Prevalence of Palmar Hyperhidrosis Affecting Clinical Efficacy in Medical Professionals
Received: 19-Dec-2022, Manuscript No. AMHSR-23-84187; Editor assigned: 21-Dec-2022, Pre QC No. AMHSR-23-84187 (PQ); Reviewed: 04-Jan-2023 QC No. AMHSR-23-84187; Revised: 20-Feb-2023, Manuscript No. AMHSR-23-84187 (R); Published: 27-Feb-2023
Citation: Sanghavi PJ, et al.. Prevalence of Palmar Hyperhidrosis Affecting Clinical Efficacy in Medical Professionals. Ann Med Health Sci Res. 2023;13:558-561.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Hyperhidrosis, meaning excessive sweating, can be described as perspiration in excess of the physiologic amount necessary to maintain the thermal homeostasis. It is thought to be the result of eccrine sweat glands by the cholinergic sympathetic ibers which innervate them. Many of medical professionals such as physiotherapists, dentists, and nurses, may suffer from palmar hyperhidrosis, due to which their clinical efficacy may get affected to some considerable extent. Their efficacy of treating the patients manually, handling tools, injecting needles, dressing wounds, and grasping the surgical instruments, are all hampered due to excessive sweating. The main goal of the study was to determine the prevalence of palmar hyperhidrosis affecting the clinical efficacy of medical professionals. The objective was to assess the extent of palmar hyperhidrosis affecting clinical efficacy.
Method: A total of forty (40) medical professionals with palmar hyperhidrosis voluntarily participated in the study. The clinical efficacy was assessed by using hyperhidrosis questionnaire.
Results: Based on the statistical analysis, among the total population taken, the prevalence of palmar hyperhidrosis affecting clinical efficacy in medical professionals was considered extremely signi icant (p<0.0001). Overall, 45.56% of the clinical efficacy was seen to be reduced or affected due to palmar hyperhidrosis.
Conclusion: The overall study indicates that the clinical efficacy of medical professionals due to palmar hyperhidrosis is reduced to a considerable extent in the age group of 20-30 years. Also, the quality of life of the subjects was found to be reduced signi icantly. Hence, the prevalence of palmar hyperhidrosis affecting clinical efficacy in medical professionals is significant.
Keywords
Palmar hyperhidrosis; Clinical efficacy; Medical professionals; Quality of life
Introduction
Hyperhidrosis is generally defined as over activity of the eccrine sweat glands that results in excessive, bilateral, relatively symmetric sweating beyond the amount necessary to maintain a body temperature within normal limits. Sweat is primarily produced by the eccrine sweat glands. It leads to the dissipation of heat through evaporation. The human body consists of 2 to 4 million eccrine sweat glands. Human eccrine sweat glands have 2 distinct functions they allow body cooling by evaporation and also moisten the skin on the palms and soles at times of activity to improve their grip. Histologic evaluation of eccrine sweat glands shows normal appearing glands with a normal size, number and density. Sweating is a reflex function which is primarily controlled by the sympathetic nervous system. These nerves are anatomically sympathetic but functionally cholinergic i.e. acetylcholine is the principles terminal neurotransmitter rather than norepinephrine. Neural impulses for sweating travel from the anterior hypothalamus via the reticulospinal tracts to the appropriate level in the spinal cord, out through the rami communicates to autonomic ganglia, and then within sympathetic cholinergic neurons to the secretory cells of the eccrine glands. The most widely used classification system divides hyperhidrosis into primary and secondary types. Primary hyperhidrosis is the most common type. The highest prevalence rates of primary hyperhidrosis are among the ages of 18 to 54 years. A positive family history contributing to primary hyperhidrosis has been seen in 30% to 65% of patients. It is defined as excessive sweating in localized areas such as the armpits, face, soles, and palms which may be genetic or is not associated with a systemic disorder. The onset is most common in the age of 14 to 25 years. Men and women of all races are equally affected. Palmar hyperhidrosis is the most common form of primary hyperhidrosis. It is seen both in cold and warm environments, but is more problematic in hot weather. Secondary hyperhidrosis is caused due to some drugs, infection, malignancy, anxiety or endocrine disorders such as diabetes, and hyperthyroidism. It may be localized or generalized. Hyperhidrosis affects about 3% of