Radiological Assessment of Postoperative Changes Following Lapidus Procedure for the Treatment of Hallux Valgus
Citation: Almaawi A, et al. Radiological Assessment of Postoperative Changes Following Lapidus Procedure for the Treatment of Hallux Valgus . Ann Med Health Sci Res. 2021;11:1378-1384.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Context: Hallux valgus is considered the most common pathological cause of pain among adults. There are multiple surgical approaches for its treatment, Therefore, to know the effectiveness of each technique in accordance to our population, they have to be analysed. Aims: The aim of this study was to radiologically assess postoperative changes after the Lapidus procedure from weight-bearing anteroposterior and lateral radiographs. Settings & Design: To analyze the effectiveness of the Lapidus procedure in our setting, we will use a retrospective cohort design to collect the data. Outcomes are defined as reduced calculated angles on radiograph images in King Saud University Medical City. Methods & Material: Data of all patients who underwent a modified Lapidus procedure between 2015 and 2019 were collected from multiple centers. All angles (hallux valgus angle, intermetatarsal angle, calcaneal pitch angle, Meary’s angle, and tibial sesamoid position) were measured both preoperatively and postoperatively. Statistical Analysis Used: Data will be analyzed according to appropriate statistical methods via Statistical Package for Social Studies (SPSS 22; IBM Corp., New York, NY, USA). Results: A total of 100 Lapidus procedures in 89 patients were reviewed. There were 78 unilateral procedures and 11 bilateral procedures with a mean follow-up period of 2 years. The mean hallux valgus correction angle between the preoperative and postoperative follow-up radiographs was 21.7° (p<0.001). The average decrease in the intermetatarsal angle was 7.5° (p<0.001; 95% confidence interval (CI), (6.8–8.3)). The correction angle Meary’s angle mean was 0.2 (p<0.721; CI, (-1.3–0.9)). The average increase in the calcaneal pitch angle was 3.8° (p<.001). The average decrease in the LaPorta classification was 2.9 units (p<.001; CI, (2.6–3.3)). Postoperatively, no patients were in the LaPorta group 6 or 7. Conclusion: In the Lapidus procedure, the first tarsometatarsal joint derotational arthrodesis produced good radiologic correction on flexible Hallux Valgus. In addition, the LaPorta classification showed a significant decrease and proper positioning of sesamoids postoperatively, which is a predictor for good results and a decrease in recurrence.
Keywords
Hallux valgus; Lapidus procedure; Foot and ankle; First tarsometatarsal joint derotational arthrodesis; Chevron osteotomy; Orthopedic surgery
Introduction
Hallux valgus is one of the most frequent deformities affecting the forefoot. [1-4] It usually presents as an irreversible abnormality, [5-7] where the 1st metatarsal bone is shifted medially or adducted and the phalanx is shifted laterally or abducted, [8-11] Such a deformity can affect the alignment of the 1st metatarsophalangeal joint (metatarsophalangeal joint) and attenuation of the medial collateral and the medial capsule along with the plantar flexor, leading to translation of the sesamoid bones, laxity, hypermobility, and instability; eventually, it might disrupt the gait when severe. [3,10,12,13]
The overall prevalence of hallux valgus in Saudi Arabia was 43%; the prevalence of hallux valgus in men and women was 30.7% and 49.2%, respectively. [14] In another study on 100 female participants, it was found that 39% of patients not only had hallux valgus but also had bilateral hallux valgus. [15]
In hallux valgus, the pain has been found to be linked to and located at the forefoot, with a higher incidence rate in females than in males. Pain affects lifestyle and daily activities. It was also noted that severe hallux valgus could lead to a high chance of falling due to changes in gait biomechanics. [3,9,16-21]
Multiple risk factors have been associated with hallux valgus. Pes planus has been found to be the most important risk factor [22,23] wherein there is an increase in the pressure over the medial plantar side of the first ray, which also contributes to a decrease in the range of motion of the metatarsophalangeal joint. [24] Additionally, shoe wear, [25] particularly high heels, which increases the load over the 1st metatarsal bones, increases the load on the forefoot by 30%–47% depending on the heel height. [26-30] Hallux valgus occurs at higher rates among the elderly population. [8,18,31,32] Moreover, many risk factors have also been linked to hallux valgus, such as family history, genetics, ligaments laxity [33-35] and Body Mass Index (BMI). [17,36]
A variety of procedures have been recommended, one of which is the Lapidus procedure. The Lapidus procedure is mainly indicated for moderate to severe hallux valgus with first meta tarsophalgeal joint subluxation, hypermobility of the first tarsometatarsal joint, or ligamentous laxity, as well as in the treatment of recurrent hallux valgus. This procedure aims to correct the position and rotation of the 1st metatarsal. This can be achieved by reducing the intermetatarsal angle, which alters and changes the rotation and position of the metatarsals, [37,38] including the correction of the sesamoid complex. The relocation of the 1st metatarsal over the sesamoid bones with frontal plane rotation is an important factor in the success of the procedure. [39]
The purpose of our study was to review the radiographic changes in the foot after undergoing the Lapidus procedure.
