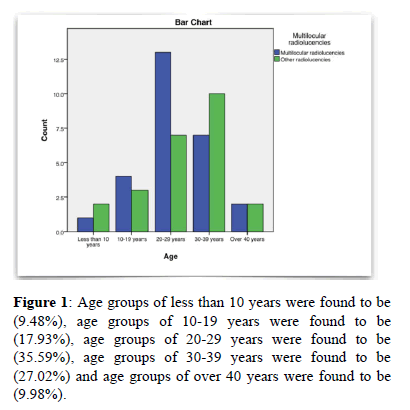
Using these methods, information about the prevalence of multilocular radiolucencies were gathered, here are our conclusive findings. In the present study, it was found that (52.94%) of the male population and (47.06%) of the female population were involved in the study (Figures 1 and 2) [15].
Firstly, multilocular lesions in the jaw include a range of benign and malignant lesions. A dentist should always consider the possibility of vascular lesions or even a malignant tumor when evaluating a multi-cavity lesion and act with caution. Given the different biological behavior of these lesions and consequently different surgical approaches, it is important to achieve the correct diagnosis and differential diagnosis of these lesions. In addition, we may note that many benign lesions cause multilocular lesions in the mandible, which can be divided into those of odontogenic and non-odontogenic origin. Lesions include ameloblastoma, radicular cyst, dentigerous cyst, Odontogenic Keratocyst (OKC), central giant cell granuloma, fibro-osseous lesions, and osteomas. The most common tumor of odontogenic origin is ameloblastoma, which develops from epithelial cell elements and tooth tissues in their various stages of development. From further studies, we can possibly derive that cherubism is more common in children and presents as bilateral multilocular radiolucency. Aneurysmal bone cysts commonly affect people under the age of 20, and the lesions are tender. Unicystic ameloblastoma are observed more frequently in younger patients. Based on a previous study, multiple myeloma occurs in the 40-70 age group, most commonly in males, with an M:F ratio of 4:1. Ameloblastoma is the most common odontogenic neoplasm. It presents a variety of clinical, radiological, and histopathological features. On top of everything mentioned earlier in this discussion, it is of great importance that the dentist must be aware of the jaw manifestations in order to avoid possible complications such as bleeding and pathological fractures. Improved diagnostic and therapeutic options and, in particular, Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) have led to improved chances of survival [16-19].
Conclusion
Further research studies are required to enhance more knowledge based on multilocular radiolucencies. Immunohistochemically studies help us to know the nature of the lesion and also to differentiate the same from other cysts of odontogenic origin. Hence, it is essential that studies should be conducted on a large scale in order for us to ascertain the origin and nature of the lesion. Radiographic imaging may not provide a specific diagnosis, however, it assists in narrowing the differential diagnosis, thereby helping to guide patient treatment. In conclusion, we would aim to achieve precise and accurate radiograph results in order for us to understand the prevalence of multilocular radiolucencies.
Acknowledgement
The authors sincerely acknowledge the faculty, Medical record and information technology department of SIMATS for their tireless help in sorting out data pertinent to this study.
Authors Contributions
• Sivaharini S: Literature search, data collection, data analysis, manuscript writing.
• Dr. Sneha: study design, data verification, manuscript drafting.
Conflict of Interest
The authors declare that there were no conflicts of interest in the present study.