the population. Primary hyperhidrosis becomes symptomatic in childhood itself, usually around puberty. The degree of severity of palmar hyperhidrosis ranges between moderate moisture to severe dripping. Also, it aggravates during the stress and anxiety periods. Daily social and occupational activities of an individual are hampered due to hyperhidrosis. Thus, hyperhidrosis has an impact on the quality of life of an individual. Many of medical professionals such as physiotherapists, nurses, and dentists, may suffer from hyperhidrosis, due to which their clinical efficacy gets affected to some extent. Their efficacy of treating the patient manually, handling tools, injecting needles, and grasping the surgical instruments, are all hampered due to excessive sweating. Hyperhidrosis has more reduction in the quality of life than that caused by other dermatologic diseases such as atopic dermatitis, contact dermatitis, and psoriasis. Palmar hyperhidrosis impacts the patient’s quality of life leading them to adapt their behaviour to fit in with their condition. The first step in the diagnosis of hyperhidrosis is to differentiate between primary and secondary hyperhidrosis. History should be taken regarding the location of hyperhidrosis, duration and specific triggers. Medical disorders and medications should be documented. Measurement of sweat can be performed. A grading scale for volar disease lists “low” as a moist palm without visible sweat droplets. “Moderate” disease is characterized by sweating towards the fingertips. “Severe” cases drip sweat. Thoracic sympathectomy has been recognized as the life. A simple test, called Minor’s starch-iodine test, is a tool that demonstrates the sweating pattern and reveals the location of the most active sweat glands in a given area. In order to document amounts of sweat produced, gravimetric (via weighing filter paper before and after application to the skin) and evaporative (via a device that assesses water vapour loss from the skin) measurements can be made at volar sites. Various treatments to control hyperhidrosis have been reported, which include topical therapy anticholinergics, iontophoresis, botulinum toxin and surgery. In a small number of cases, psychotherapy has been proven beneficial. Various studies have demonstrated iontophoresis efficacy in the treatment of hyperhidrosis. In iontophoresis, an electromotive force is used which enhances percutaneous absorption of a drug or chemical in form of ions on the skin. Each of the treatment options has its advantages, disadvantages, and side effects. It is essential to provide the patient with precise information regarding the efficacy, complications, and adverse effects of each treatment modality before starting any therapy [1-5].
Materials and Methods
An ethical clearance certificate was obtained by the institutional ethical committee of krishna institute of medical sciences deemed to be university, Karad. This study was conducted at Karad. Subjects from Krishna institute of medical sciences deemed to be university, Karad, were included. Medical professionals who experience hyperhidrosis during their clinical practices were selected. Subjects were chosen by random sampling method according to the inclusion and exclusion criteria. Informed written consent was obtained from the subjects. The procedure was explained to the participants. The subjects were asked to fill out the provided questionnaire on their smartphones. Statistical analysis of collected data was done accordingly and hence conclusion was given. This was an observational study conducted among 40 participants, aged between 20 and 30 years. The study was done from January 2022 to June 2022. The selection of participants was done using the random sampling method. Both males and females were included. The participants were considered according to the inclusion and exclusion criteria. The total sample size was 60 but we got 40 samples due to time limitations.
Inclusion criteria
Symptomatic subjects i.e. participants with palmar hyperhidrosis were included in this study. Participants within 20-30 years of age were taken, including both males and females. Only medical professionals (physiotherapists, nurses, dentists) from Krishna institute of medical sciences, deemed to be university were included. Participants who were willing to participate were chosen.
Exclusion criteria
Asymptomatic medical professionals were excluded. Participants with hyperhidrosis at sites other than palms were excluded. Participants with skin conditions other than palmar hyperhidrosis were also excluded. Participants who were not willing to participate were excluded.