Patients and Methods
This was a retrospective observational study on the radiological review of patients who underwent the Lapidus procedure between 2015 and 2019. The inclusion criterion was all patients who underwent the Lapidus procedure during the inclusion time regardless of their age, sex, and comorbidities; these characteristics shown in Table 1. Our exclusion criteria were any patient who previously underwent any hallux valgus procedure, those with a restriction of range of motion of the 1st metatarsophalangeal joint, and those with any signs that indicated degenerative changes. All data were extracted from the electronic databases of the King Saud University Medical City (KSUMC), Specialized Medical Center (SMC) and Dallah Hospital’s, Dr. Sulaiman Alhabib Medical Center. Radiologic measurements were obtained from different imaging systems: Centricity™ in King Saud University Medical City (KSUMC), Sectra™ in Dallah Hospital, Isite™ in Specialized Medical Center (SMC), and PACs™ in Dr. Sulaiman Al Habib Medical Center.This was a retrospective observational study on the radiological review of patients who underwent the Lapidus procedure between 2015 and 2019. The inclusion criterion was all patients who underwent the Lapidus procedure during the inclusion time regardless of their age, sex, and comorbidities; these characteristics shown in Table 1. Our exclusion criteria were any patient who previously underwent any hallux valgus procedure, those with a restriction of range of motion of the 1st metatarsophalangeal joint, and those with any signs that indicated degenerative changes. All data were extracted from the electronic databases of the King Saud University Medical City (KSUMC), Specialized Medical Center (SMC) and Dallah Hospital’s, Dr. Sulaiman Alhabib Medical Center. Radiologic measurements were obtained from different imaging systems: Centricity™ in King Saud University Medical City (KSUMC), Sectra™ in Dallah Hospital, Isite™ in Specialized Medical Center (SMC), and PACs™ in Dr. Sulaiman Al Habib Medical Center.
| Variable | Category | % |
|---|---|---|
| Side | Left | 43 |
| Right | 57 | |
| Gender | Male | 7 |
| Female | 93 | |
| Smoker | No | 100 |
| Yes | 0 | |
| Diabetes | No | 92 |
| Yes | 8 |
Table 1: Baseline characteristics of respondents.
IRB approval was provided by the Institutional Review Board (IRB) at KSUMC, and the patients’ consent was waived as per our IRB regulations for retrospective studies.
The diagnosis and classification of hallux valgus and its severity rely on angular measurement from anteroposterior and lateral weight-bearing radiographs. [40] The severity of hallux valgus can be determined by the hallux valgus angle, which is the angle created by a line that bisects the 1st hallux and another line that bisects the 1st metatarsal. [41] In addition, the intermetatarsal angle, which is an angle created by the 1st and 2nd metatarsal, indicts a widening between the 1st and 2nd metatarsal bones. [42] A severe hallux valgus deformity is when the hallux valgus angle is greater than 40° and the intermetatarsal angle is greater than 16°. [43]
The hallux valgus angle and intermetatarsal angle were measured from the standing foot anteroposterior images. The calcaneal pitch angle and Meary’s angle (angle between the longitudinal axes of the talus and the 1st metatarsal) were measured from the lateral weight-bearing images. The tibial sesamoid position relative to the 1st metatarsal bisector was assessed from a standing foot anteroposterior X-ray through the LaPorta classification, ranging from grade 1 (normal position) to grade 7 (most laterally translocated). [44]
All measurements and data collection were performed in accordance with the guidelines of the American Orthopedic Foot and Ankle Society Ad Hoc Committee on Angular Measurements reference. Of a total of 100 procedures, 93 procedures were performed in female patients (93%) and 7 were in males (7%). Our patients had a mean age of 40.7 years. All demographic data of the patients are included in Table 1.
