Report of a Rare Case of an Odontogenic Myxoma of the Maxilla and Review of Literature
- *Corresponding Author:
- Dr. SM Manjunath
Department of Oral Pathology and Microbiology, MM College of Dental Sciences, MM University, Mullana, Ambala, Haryana, India.
E-mail: smmanjunath29@rediffmail.com
Citation: Manjunath SM, Gupta AA, Swetha P, Moon NJ, Singh S, Singh A. Report of a rare case of an odontogenic myxoma of the maxilla and review of literature. Ann Med Health Sci Res 2014;4:45-8.
Abstract
Odontogenic myxoma (OM) is a mesenchymal tissue benign neoplasia, being relatively rare which is almost exclusively seen in tooth‑bearing areas. OM commonly occurs in the 2nd and 3rd decade and the mandible is involved more commonly than the maxilla. The lesion often grows without symptoms and presents as a painless swelling. Radiographically, the myxoma appears as a unilocular or multilocular radiolucency. This article presents a rare case of OM occurring in the maxilla of a 28‑year‑old female patient with a brief review of the literature.
Keywords
Fibromyxoma, Odontogenic myxomas, Odontogenic tumors
Introduction
Odontogenic myxoma (OM) of the jaws, first described by Thoma and Goldman in 1947, is believed to arise from odontogenic ectomesenchyme.[1,2] It is a rare benign tumor characterized grossly by mucoid or gelatinous grayish‑white tissue that replaces the cancellous bone and expands the cortex. OMs are locally invasive, non‑metastasizing neoplasms of the jaws, almost exclusively seen in tooth‑bearing areas. It accounts for 0.2‑17.7% of odontogenic tumors. It predominantly involves the mandible and maxillary tumors are known to be more aggressive than tumors involving the mandible.[3] Most frequently, OMs occur in the 2nd and 3rd decades of life. Cortical expansion and perforation are common findings; however, maxillary myxomas often extend into the sinus.[4]
Materials and Methods
Radiographically, the tumor presents as a unilocular or multilocular radiolucent lesion with fine, bony trabeculae within its interior structure expressing a honeycombed, soap bubble, or tennis racket appearance.[5] A histologic characteristic of this tumor resembles the mesenchymal portion of a tooth in development. The lesion is not encapsulated being characterized by the proliferation of a few rounded cells, fusiforms and star cells, being included in abundant myxomatous stroma with a few collagen fibers.[6] In this article, we present a case of OM occurring in the maxilla of a 28‑year‑old female patient followed by a review of the literature.
Case Report
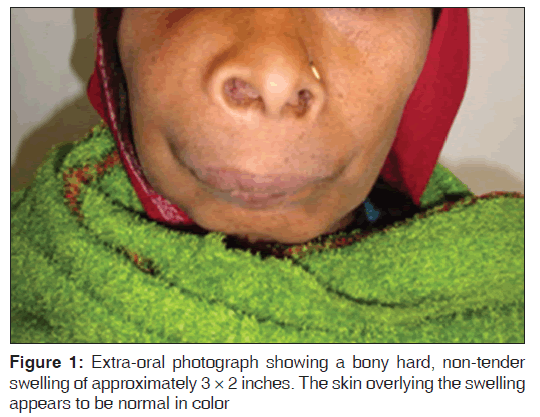
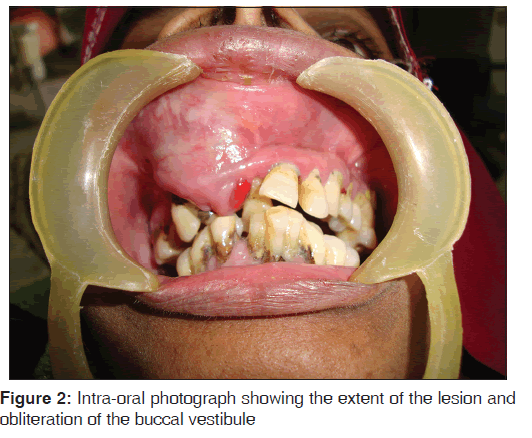
The present case report is about a 28‑year‑old female patient who presented for the evaluation of a swelling on the front region of her face. Clinically, the swelling was painless with associated nasal discharge and deviation of the nasal septum. She had a bony hard, non‑tender swelling of approximately 3 × 2 inches, extending superoinferiorly from the infra‑orbital ridge of the right side to the level of the right corner of the mouth and anteroposteriorly from the right corner of the mouth to the anterior border of the ramus [Figure 1]. The borders of the swelling were diffuse and the skin overlying the swelling was normal in color. Intra‑oral examination revealed a non‑tender, bony hard swelling extending from the maxillary right central incisor to the right second premolar, thereby obliterating the buccal vestibule [Figure 2]. The associated teeth were displaced and showed Grade‑I mobility.