Materials used were Google forms and data collection sheets
Procedure: This is a study of prevalence of palmar hyperhidrosis affecting clinical efficacy in medical professionals. This study was conducted at Karad. An ethical clearance certificate was obtained by institutional ethical committee of Krishna institute of medical sciences deemed to be university, Karad. Subjects from Krishna institute of medical sciences deemed to be university, Karad, were included. Medical professionals who experience hyperhidrosis during their clinical practices were selected. Subjects were chosen by random sampling method according to the inclusion and exclusion criteria. An informed written consent was obtained from subjects. The procedure was explained to the participants. The subjects were asked to fill the provided questionnaire on their smart phones. Statistical analysis of collected data was done accordingly and hence conclusion was given [6-10].
Outcome measures: Hyperhidrosis questionnaire.
Results
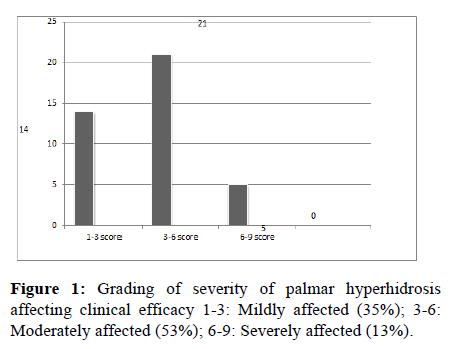
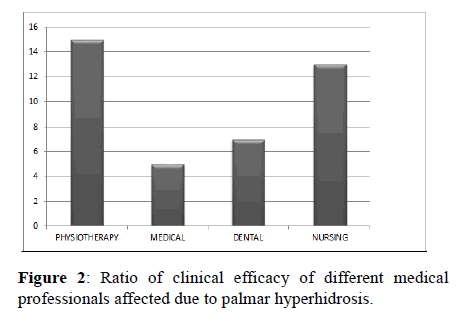
Among the 40 subjects, 13% of the subject’s clinical efficacy was severely affected, 53% was affected moderately, and 35% of the subject’s efficacy was mildly affected. According to the study, 55.1% of hyperhidrosis increased during stressful conditions. The present study was conducted at a single institution; therefore generalization of the study may be limited (Figure 1 and Table 1). Another limitation of the study was the lesser number of sample size. Overall, 45.56% of the clinical efficacy was seen to be reduced or affected due to palmar hyperhidrosis (Figure 2).
| S. no. | Gender | 1-3 score | 3-6 score | 6-9 score | Mean | SD | P value |
|---|---|---|---|---|---|---|---|
| 1 | Male | 3 | 6 | 1 | 4.238 | 1.662 | <0.0001 |
| 2 | Female | 11 | 15 | 4 |
Table 1: Ratio of males is to females whose clinical efficacy is affected.
Discussion
In this study, the majority of the subjects are between 20 and 30 years. Hyperhidrosis is found to be more in females than in males. In this study, only subjects or medical professionals with symptoms of hyperhidrosis were included. Also, only the palmar aspect of the body affected by hyperhidrosis was taken into consideration. This study included about 40 medical professionals from medical, dental, physiotherapy and nursing specifically only from Krishna institute of medical sciences deemed to be university, Karad. Among them, 30 were females and 10 were males. The study was carried out using a hyperhidrosis questionnaire. The questionnaire included 11 questions regarding the effects of palmar hyperhidrosis on clinical efficacy were included. The questions included were such as the severity of hyperhidrosis, its effect on the clinical efficacy, its effect on confidence levels, and discomfort during attending the patients, etc. The subjects were asked to fill out the hyperhidrosis questionnaire form that was forwarded to them. In this study, many of the subjects were aware of the causes but some were not. The previous study was done in Rio de Janeiro, where a sample of 900 medical students was taken. Demographic data including gender, ethnicity, age, height and weight were collected. Prevalence was done based on the questionnaires which inquired about the presence of palmar hyperhidrosis along with its characteristics. The Hyperhidrosis Disease Severity Scale (HDSS) was used to evaluate the severity of hyperhidrosis. Out of 900 subjects, the prevalence of palmar hyperhidrosis among medical students was about 20.56%. It was similar between men and women and was mostly associated with a family history of the disease. Among the total population of hyperhidrosis, 63.78% were axillary, 50.81% palmar, 20.54% craniofacial, 18.38% face flushing, and 2.16% gustatory sweating. The mean current age for palmar hyperhidrosis patients was about 2.11% (± 4.04) [11-13].