Lapidus procedures were performed by three surgeons working simultaneously at these institutes. All surgeons had undergone foot and ankle fellowship training in North America and similarly performed the procedure. The Lapidus procedure was performed by fusing the 1st tarsometatarsal joint while correcting the intermetatarsal angle. Under fluoroscopy guidance, the 1st metatarsal head is restored back onto the sesamoids, and the hallux is derotated and straightened, with attenuation of the medial joint capsule along with modified McBride procedure. [45]
The analysis was performed using Statistical Package for Social Sciences version 22.0 software (SPSS Inc., Chicago, IL, USA). Categorical data were expressed using frequency and percentage. Chi-square and Fischer’s exact tests were used to compare the categorical data for the two groups. We assumed statistical significance when the p-value was less than 0.05.
Results
In this study, we reviewed 100 laparoscopic procedures in 89 patients. Among the participants, there were 78 unilateral procedures and 11 bilateral procedures with a two-year mean follow-up period [Table 1 and Table 2].
| Parameter | Preoperative | Postoperative | Mean difference (95% CI) |
P-value |
|---|---|---|---|---|
| Hallux valgus angle | 33.2 ± 8.0° | 11.5 ± 7.4° | 21.7° (19.9° to 23.5°) | <0.001 |
| Intermetatarsal angle | 14.4 ± 3.3° | 6.8 ± 3.7° | 7.5° (6.8° to 8.3°) | <0.001 |
| Calcaneal pitch angle | 17.7 ± 6.8° | 21.5 ± 6.8° | -3.8° (-4.9° to -2.6°) | <0.001 |
| Meary's angle | 5.5° ± 4.1° | 5.7° ± 4.4° | -0.2° (-1.3° to 0.9°) | 0.721 |
| Sesamoid position (LaPorta position) | 5.6 ± 1.5 | 2.7 ± 1.3 | 2.9 (2.6 to 3.3) | <0.001 |
Table 2: Effect of operation on radiologic parameters.
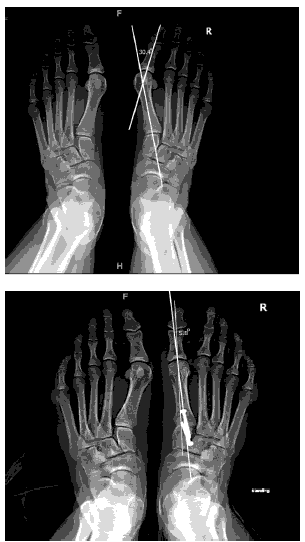
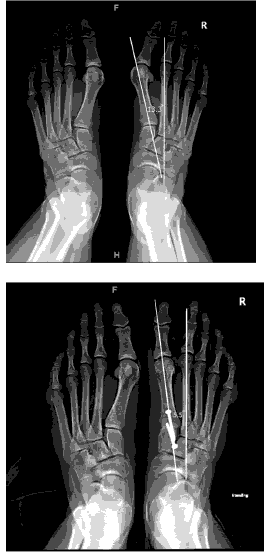
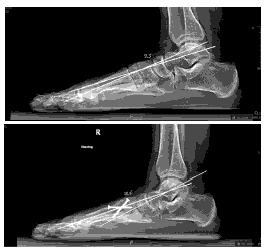
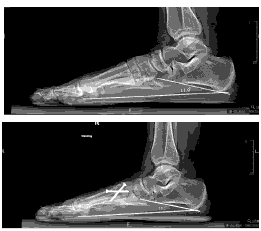
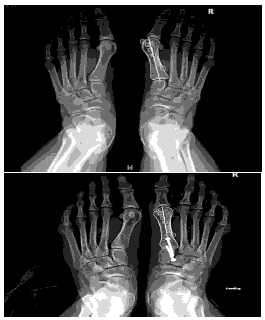
In terms of adjunct procedures, 51 patients (51%) underwent gastrocnemius/Achilles elongation, and one patient underwent Weil osteotomy (1%). There were no reports of infection or nonunion. There was one reoperation (1%) due to broken screws. The mean hallux valgus correction angle between the preoperative and postoperative follow-up radiographs shown in Table 2 was 21.7 (p<0.001). The mean Meary’s angle was 5.5° preoperatively and 5.7° postoperatively, with a mean change of 0.2° (p<0.721; CI, (-1.3–0.9)). The average increase in the calcaneal pitch angle was 3.8° (p<0.001). The average decrease in the intermetatarsal angle was 7.5° (p<.001; CI, (6.8–8.3)) [Figure 1].