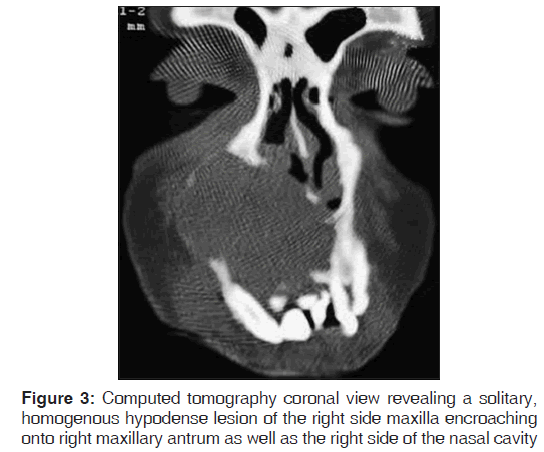
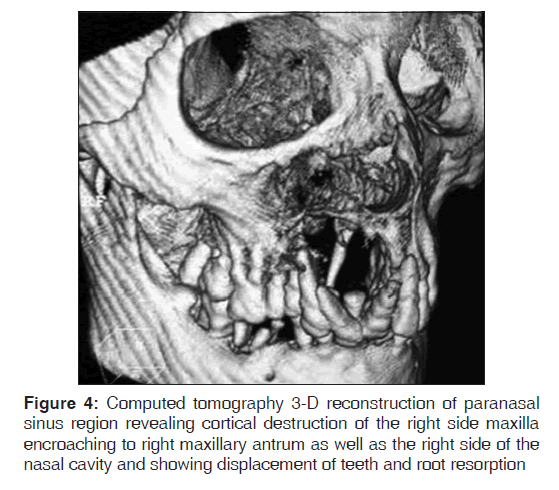
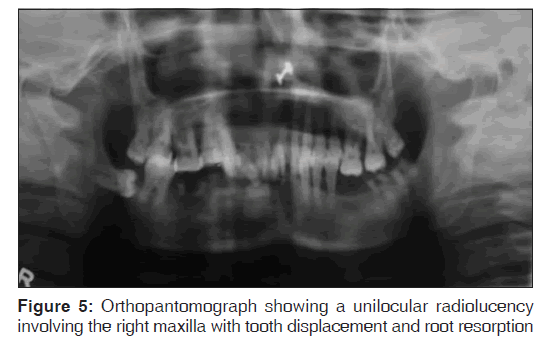
The computed tomography (CT) scan revealed a solitary, homogenous hypodense lesion of the right side maxilla encroaching onto right maxillary antrum as well as the right side of the nasal cavity. The lesion crossed the midline medially, extended superiorly to right infra‑orbital margin and inferiorly to the right side palate [Figure 3]. CT 3‑D reconstruction of paranasal sinus region revealed cortical destruction of the right side maxilla encroaching onto right maxillary antrum as well as the right side of the nasal cavity and also showed displacement of teeth and root resorption [Figure 4]. Orthopantomograph revealed a unilocular radiolucency involving the right maxilla with tooth displacement and root resorption [Figure 5].
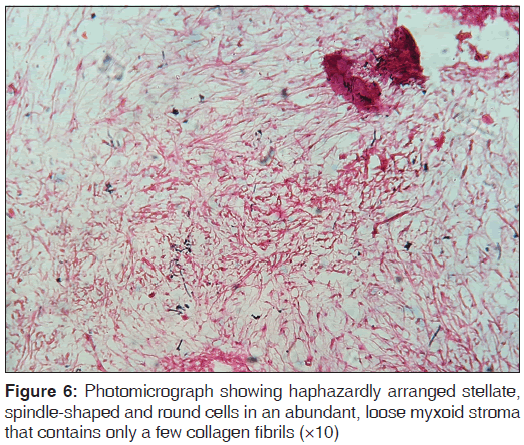
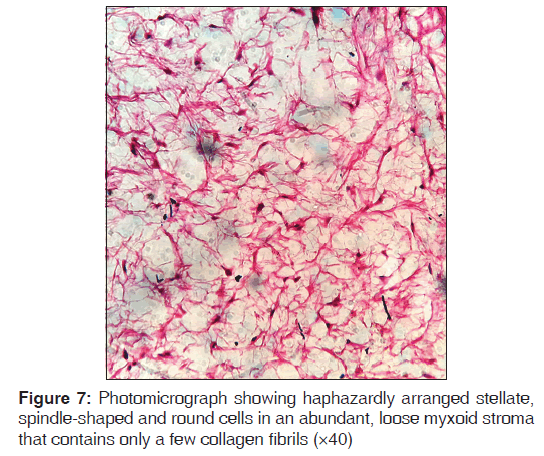
The lesion was surgically removed. On gross examination, the specimen was a white gelatinous mass. Histopathological examination of the biopsy specimen revealed haphazardly arranged stellate, spindle shaped and round cells in an abundant, loose myxoid stroma that contained only a few collagen fibrils [Figures 6 and 7]. The loose, myxomatous tissue was seen filling the marrow spaces between the bony trabeculae [Figure 8].
