Renal Tuberculosis Mimicking a Systemic Lupus Erythematosus Renal Flare
Received: 14-Feb-2024, Manuscript No. amhsr-24-131898; Editor assigned: 16-Feb-2024, Pre QC No. amhsr-24-131898 (PQ); Reviewed: 01-Mar-2024 QC No. amhsr-24-131898 ; Revised: 08-Mar-2024, Manuscript No. amhsr-24-131898 (R); Published: 18-Mar-2024
Citation: Sayhi S, et al. Renal Tuberculosis Mimicking a Systemic Lupus Erythematosus Renal Flare. Ann Med Health Sci Res. 2024;14:943-944.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Infections are frequent and grave problems in patients with systemic lupus erythematosus. Infections have been incriminated in initiating the disease and are usually responsible for relapses. However, infections such as tuberculosis can also mimic systemic lupus erythematosus flares resulting in challenging differential diagnosis and often delayed therapy. In this regard, we report the case of a twenty-six year-old male in whom diagnosis of systemic lupus erythematosus with joint, pleural and hematological involvement was retained. The patient presented three months after initial diagnosis fever, dry cough and mild proteinuria with laboratory evidence of inflammation. Renal flare related to systemic lupus or Sjögren’s syndrome was suspected and thus renal biopsy was performed. Histological examination revealed granuloma with caseating necrosis associated with sings of tubulointersitial nephropathy. Chest and abdominal computed tomography revealed the presence of an excavated nodule of the right lung but also three nodular lesions of the right kidney ranging from 4 to 11 mm. Diagnosis of pulmonary and renal tuberculosis was retained. Treatment with oral anti-tuberculosis drugs was initiated with favorable outcome.
Keywords
Systemic Lupus Erythematosus; Tuberculosis; Nephropathy; Granuloma
Introduction
Patients with Systemic Lupus Erythematosus (SLE) present a higher risk for infections. This can either be related to intrinsic immunological deficits or frequent usage of corticosteroids and immunosuppressive therapy [1]. Infection is the first cause of mortality for patient with SLE during the first year of disease evolution [2]. Higher rate of tuberculosis is observed in patients with SLE compared with general population especially in endemic countries [3]. Genitourinary system tuberculosis is the third most frequent extra-pulmonary location, in which case kidneys are usually affected. We report a case of patient with SLE who presented renal tuberculosis three months after SLE diagnosis mimicking a SLE renal flare.
Case Presentation
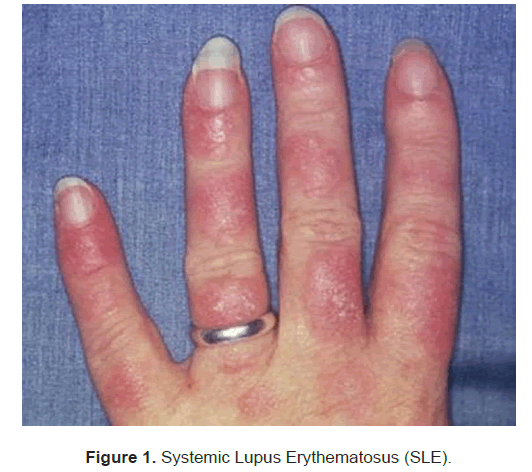
Twenty-six year-old man with a medical history of agenesis of the left forearm was referred to our internal medicine department for inflammatory joint pain associated with fever and involuntarily weight loss. Patient denied intake of any medication or illicit drugs. On clinical examination, patient was febrile. He presented painful swelling regarding the knees and the rightwrist. There were no palpable lymphadenopathy and the rest of examination was without abnormalities. Routine laboratory tests revealed signs of inflammation with elevated C-reactive protein: 42 mg/l and erythrocyte sedimentation rate: 84 mmH 1. Full blood count showed lymphopeania at 900/mm3 while hemoglobin and platelet count were normal. Kidney and liver function tests were within normal range. Polyclonal hypergammapolyglobulinemia: 16 g/l was also noted. Urinalysis was without abnormalities. Chest X-ray noted the presence of pleural effusion. Infectious investigation did not yield positive results. Echocardiography did not show signs of pericardial effusion nor of infectious endocarditis. Tuberculin skin test was negative. Immunologic work-up concluded to positive antinuclear antibodies at 1/1280 with positive SSA, SSB and Sm antibodies. Rheumatoid factor and cyclic citrullinated antibodies were absent. Diagnosis of systemic lupus erythematosus with joint, pleural and hematological involvement was retained and patient was put on Hydroxychloriquine 400 mg/day with favorable clinical course (Figure 1).