References
- Johnson NR, Gannon OM, Savage NW, Batstone MD. Frequency of odontogenic cysts and tumors: a systematic review. J Investig Clin Dent. 2014;5:9-14. [Crossref] [Google Scholar] [PubMed]
- Kaneda T, Minami M, Kurabayashi T. Benign odontogenic tumors of the mandible and maxilla. Neuroimaging Clin N Am. 2003;13:495-507. [Crossref] [Google Scholar] [PubMed]
- Borghesi A, Nardi C, Giannitto C, Tironi A, Maroldi R, Bartolomeo FD. Odontogenic keratocyst: imaging features of a benign lesion with an aggressive behavior. Insights Imaging. 2018;9:883-897. [Crossref] [Google Scholar] [PubMed]
- Antonoglou GN, Sandor GK, Koidou VP, Papageorgiou SN. Non-syndromic and syndromic keratocystic odontogenic tumors: Systematic review and meta-analysis of recurrences. J Craniomaxillofac Surg. 2014;42:364-371. [Crossref] [Google Scholar] [PubMed]
- Givol N, Buchner A, Taicher S, Kaffe I. Radiological features of osteogenic sarcoma of the jaws. A comparative study of different radiographic modalities. Dentomaxillofac Radiol. 1998;27:313-320. [Crossref] [Google Scholar] [PubMed]
- Harmon M, Arrigan M, Toner M, O’Keeffe SA. A radiological approach to benign and malignant lesions of the mandible. Clin Radiol. 2015; 70:335-350. [Crossref] [Google Scholar] [PubMed]
- Kim SG, Jang HS. Ameloblastoma: a clinical, radiographic, and histopathologic analysis of 71 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 91:649-653. [Crossref] [Google Scholar] [PubMed]
- More C, Tailor M, Patel HJ, Asrani M, Thakkar K, Adalja C. Radiographic analysis of ameloblastoma: a retrospective study. Indian J Dent Res. 2012;23:698. [Crossref] [Google Scholar] [PubMed]
- Murphey MD, Nomikos GC, Flemming DJ, Gannon FH, Temple HT, Kransdorf MJ. From the archives of AFIP. Imaging of giant cell tumor and giant cell reparative granuloma of bone: Radiologic-pathologic correlation. Radiographics. 2001;21:1283-309. [Crossref] [Google Scholar] [PubMed]
- Ji YD, Keith DA. Clinical Trials of Rare Benign Pathologies in Oral and Maxillofacial Surgery. J Oral Maxillofac Surg. 2020;78:866-899. [Crossref] [Google Scholar] [PubMed]
- Katz JO, Underhill TE. Multilocular radiolucencies. Dent Clin North Am. 1994;38:63-81. [Crossref] [Google Scholar] [PubMed]
- Chi AC, Neville BW, Klinger BJ. A multilocular radiolucency. Botryoid odontogenic cyst. J Am Dent Assoc. 2007;138:1102-1103. [Crossref] [Google Scholar] [PubMed]
- Bonanthaya K, Panneerselvam E, Manuel S, Kumar VV, Rai A. Oral and maxillofacial surgery for the clinician. 1st ed, Springer Singapore, Gateway East Singapore 189721. Singapore. 2021;1-2008. [Google Scholar]
- Rajendran R. Shafer’S Textbook of oral pathology. 6th ed, Elsevier, India. 2009;1-963. [Google Scholar]
- Gundlach Kkh. Peter A Reichart, Hans P Philipsen: Odontogenic tumors and allied lesions. Mund Kiefer GesichtsChir. 2005;9:263-263. [Google Scholar]
- Pindborg JJ. Histological typing of odontogenic tumours, jaw cysts, and allied lesions. Inter his classify tumor. 1971;1-44. [Google Scholar]
- Stoopler ET, Vogl DT, Alawi F, Greenberg MS, Sollecito TP, Salazar G, et al. The presence of amyloid in abdominal and oral mucosal tissues in patients initially diagnosed with multiple myeloma: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:326-332. [Crossref] [Google Scholar] [PubMed]
- Harousseau JL, Minvielle S, Bataille R. Oncogenesis of multiple myeloma: 14q32 and 13q chromosomal abnormalities are not randomly distributed, but correlate with natural history, immunological features, and clinical presentation. Blood. 2002;99:2185-2191. [Crossref] [Google Scholar] [PubMed]
- Daley TD, Wysocki GP, Pringle GA. Relative incidence of odontogenic tumors and oral and jaw cysts in a Canadian population. Oral Surg Oral Med Oral Pathol. 1994; 77:276-280. [Crossref] [Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.