The LaPorta classification was used to measure the rotational correction of the 1st metatarsal along its longitudinal axis. The average decrease in the LaPorta classification was 2.9 units (p<0.001; CI, (2.6–3.3)). Postoperatively, no patients were in the LaPorta group 6 or 7. [Figure 2–Figure 5]
Discussion
Several procedures have been described in the literature for symptomatic hallux valgus, such as the Lapidus procedure, modified McBride procedure, distal metatarsal osteotomies, metatarsal shaft osteotomies, Akin osteotomy, proximal metatarsal osteotomies, and hallux joint fusion. [40]
The indications of the Lapidus procedure have been well described in the literature, including the increase in the angulation of the 1st tarsometatarsal joint inclination of >30°. Increased mobility of the 1st ray along with instability is also [46-51] an indication. Hallux valgus with pes planovalgus has been considered as an indication for surgical correction with the Lapidus procedure, particularly for hypermobility of the 1st tarsometatarsal joint associated with pes planovalgus. However, the significance and surgical treatment of medial column hypermobility is an area of debate among surgeons. [52,53]
In this procedure, the windlass mechanism of the 1st metatarsophalangeal joint remains intact. [54] The 1st metatarsal rotational correction mimics the peroneus longus function of the foot. [55] First tarsometatarsal joint arthrodesis has shown an improvement in the efficiency of the peroneus longus in stabilizing the medial column. [16] In the method described, the 1st metatarsal head is restored back onto the sesamoids, and the hallux is derotated and straightened, with attenuation of the medial joint capsule along with modified McBride. [45]
The relationship between both Meary’s angle and calcaneal pitch and hallux valgus has been described in the literature. Coughlin et al. conducted a study on 118 feet (44% had hallux valgus); there was no statistical significance between both groups in terms of the incidence of pes planus or pes cavus. Saragus et al. reviewed 34 male patients (41 feet) and found similar results. [30,56] Although hallux valgus is not generally associated with the cavus foot, [22] our results demonstrated that the majority of our patients had a positive Meary’s angle preoperatively, indicating a more plantar flexion of the 1st tarsometatarsal. According to Klemola et al., eversion of the 1st metatarsal in pes planovalgus will cause lateralization of the sesamoids in a fixed hallux valgus deformity; thus, they only recommend the 1st tarsometatarsal joint derotational arthrodesis for flexible deformities. [54]
In this study, the mean hallux valgus angle correction was 21.7°. Torkki et al. reported a 10° correction of the hallux valgus angle using the chevron osteotomy technique, [57] while Klemola et al. had relatively close numbers with a mean difference of 19.8° in the hallux valgus angle corrections using the Lapidus procedure [54]
In a retrospective study by Rink-Brüne on 106 patients, the Lapidus procedure showed a high success rate and reproducible correction in cases of severe hallux valgus with an intermetatarsal angle greater than 15°. Moreover, the author suggested that in patients with first ray hypermobility, the sesamoid position is a better measurement for under correction than the IM angle, irrespective of the type of surgery performed. In addition, patients had an overall mean postoperative sesamoid position of 2.5, which is similar to that in this study, suggesting that the Lapidus procedure can restore joint alignment irrespective of the severity of metatarsus adducts. [58]
The sesamoid position is classified according to LaPorta into 7 grades in relation to the axis of the 1st metatarsal, where the normal is grade 1, grade 7 is the most subluxated position laterally, and grade 4 is considered to be at the center of the shaft. [44] When there is a lateral displacement of the sesamoid bone, it indicates that there is a displacement of the 1st metatarsal to the medial side. Surgical reduction of the sesamoid bone into a more medial position can reduce the whole deformity of the metatarsophalangeal joint, which helps decrease the chance of recurrence. [59] In a study that followed up 88 feet with hallux valgus that underwent first tarsometatarsal joint derotational arthrodesis with a total follow-up of 3–8 years, the Lapidus procedure had a great impact on correcting the tibia-sesamoid bone by decreasing the LaPorta degree by 1.1 units (95% CI: 0.9–1.4; p<.001) compared to 2.9 units correction in this study. [60]