Conclusion
• The overall study indicates that the clinical efficacy of
medical professionals due to palmar hyperhidrosis is
reduced to considerable extent in the age group of 20-30
years.
• Also, the quality of life of the subjects was found to be
reduced significantly.
• Hence, it is significant that the clinical efficacy of the
medical professionals is reduced due to palmar
hyperhidrosis.
Limitations
• Poor geographical area (restricted to KIMS).
• Inadequate time for study.
• Population restricted (medical professionals).
• Since the study size was small, results cannot be
generalized for the entire population.
• Only palmar aspect was considered for hyperhidrosis.
References
- Kamudoni P, Mueller B, Halford J, Schouveller A, Stacey B, et al. The impact of hyperhidrosis on patients' daily life and quality of life: A qualitative investigation. Health Qual Life Outcomes. 2017;15:121.
[Crossref] [Google Scholar] [PubMed]
- Westphal FL, de Carvalho MAN, de Carvalho BCN, Padilla R, Araujo KKL. Prevalence of hyperhidrosis among medical students. Rev Col Bras Cir. 2017;29:728-734.
[Crossref] [Google Scholar] [PubMed]
- Kim DH, Kim TH, Lee SL, Lee AI. Treatment of palmar hyperhidrosis with tap water iontophoresis: A randomized, sham-controlled, single-blind, and parallel-designed clinical trial. Ann Dermatol. 2017;29:728-734.
- Kyung MR, Cantor RM, Lange KL, Ahn SS. Palmar hyperhidrosis: Evidence of genetic transmission. J Vasc Surg. 2002;35:382-386.
[Crossref] [Google Scholar] [PubMed]
- Griffiths C, Barker J, Bleaker T, Chalmers R, Creamer D. Rook’s Textbook of Dermatology. 9th ed. Wiley Publishing Company. New York, United States. 2013.4432.
- Solish N, Benohanian A, Kowalski JW. Prospective open-label study of botulinum toxin type a in patients with axillary hyperhidrosis: Effects on functional impairment and quality of life. Dermatol Surg. 2005;31:405-413.
[Crossref] [Google Scholar] [PubMed]
- Fujimoto T, Kawahara K, Yokozeki H. Epidemiological study and considerations of primary focal hyperhidrosis in Japan: From questionnaire analysis. J Dermatol. 2013;40:886-990.
[Crossref] [Google Scholar] [PubMed]
- Lima So, Aragao Jf, Machado NJ, Almeida Kb, Menezes Lm, et al. Research of primary hyperhidrosis in students of medicine of the state of sergipe, Brazil. An Bras Dermatol. 2015;90:661-665.
[Crossref] [Google Scholar] [PubMed]
- Young O, Neary P, Keaveny Tv, Mehigan D, Sheehan S. Evaluation of the impact of transthoracic endoscopic sympathectomy on patients with palmar hyperhydrosis. Eur J Vascendovasc Surg. 2003;26:673-676.
[Crossref] [Google Scholar] [PubMed]
- Morard MRS, Martins RB, Ribeiro ACL, Lima PGR, Carvalho BDS, et al. Primary hyperhidrosis prevalence and characteristics among medical students in Rio de Janeiro. PLoS One. 2019; 14:0220664
[Crossref] [Google Scholar] [PubMed]
- Lear W, Kessler E, Solish N, Glaser DA. An epidemiological study of hyperhidrosis. Dermatol Surg. 2007;33:69-75.
[Crossref] [Google Scholar] [PubMed]
- Connolly M, de Berker D. Management of primary hyperhidrosis: A summary of the different treatment modalities. Am J Clin Dermatol. 2003;4:681-697.
[Crossref] [Google Scholar] [PubMed]
- Sultan AA, Kaliyadan F, Aldhafiri M. The impact of primary hyperhidrosis on quality of life among residents in Al-Ahsa City, Saudi Arabia. J Pharm Negat. 2022; 13:670-677.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.