Discussion
Myxomas of the head and neck are rare tumors. Two forms can be identified: (1) Facial bone derived, which had been subdivided in the past into true osteogenic myxoma and OM; and (2) “soft‑tissue”‑derived myxoma, derived from the perioral soft‑tissue, parotid gland, ear and larynx.[7] Virchow, in 1863, coined the term myxoma for a group of tumors that had histologic resemblance to the mucinous substance of the umbilical cord.[8] In the year 1948, Stout redefined the histologic criteria for myxomas as true neoplasms that do not metastasize and exclude the presence of recognizable cellular components of other mesenchymal tissues, especially chondroblasts, lipoblasts and rhabdomyoblasts.[4]
Traditionally, the myxoma of the maxilla and mandible has been considered to be a neoplasm of odontogenic origin. Although the evidence is mainly circumstantial, support of an odontogenic origin has been perpetuated by its almost exclusive occurrence in the tooth‑bearing areas of the jaws, its common association with an unerupted tooth or a developmentally absent tooth, its frequent occurrence in young individuals, its histologic resemblance to dental mesenchyme, especially the dental papilla and the occasional presence of sparse amounts of odontogenic epithelium.[4,9]
OM is a rare aggressive intra‑osseous lesion derived from embryonic mesenchymal tissue associated with odontogenesis and primarily consisting of a myxomatous ground substance with widely scattered undifferentiated spindled mesenchymal cells.[10] Odontogenic maxillary myxomas were first mentioned in the literature by Thoma and Goldman in 1947.[2] The OM is a benign, slow growing locally aggressive neoplasm of ectomesenchymal origin. This neoplasm occurs almost exclusively in the jaw bones and comprises 0.2‑17.7% of odontogenic tumors.[3,11] It may present at any age but is most frequently discovered in the 2nd‑3rd decades as in the present case.[4] It occurs more frequently in the mandible than in the maxilla with the ratio of 3:1. The male to female ratio is 1:1.5. Maxillary OM, as in the present case is less frequent but behaves more aggressively than in the mandible as it spreads through the maxillary sinus. Displacement of teeth by the tumor is a relatively common finding, but root resorption is rare and the tumor is often scalloped in between the roots.[3,11,12]
Radiographically, the myxoma appears as a unilocular or multilocular radiolucency with irregular or scalloped margins. The radiolucent defect may contain thin, wispy trabeculae of residual bone, which are often arranged at right angles to one another. Large myxomas may show a “soap bubble” radiolucent pattern, which is indistinguishable from that seen in ameloblastomas.[1] In a retrospective radiographic analysis of 21 cases, the mandible was more involved than the maxilla. Furthermore, it was observed that unilocular forms were usually located in the anterior maxilla while the multilocular forms involved the posterior region.[13] Clinical and radiographic differential diagnosis of OMs may include: Intra‑osseous hemangioma, cherubism, aneurysmatic bony cyst, fibrous dysplasia, ameloblastoma, gigantic cells central lesion, traumatic bony cyst and odontogenic cysts (radicular, lateral periodontal, dentigerous and keratocyst).[1,13] CT images of OM may show any of the following features: (1) Osteolytic expansile lesions with mild enhancement of the solid portion of the mass in the myxoma of the mandible; (2) bony expansion and thinning of cortical plates with strong enhancement of the mass lesion in the anterior maxilla; (3) a soft‑tissue mass with bone destruction and thinning and strands of fine lace‑like density representing ossifications in the maxillary sinus.[14]
On histological examination, the OM has abundant mucosal intercellular substance, made up of eosinophilic lax connective tissue. Immersed in this stroma are spindle‑like, star‑shaped cells with elongated cytoplasm, with or without small masses of inactive odontogenic epithelium. These epithelial rests are not required for the diagnosis and are not obvious in most cases. The differential diagnosis must be made with rabdomyosarcoma, myxoid liposarcoma, neurogenic sarcoma, neurofibroma, lipoma, fibroma and chondromyxoid fibroma.[1,15]
Farman et al. reviewed the histochemical findings in OM. The ground substance of OM has been shown to consist of about 80% hyaluronic acid and 20% chondroitin sulfate. Tumor cells appear to be relatively inactive, with low levels of oxidative enzymes. Tumor cells also show slight alkaline phosphatase activity. The myxoid intercellular matrix stains positively with alcian blue, but periodic acid‑Schiff staining may be negative.[16]
The tumor is not radiosensitive and surgery is the treatment of choice. Treatment of OM varies from local excision, curettage, or enucleation to radical resection. OM may be infiltrative and aggressive, with high recurrence rates.[12,16,17] OMs bear a high risk of recurrence, mainly due to its gelatinous aspect and the fact that it does not have a capsule, thus it is necessary that the initial treatment be very efficient. Due to poor follow‑up and lack of reports, a precise analysis of recurrence rates is still missing. Recurrence is considered to be directly related to the type of therapy, with conservative surgery resulting in a higher number of recurrences.[18]
Conclusion
A rare case of OM of the maxilla in a 28‑year‑old female patient has been presented. Clinical and radiological aspects of maxillary OMs are not conclusive, thus it is necessary to have a histopathological examination for the final diagnosis. Due to its high rate of recurrence, especially due to its gelatinous and mucous aspect, surgical treatment through bone resection is the most indicated treatment modality and the patient must be followed‑up closely for years.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Neville BW, Damm DD, Allen CM, Bouquot JE, editors.Odontogenic cysts and tumors. In: Oral and Maxillofacial Pathology. 3rd ed. Philadelphia: WB Saunders; 2010. p. 678-740.