In another study with a sample size of 29 patients undergoing the Lapidus procedure, the overall satisfaction rate was 90% (26/29 patients), and 86% (25/29 patients) had satisfaction regarding the cosmetic outcome. [61]
The most common complication in the Lapidus procedure was a recurrence of hallux valgus deformity, [62] along with the shortening of the 1st metatarsal and failure of fixation. [63-65] Lapidus has acknowledged the shortening of the 1st metatarsal and, to avoid this issue, has advised the minimization of cutting in the lateral articular surface of the cuneiform and the 1st metatarsal along with a smaller wedge osteotomy. [13,66] The recurrence rate was low after the Lapidus procedure, in a study by Bennet et al. on 107 feet, of which 13% had a failure of fusion related to implant failure, but only 2% required operative treatment for recurrence. [67] Moreover, in another multicenter study that included 342 patients who underwent the modified Lapidus procedure, the rate of recurrence was found to be 2.92% (10 patients). [68]
There was no nonunion of the first tarsometatarsal joint fusion site reported in our study, even though nonunion usually carries a concern among surgeons. In a multicenter study by Prissel et al., which focused on nonunion following the Lapidus procedure, nonunion was not a common complication. Only 6.5% of the sample size of 367 patients developed a nonunion. In addition, they challenged whether the timing of the weightbearing had any effect on the union, describing that early weight-bearing within 21 days after surgery does not affect the union. [69] Another study showed the incidence of nonunion after Lapidus arthrodesis (8.3%) with a sample size of 35 patients. [70] However, Coetze et al. argued that wound complications and smoking are major risk factors for nonunion in the Lapidus procedure. [71]
Although the Lapidus procedure is an effective hallux valgus treatment method that corrects the intermetatarsal angle and the Laporta classification, it does not suit those with degenerative changes or fixed deformities due to the chance of causing lateralization of the sesamoids. [54]
The limitations of the present study were its retrospective nature and the short-term follow-up. In addition, pre- and postoperative evaluation of patient satisfaction was not measured, and there was a lack of a control group to compare other surgical techniques that could have added more value to our study.
Conclusion
The purpose of our study was to report the efficacy of the Lapidus procedure in the correction of the deformity radiologically. The 1st tarsometatarsal joint derotational arthrodesis produced good radiologic results on flexible hallux valgus. In addition, the LaPorta classification showed a significant decrease and proper positioning of the sesamoids postoperatively. We recommend additional studies with a longer follow-up period be conducted to determine the effect of this procedure and the recurrence of Hallux Valgus.
Competing Interests
The authors report no competing (commercial/academic) interests.
Acknowledgements
We are grateful to the College of Medicine Research Center (CMRC), Deanship for Scientific Research, King Saud University
REFERENCES
- Suzuki J, Tanaka Y, Takaoka T, Kadono K, Takakura Y. Axial radiographic evaluation in hallux valgus: evaluation of the transverse arch in the forefoot. J Orthop Sci. 2004;9:446-451.
- Geng X, Zhang C, Ma X, Wang X, Huang J, Xu J, et al. Lateral sesamoid position relative to the second metatarsal in feet with and without hallux valgus: a prospective study. J Foot Ankle Surg. 2016;55:136-139.
- Nix SE, Vicenzino BT, Collins NJ, Smith MD. Gait parameters associated with hallux valgus: a systematic review. J Foot Ankle Res. 2013;6:1-2.
