Pustulovesicular Skin Eruption as Presenting Feature of Incomplete Kawasaki Disease
- *Corresponding Author:
- Goyal JP
Department of Pediatrics, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, Gujarat, India
E-mail: gkathir72@gmail.com
This is an open access article distributed under the terms of the Creative Commons AttributionNon CommercialShare Alike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
A 12-year-old female was referred with a history of fever and abdominal pain for 10 days and swelling all over her body for 4 days. Swelling developed initially over her left leg and arm followed by the right extremities, later involving the entire body. She also gave a history of passage of red-colored urine for 1 day. On general physical examination, she was febrile (temperature −102°F) with mild pallor and erythema over the lips. Her blood pressure was normal and there was no lymphadenopathy. On abdominal examination, mild ascites and tenderness were present
Dear Sir,
A 12-year-old female was referred with a history of fever and abdominal pain for 10 days and swelling all over her body for 4 days. Swelling developed initially over her left leg and arm followed by the right extremities, later involving the entire body. She also gave a history of passage of red-colored urine for 1 day. On general physical examination, she was febrile (temperature −102°F) with mild pallor and erythema over the lips. Her blood pressure was normal and there was no lymphadenopathy. On abdominal examination, mild ascites and tenderness were present. She had pustulovesicular lesions all over the right forearm [Figure 1] and right knee joint along with erythematous skin rash over her buttock and back. The rest of her systemic examination was normal. Investigations are tabulated in Table 1.
| Laboratory parameters | Result | Reference normal range |
|---|---|---|
| Hemoglobin (g/dL) | 7.8 | 11.5-15.5 |
| WBC count (×103/µL) | 15.4 | 5-14.5 |
| Platelets (×103/µL) | 821 | 150-450 |
| Erythrocyte sedimentation | 62 | 3-13 |
| rate (mm/h) | ||
| Peripheral smear for | Not detected | - |
| malaria parasite | ||
| Urine analysis | 10-15 WBC/HPF | 0-4/HPF |
| Urine culture and sensitivity | Sterile | - |
| Blood culture and | Sterile | - |
| sensitivity | ||
| Culture of aspirated fluid | Sterile | - |
| from skin lesion | ||
| Urea (mg/dL) | 33 | 20-40 |
| Creatinine (mg/dL) | 0.9 | 0.12-1.06 |
| Sodium (mEq/L) | 114 | 136-145 |
| Potassium (mEq/L) | 4.4 | 3.5-5.5 |
| ALT (units/L) | 101 | 10-55 |
| Aspartate aminotransferase | 194 | 15-40 |
| (units/L) | ||
| Bilirubin (mg/dL) | 0.8 | 0.2-1.00 |
| Albumin (g/dL) | 1.9 | 3.7-5.5 |
| Globulin (g/dL) | 2.9 | 2.3-5.5 |
| Alkaline | 54 | 200-495 |
| phosphatase (unit/L) | ||
| Prothrombin time (s) | 40 | 12.2-15.5 |
| C-reactive protein (mg/dL) | 363 | <10 |
| Creatine kinase (unit/L) | 3615 | 60-330 |
| Direct comb test | Negative | - |
| Antinuclear antibody | Negative | - |
| Antistreptolysin O titer (IU) | <200 | <200 |
| Rheumatoid factor | 10 | <15 |
| (units/mL) | ||
| TORCH serology | Negative | - |
| IgM serology for dengue, | Negative | - |
| typhoid, and leptospirosis | ||
| USG abdomen | Gaseous distension | - |
| with free fluid in | ||
| pelvic cavity | ||
| Doppler study of lower limb | Normal | - |
| ECG | Nonspecific ST-T | - |
| changes | ||
| 2D echocardiogram | Normal |
Table 1: Laboratory parameters of index case at the time of presentation
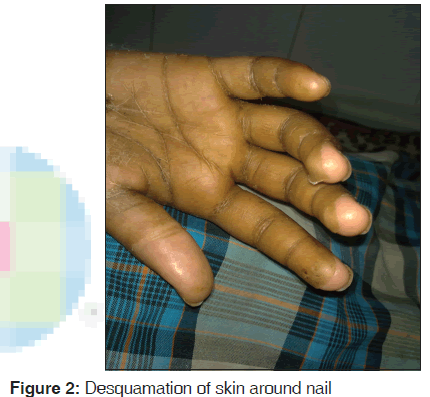
The patient was managed conservatively with 3% saline to correct her hyponatremia. Vitamin K and fresh frozen plasma were given for deranged coagulation profile and intravenous antibiotics for high white cell count. Although her electrolytes and prothrombin time showed improvement, her fever did not subside. She developed desquamation of skin around nails after 10 days of admission [Figure 2].
Initially, administration of intravenous immunoglobulin was planned; however, due to financial constraints, she was treated with oral prednisolone 2 mg/kg/day for a week which was tapered subsequently. Aspirin was added as an anti-inflammatory. Her fever subsided, swelling on the extremities reduced, and C-reactive protein (CRP) normalized within a week. The patient was discharged on low-dose aspirin and advised to repeat two-dimensional (2D) echo in 6-week time. After being discharged, she developed Beau’s line within 15 days [Figure 3]. Her repeat 2D echo was normal at 6 weeks.