Three months later, patient was readmitted for reoccurrence of fever, dry cough and positive proteinuria. Other than fever, clinical examination was without remarkable finding especially auscultation of the respiratory system. Laboratory signs of inflammations were present with elevated C-reactive protein: 66 mg/l and erythrocyte sedimentation rate: 102 mmH 1. A slight renal impairment was noted with creatinine serum level at 140 μmol/l with an estimated glomerular filtration rate at 56 ml/min Modification of Diet in Renal Disease (MDRD). Urinalysis revealed the presence of high urinary leucocyte count (leucocyturie: 30 elements/mm3) and proteinuria at 0.6 g/24 h. Urine bacteriologic and mycological investigations were negative. Chest X-ray was normal. Systemic lupus erythematosus renal flare or renal involvement related to Sjögren syndrome was suspected given the eye and mouth dryness reported by the patient. Renal ultrasound did not reveal abnormalities. Thus, renal biopsy was performed. Histological examination noted the presence of granuloma with caseating necrosis associated with signs of tubulointersitial nephropathy. Diagnosis of tuberculosis was highly suspected. Sputum and urine culture did not objectify Koch bacillus. Chest and abdominal computed tomography revealed the presence of an excavated nodule of the right lung but also three nodular lesions of the right kidney ranging from 4 mm to 11 mm. Given the finding of renal biopsy, chest and abdominal computed tomography, diagnosis of renal tuberculosis with likely associated pulmonary tuberculosis was retained. Patient was put on oral anti-tuberculosis treatment. Clinical course was marked by complete regression of fever and disappearance of the cough; renal laboratory tests and proteinuria were within normal range after two months of treatment.
Discussion
Tuberculosis is one of the most frequently encountered infections in patient with SLE, especially in endemic regions [3]. High mean dose of corticosteroids, renal and neurological involvement are important risk factors for development of tuberculosis in such patients [4]. SLE presents a favorable condition for tuberculosis as the risk is reported to be 5 to 60 folds compared to general population [5]. Interaction between tuberculosis and SLE are quite complicated as symptoms such as fever, sweating and lymphadenopathy may be observed in both diseases. Meanwhile, multiples studies also proved that tuberculosis can be responsible for SLE flare [6]. Renal tuberculosis may mimic a conventional urinary tract bacterial infection. Resistance to antibiotics may triggers suspicion. It can also mimic SLE renal flair. In our case, diagnosis of SLE flair with renal involvement was initially suspected considering the medical history of our patient and the negativity of conventional infectious investigations. Also, our patient presented renal function deterioration which is uncommon in tuberculosis. It was histological examination of renal tissue that allowed differential diagnosis.
A sensitivity of 42.7% was demonstrated in the detection of acid- fast bacilli in urine. Computed tomography hold an important place in renal tuberculosis exploration as it allows to search for parenchymal cavities, mass and scarring [5]. Our patient did not present abnormalities at renal ultrasound imaging; however, abdominal computed tomography highlighted the presence of nodules at the kidneys confirming the importance of this imaging technique. Koch bacilli search in urine was negative. Tuberculin skin test can behelpful in case of clinical suspicion; however in immunocompromised patients such as those with SLE, it has a low sensitivity and specificity. Thus, using interferon-gamma release assay is usually recommended in those conditions [4]. Screening for latent tuberculosis is highly important in patients presenting chronic auto-immune or inflammatory diseases. If patient condition requires corticosteroid or immunosuppressive therapy, prophylactic anti-tuberculosis treatment may be initiated in case of latent tuberculosis suspicion.
Our patient also presented an excavated nodule of the lung on chest computed tomography which is probably related to tuberculosis infection. Pulmonary tuberculosis in patients with SLE tends to have higher incidence of miliary disease due to delay in diagnosis and non-specific clinical symptoms that mimic lupus [5].
Treatment is a delicate issue in patient presenting tuberculosis associated with SLE. Clearly anti-tuberculosis therapy is a must. However some authors recommend association with corticosteroid as to avoid SLE flare which can be as life- threatening as tuberculosis [4]. Our patient did not receive corticosteroid therapy as he did not exhibit signs of SLE flare and clinical course was favorable on tuberculosis treatment.
Conclusion
Tuberculosis and systemic lupus erythematosus clinical manifestations usually overlap making the diagnosis difficult. Such was the case in our patient as SLE renal flair was initially suspected. Extra pulmonary tuberculosis is becoming more frequent in immunocompromised patients. As patients present signs of systemic lupus flare, searching for a concomitant infection is mandatory especially tuberculosis as SLE treatment may lead to serious complications in such patients.
References
- Gonzalez LA, Munoz C, Restrepo M, Vanegas AL, Vasquez G. Tuberculosis infection causing intestinal perforations in 2 patients with systemic lupus Erythematosus. J Clin Rheumatol. 2014;20:287–290.
[Crossref] [Google Scholar] [PubMed]
- Sciascia S, Cuadrado MJ, Karim MY. Management of infection in systemic lupus Erythematosus. Best PractRes Clin Rheumatol. 2013;27:377-89.
- Ruangnapa K, Dissaneewate P, Vachvanichsanong P. Tuberculosis in SLE patients: Rare diagnosis, riskytreatment. Clin Exp Med. 2014.
- Prabu V, Agrawal S. Systemic lupus erythematosus and tuberculosis: A review of complex interactions of complicateddiseases. J Postgrad Med. 2010;56:244-250.
- Hou CL, Tsai YC, Chen LC. Tuberculosis infection in patients with systemic lupus erythematosus: Pulmonary and extra-pulmonary infection compared. Clin Rheumatol 2008;27:557–63. [Crossref]
[Google Scholar] [PubMed]
- Lin YC, Liang SJ, Liu YH. Tuberculosis as a risk factor for systemic lupus erythematosus: Results of a nationwide study in Taiwan. Rheumatol Int 2012; 32: 1669-73.
[Crossref] [Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.