- Li X, Guo M, Zhu Y, one XXP. The excessive length of first ray as a risk factor for hallux valgus recurrence. PloS one. 2018;13:e0205560.
- Hueter C. Klinik der Gelenkkrankheiten mit Einschluß der Orthopädie. 1877.
- Durlacher L. A treatise on corns, bunions, and diseases of the nails. Med Chir Rev. 1845;2:239-243.
- Sim-Fook L, Hodgson AR. A comparison of foot forms among the non-shoe and shoe-wearing Chinese population. JBJS. 1958;40-A:1058-1062.
- Hurn SE, Vicenzino BT, Smith MD. Correlates of foot pain severity in adults with hallux valgus: a cross-sectional study. J Foot Ankle Res. 2014;7:1-10.
- Wen J, Ding Q, Yu Z, Sun W, Wang Q, Wei K. Adaptive changes of foot pressure in hallux valgus patients. Gait Posture. 2012;36:344-349.
- Koller U, Willegger M, Windhager R, Wanivenhaus A, Trnka HJ, Schuh R. Plantar pressure characteristics in hallux valgus feet. J Orthop Res. 2014;32:1688-1693.
- Glasoe WM. Treatment of progressive first metatarsophalangeal hallux valgus deformity: a biomechanically based muscle-strengthening approach. J Orthop Sports Phys Ther. 2016;46:596-605.
- Mann RA, Coughlin MJ. Hallux valgus--etiology, anatomy, treatment and surgical considerations. Clin Orthop Relat Res. 1981;31-41.
- Dietze A, Bahlke U, Martin H, Mittlmeier T. First ray instability in hallux valgus deformity: a radiokinematic and pedobarographic analysis. Foot Ankle Int. 2013;34:124-130.
- Alkhaibary. Hallux valgus in Riyadh, Saudi Arabia: Prevalence, characteristics, and its associations. J Musculoskelet Surg. Medknow Publications; 2019;3:292.
- Al-Abdulwahab SS, Al-Dosry RD. Hallux valgus and preferred shoe types among young healthy Saudi Arabian females. Ann Saudi Med. 2000;20:319-321.
- Hurn SE, Vicenzino B, Smith MD. Functional impairments characterizing mild, moderate, and severe hallux valgus. Arthritis Care Res (Hoboken). 2015;67:80-88.
- Galica AM, Hagedorn TJ, Dufour AB, Riskowski JL, Hillstrom HJ, Casey VA, et al. Hallux valgus and plantar pressure loading: the Framingham foot study. J Foot Ankle Res. 2013;6:1-8.
- Hutton WC, related MDCOA, 1981. The mechanics of normal and hallux valgus feet--a quantitative study. Clin Orthop Relat Res. 1981;157:7-13.
- Menz HB. Biomechanics of the ageing foot and ankle: a mini-review. GER. Karger Publishers; 2015;61:381-388.
- Hendry GJ, Fenocchi L, Woodburn J, Steultjens M. Foot pain and foot health in an educated population of adults: results from the Glasgow Caledonian University Alumni Foot Health Survey. J Foot Ankle Res. 2018;11:48.
- Menz HB. Chronic foot pain in older people. Maturitas. 2016;91:110-114.
- Inman VT. Hallux valgus: a review of etiologic factors. Orthop Clin North Am. 1974;5:59-66.
- Greenberg GS. Relationship of hallux abductus angle and first metatarsal angle to severity of pronation. J Am Podiatry Assoc. 1979;69:29-34.
- Phillips RD, Phillips RL. Quantitative analysis of the locking position of the midtarsal joint. J Am Podiatry Assoc. 1983;73:518-522.
- Shine LB. Incidence of hallux valgus in a partially shoe-wearing community. Br Med J. 1965;1:1648-1650.
- Speksnijder CM, vander Munckhof RJH, Moonen SAFCM, Walenkamp GHIM. The higher the heel the higher the forefoot-pressure in ten healthy women. The Foot. 2005;15:17-21.