The usual skin rash in Kawasaki disease (KD) is an erythematous maculopapular lesion which is nonbullous and nonvesicular. [1,2] Less common are other types of skin rashes such as scarlatiniform, psoriatic, hyperkeratotic, and pustular lesion, which have been reported in literature. [3-7] A patient who does not fulfill the criteria for KD should be diagnosed as having incomplete KD. [8]
We report an interesting case of incomplete KD with unusual pustulovesicular skin lesions. Although pustular skin lesions have been reported occasionally in literature, [6,7] concomitant vesicular lesions are very rare. Till date, only one case of KD with pustulovesicular lesion has been reported in literature to the best of our knowledge. [9]
In our case, persistence of fever for more than 5 days and presence of three clinical criteria (changes in extremities, polymorphous exanthema, and changes in oral cavity), elevated CRP and erythrocyte sedimentation rate (ESR), along with the presence of more than three supplementary criteria (albumin ≤3 g/dl, anemia for age, elevated alanine aminotransferase, platelets ≥450 × 103 µL after 7 days, white blood cells ≥15 × 103 µL, and urine ≥10 white cells/high power field) helped in diagnosing the patient with incomplete KD. [1]
KD should be differentiated from scarlet fever, toxic shock syndrome, measles, adenovirus infections, drug hypersensitivity reactions, and leptospirosis. Measles infection is associated with exudative conjunctivitis and maculopapular rash that begins on the face behind the ear, leukopenia, and normal CRP/ESR. Adenovirus infection is associated with exudative pharyngitis and conjunctivitis. All these findings were absent in our patient. Herpes, cytomegalovirus, varicella, and Epstein–Barr virus infection may sometime also mimic KD. The diagnosis of viral infections was excluded by negative serology. Moreover, typical changes in the extremities in our case which suggest KD is usually absent in these viral infections. In case of drug reaction, there are periorbital edema, oral ulceration, and a normal or minimally elevated ESR which help in distinguishing it from KD. The absence of hypotension and renal involvement in our case clinically helped us to differentiate it from toxic shock syndrome. Scarlet fever was excluded based on typical clinical features at presentation and negative blood culture. [10]
Corticosteroid was given based on observations by Nonaka et al. [11] and Shinohara et al. [12] They found shorter fever duration in the steroid group in comparison to control, but no statistically significant difference in the prevalence of coronary aneurysm.
This case highlights the association of incomplete KD with pustulovesicular lesion. The probability of KD should be kept in mind as a differential diagnosis in patients presenting with fever and pustulovesicular skin lesions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: A statement for health professionals from the Committee on rheumatic fever, endocarditis, and Kawasaki disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 2004;114:1708-33.
- Burns JC, Glodé MP. Kawasaki syndrome. Lancet 2004;364:533-44.
- Boralevi F, Barat P, Lepreux S, Stockman AL, Taïeb A, Léauté-Labrèze C. Kawasaki’s disease with eruptive pustular and guttate psoriasis. Ann Dermatol Venereol 2003;130:528-31.
- Zvulunov A, Greenberg D, Cagnano E, Einhorn M. Development of psoriatic lesions during acute and convalescent phases of Kawasaki disease. J Paediatr Child Health 2003;39:229-31.
- Mizuno Y, Suga Y, Muramatsu S, Hasegawa T, Ogawa H. Psoriasiform and palmoplanter pustular lesions induced after Kawasaki disease. Int J Dermatol 2006;45:1080-2.
- Ulloa-Gutierrez R, Acón-Rojas F, Camacho-Badilla K, Soriano-Fallas A. Pustular rash in Kawasaki syndrome.Pediatr Infect Dis J 2007;26:1163-5.
- Kimura T, Miyazawa H, Watanabe K, Moriya T. Small pustules in Kawasaki disease. A clinicopathological study of four patients. Am J Dermatopathol 1988;10:218-23.
- Sundel RP, Petty RE. Kawasaki disease. In: Cassidy JT, Petty RE, Laxer RM, Lindsley CB, editors. Textbook of Pediatric Rheumatology. 5th ed.. Philadelphia: Elsevier Saunders; 2005. p. 521-38.
- Kwan YW, Leung CW. Pustulo-vesicular skin eruption in a child with probable Kawasaki disease. Eur J Pediatr 2005;164:770-1.
- Rowley AH, Shulman ST. Kawasaki disease. In: Kliengman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson Textbook of Pediatrics. 18th ed. Philadelphia, PA: W.B. Saunders; 2008. p. 1036-42.
- Nonaka Z, Maekawa K, Okabe T, Eto Y, Kubo M. Randomized controlled study of intravenous prednisolone and gamma globulin treatment in 100 cases with Kawasaki disease. In: Kato H, editor. Kawasaki Disease: Proceedings of the 5th International Kawasaki Disease Symposium, Fukuoka,Japan, May 22-25, 1995. New York: Elsevier Science; 1995. p. 328-31.
- Shinohara M, Sone K, Tomomasa T, Morikawa A. Corticosteroids in the treatment of the acute phase of Kawasaki disease. J Pediatr 1999;135:465-9.






 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.