- Noffke CE, Raubenheimer EJ, Chabikuli NJ, Bouckaert MM. Odontogenic myxoma: Review of the literature and report of 30 cases from South Africa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:101-9.
- Jaswal A, Jana AK, Biswas M, Sikder B, Nandi TK. Recurrent odontogenic myxoma of maxilla: A diagnostic and operative dilemma. Indian J Otolaryngol Head Neck Surg 2008;60:41-4.
- Singaraju S, Wanjari SP, Parwani RN. Odontogenic myxoma of the maxilla: A report of a rare case and review of the literature. J Oral Maxillofac Pathol 2010;14:19-23.
- Sivakumar G, Kavitha B, Saraswathi TR, Sivapathasundharam B. Odontogenic myxoma of maxilla. Indian J Dent Res 2008;19:62-5.
- Aquilino RA, Tuji FM, Eid NL, Molina OF, Joo HY, Neto FH. Odontogenic myxoma in the maxilla: A case report and characteristics on CT and MR. Oral Oncol Extra 2006;42:133-6.
- Regezi JA, Kerr DA, Courtney RM. Odontogenic tumors: Analysis of 706 cases. J Oral Surg 1978;36:771-8.
- Landa LE, Hedrick MH, Nepomuceno-Perez MC, Sotereanos GC. Recurrent myxoma of the zygoma: A case report. J Oral Maxillofac Surg 2002;60:704-8.
- Halfpenny W, Verey A, Bardsley V. Myxoma of the mandibular condyle. A case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:348-53.
- Kim J, Ellis GL. Dental follicular tissue: Misinterpretation as odontogenic tumors. J Oral Maxillofac Surg 1993;51:762-7.
- Imai K, Koseki Y, Gamo M, Fujiki Y. Ten cases of myxoma (myxofibroma) of the jaws. Dentomaxillofac Radiol 1974;3:395-9.
- Deron PB, Nikolovski N, den Hollander JC, Spoelstra HA, Knegt PP. Myxoma of the maxilla: A case with extremely aggressive biologic behavior. Head Neck 1996;18:459-64.
- Peltola J, Magnusson B, Happonen RP, Borrman H. Odontogenic myxoma ? A radiographic study of 21 tumours. Br J Oral Maxillofac Surg 1994;32:298-302.
- Asaumi J, Konouchi H, Hisatomi M, Kishi K. Odontogenic myxoma of maxillary sinus: CT and MR-pathologic correlation. Eur J Radiol 2001;37:1-4.
- Carvalho de Melo AU, de Farias Martorelli SB, Cavalcanti PH, Gueiros LA, Martorelli Fde O. Maxillary odontogenic myxoma involving the maxillary sinus: Case report. Braz J Otorhinolaryngol 2008;74:472-5.
- Farman AG, Nortj� CJ, Grotepass FW, Farman FJ, Van Zyl JA.Myxofibroma of the jaws. Br J Oral Surg 1977;15:3-18.
- Abiose BO, Ajagbe HA, Thomas O. Fibromyxomas of the jawbones ? A study of ten cases. Br J Oral Maxillofac Surg 1987;25:415-21.
- Simon EN, Merkx MA, Vuhahula E, Ngassapa D, Stoelinga PJ. Odontogenic myxoma: A clinicopathological study of 33 cases. Int J Oral Maxillofac Surg 2004;33:333-7.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.