- Nguyen U-SDT, Hillstrom HJ, Li W, Dufour AB, Kiel DP, Procter-Gray E, et al. Factors associated with hallux valgus in a population-based study of older women and men: the MOBILIZE Boston Study. Osteoarthr Cartil. 2010;18:41-46.
- Corrigan JP, Moore DP, Stephens MM. Effect of heel height on forefoot loading. Foot & Ankle. 2016;14:148-152.
- Snijders CJ, Snijder JGN, Philippens MMGM. Biomechanics of hallux valgus and spread foot. Foot & Ankle. 2016;7:26-39.
- Coughlin MJ, Thompson FM. The high price of high-fashion footwear. Instr Course Lect. 1995;44:371-377.
- Scott G, Menz HB, Newcombe L. Age-related differences in foot structure and function. Gait & Posture. 2007;26:68-75.
- Hagedorn TJ, Dufour AB, Riskowski JL, Hillstrom HJ, Menz HB, Casey VA, et al. Foot disorders, foot posture, and foot function: the Framingham foot study. PLoS One. 2013;8:e74364.
- Hardy RH, Clapham JCR. Observations on hallux valgus; based on a controlled series. J Bone Jt Surg. 1951;33:376-391.
- Johnston O. Further studies of the inheritance of hand and foot anomalies. Clin Orthop. 1956;8:146-60.
- Piqué-Vidal C, Solé MT, Antich J. Hallux valgus inheritance: pedigree research in 350 patients with bunion deformity. J Foot Ankle Surg. 2007;46:149-154.
- Cho NH, Kim S, Kwon D-J, Kim HA. The prevalence of hallux valgus and its association with foot pain and function in a rural Korean community. J Bone Jt Surg. 2009;91:494-498.
- Lee KM, Ahn S, Chung CY, Sung KH, Park MS. Reliability and relationship of radiographic measurements in hallux valgus. Clin Orthop Relat Res. 2012;470:2613-2621.
- Coughlin MJ, Jones CP. Hallux valgus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007;28:759-777.
- DiDomenico LA, Fahim R, Rollandini J, Thomas ZM. Correction of frontal plane rotation of sesamoid apparatus during the Lapidus procedure: a novel approach. J Foot Ankle Surg. 2014;53:248-251.
- Fraissler L, Konrads C, Hoberg M, Rudert M, Walcher M. Treatment of hallux valgus deformity. EFORT Open Rev. 2016;1:295-302.
- Coughlin MJ, Saltzman CL, Nunley JA. Angular measurements in the evaluation of hallux valgus deformities: a report of the ad hoc committee of the American Orthopaedic Foot & Ankle Society on angular measurements. Foot Ankle Int. 2002;23:68-74.
- Romash MM, Fugate D, Yanklowit B. Passive motion of the first metatarsal cuneiform joint: preoperative assessment. Foot & Ankle. 1990;10:293-298.
- Coughlin MJ. Hallux valgus in men: effect of the distal metatarsal articular angle on hallux valgus correction. Foot Ankle Int. 1997;18:463-470.
- Laporta G, Melillo T, Olinsky D. X-ray evaluation of hallux abducto valgus deformity. J Am Podiatr Med Assoc. 2014;64:544-566.
- Mcbride ED. The mcbride bunion hallux valgus operation: refinements in the successive surgical steps of the operation. JBJS. 1967;49:1675.
- Sangeorzan BJ, Hansen ST. Modified Lapidus procedure for hallux valgus. Foot & Ankle. 1989;9:262-266.
- Saffo G, Wooster MF, Stevens M, Desnoyers R, Catanzariti AR. First metatarsocuneiform joint arthrodesis: a five-year retrospective analysis. J Foot Surg. 1989;28:459-465.
- Chang TJ, Ruch JA. Lapidus arthrodesis: a different perspective. J Am Podiatr Med Assoc. 1994;84:281-288.
- Bacardi BE, Boysen TJ. Considerations for the Lapidus operation. J Foot Surg. 1986;25:133-138.
- Klaue K, Hansen ST, Masquelet AC. Clinical, quantitative assessment of first tarsometatarsal mobility in the sagittal plane and its relation to hallux valgus deformity. Foot Ankle Int. 1994;15:9-13.
- Goldner JL, Gaines RW. Adult and juvenile hallux valgus: analysis and treatment. Orthop Clin North Am. 1976;7:863-887.
- Myerson M. Metatarsocuneiform arthrodesis for treatment of hallux valgus and metatarsus primus varus. Orthopedics. 1990;13:1025-1031.
- Hansen ST. Hallux valgus surgery. Morton and Lapidus were right! Clin Podiatr Med Surg. 1996;13:347-354.
- Klemola T, Leppilahti J, Kalinainen S, Ohtonen P, Ojala R, Savola O. First tarsometatarsal joint derotational arthrodesis—a new operative technique for flexible hallux valgus without touching the first metatarsophalangeal joint. J Foot Ankle Surg. 2014;53:22-28.
- Johnson CH, Christensen JC. Biomechanics of the first ray part I. The effects of peroneus longus function: A three-dimensional kinematic study on a cadaver model. J Foot Ankle Surg. 1999;38:313-321.
- Saragas NP, Becker PJ. Comparative radiographic analysis of parameters in feet with and without hallux valgus. Foot Ankle Int. 1995;16:139-143.
- Torkki M, Malmivaara A, Seitsalo S, Hoikka V, Laippala P, Paavolainen P. Surgery vs orthosis vs watchful waiting for hallux valgus: a randomized controlled trial. JAMA. 2001;285:2474-2480.
- Rink-Brüne O. Lapidus arthrodesis for management of hallux valgus—a retrospective review of 106 cases. J Foot Ankle Surg. 2004;43:290-295.
- Smith RW, Reynolds JC, Stewart MJ. Hallux valgus assessment: report of research committee of American Orthopaedic Foot and Ankle Society. Foot & Ankle. 1984;5:92-103.
- Klemola T, Savola O, Ohtonen P, Ojala R, Leppilahti J. First tarsometatarsal joint derotational arthrodesis for flexible hallux valgus: results from follow-up of 3–8?years. Scand. J. Surg. 2017;106:325-331.
- Kopp FJ, Patel MM, Levine DS, Deland JT. The modified lapidus procedure for hallux valgus: a clinical and radiographic analysis. Foot Ankle Int. 2016;26:913-917.
- Kilmartin TE, O'Kane C. Combined rotation scarf and Akin osteotomies for hallux valgus: a patient focussed 9 year follow up of 50 patients. J Foot Ankle Res. 2010;3:2-12.
- Myerson M, Allon S, McGarvey W. Metatarsocuneiform arthrodesis for management of hallux valgus and metatarsus primus varus. Foot & Ankle. 1992;13:107-115.
- Sangeorzan BJ, Sigvard T Hansen J. Modified lapidus procedure for hallux valgus. Foot & Ankle. 2017;9:262-266.
- Catanzariti AR, Mendicino RW, Lee MS, Gallina MR. The modified Lapidus arthrodesis: a retrospective analysis. J Foot Ankle Surg. 1999;38:322-332.
- Kleinberg S. The operative cure of hallux valgus and bunions. Am J Surg. 1932;15:75-81.
- Bennett GL, Kay DB, Sabatta J. First metatarsophalangeal joint arthrodesis: an evaluation of hardware failure. Foot Ankle Int. 2016;26:593-596.
- Lagaay PM, Hamilton GA, Ford LA, Williams ME, Rush SM, Schuberth JM. Rates of revision surgery using chevron-austin osteotomy, lapidus arthrodesis, and closing base wedge osteotomy for correction of hallux valgus deformity. J Foot Ankle Surg. 2008;47:267-272.
- Prissel MA, Hyer CF, Grambart ST, Bussewitz BW, Brigido SA, DiDomenico LA, et al. A multicenter, retrospective study of early weightbearing for modified lapidus arthrodesis. J Foot Ankle Surg. 2016;55:226-229.
- Mallette JP, Glenn CL, Glod DJ. The incidence of nonunion after lapidus arthrodesis using staple fixation. J Foot Ankle Surg. 2014;53:303-306.
- Coetzee JC, Resig SG, Kuskowski M, Saleh KJ. The lapidus procedure as salvage after failed surgical treatment of hallux valgus: a prospective cohort study. J Bone Jt Surg. 2003;85:60.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.