Risk of Surgical Site Infection (SSI) in Diabetes Mellitus Patients: Systematic Review and Meta-analysis
2 Medical Resident, Ministry Of Health, Riyadh City, Saudi Arabia
3 Medical Intern, Al-Qunfudhah University, Al-Qunfudhah City, Saudi Arabia
4 Medical Intern, Alfarabi Colleges of Medicine, Riyadh City, Saudi Arabia
5 General Practitioner, Batterjee Medical College, Jeddah City, Saudi Arabia
6 Medical Intern, King Khalid University, Khamis Mushait, Saudi Arabia
7 General Surgery, Dr. Suliman Al Habib Medical Group, Riyadh City, Saudi Arabia
Citation: Al-Mohawis LT, et al. Risk of Surgical Site Infection (SSI) in Diabetes Mellitus Patients: A Systematic Review and Meta-analysis. Ann Med Health Sci Res. 2021;11: 1199-1202.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Much has been published in current years about the impact of diabetes on increased rates of surgical site infection (SSI) and the potentially related impact of hyperglycemia on SSI. Surgical site infections are envisioned to have an annual financial impact of extra than 3 billion dollars nationally and are the largest contributor to the general value of healthcare-associated infections. Aim: This work aims to determine the risk of Surgical Site Infection (SSI) in Diabetes Mellitus (DM) patients. Materials and Methods: A systematic search was performed over different medical databases to identify sss studies, which studied the outcome of the SSI group versus the Non-SSI group of DM patients. Using the meta-analysis process, either with fixed or random-effects models, we conducted a meta-analysis on the prevalence of SSI in diabetic patients as a primary outcome, and on the risk of DM in SSI patients in comparison to non-SSI patients as a secondary outcome. Results: Ten studies were identified involving 78489 patients, with 3518 patients in the SSI group, and 74971 patients in the Non-SSI group. The meta-analysis process revealed a pooled prevalence of SSI in diabetic patients of 26.3%. Also, there was a highly significant increase in DM in the SSI group compared to the Non-SSI group (p = 0.01). Conclusion: To conclude, our results support the hypothesis of DM is an independent risk factor for SSIs for different surgical procedures. Awareness about DM control help to improve surgical outcomes for diabetic patients.
Keywords
Surgical site infection; Diabetes Mellitus
Introduction
Surgical site infection (SSI) is the second most common nosocomial infection, accounting for up to 40% of all healthcareassociated infections in the surgical population. Surgical site infections are the most common infections after colorectal surgical operation. Patients undergoing colon surgical operation represent a high-risk cohort for SSI because of inherent risk factors such as malnutrition, chronic immunosuppression, anemia, and an excessive prevalence of emergent surgery. [1]
Surgical site contamination (SSI) is one of the most serious complications following spinal surgery at some point in the early postoperative level. The prevalence of it was reported from 0.7% to 12.0%. SSI commonly requires surgical debridement and induces higher postoperative morbidity and mortality, calls for readmission, and effects in additional treatment costs. Also, it will delay the rehabilitation of patients and affect function healing of the spine. So, early identifying the risk factors for postoperative SSI and preventing them is helpful for patients’ rehabilitation after spinal surgery. [2]
Statistics from the national Healthcare safety network show that SSI rates vary by form of surgery. SSI rates are estimated to be 1.7% for abdominal hysterectomy and 0.9% for vaginal hysterectomy. However, in gynecologic oncology this rate stages from five% to thirty-five%. this alteration depends on several elements including high body mass index (BMI), low socioeconomic status, poor nutritional status, high intraoperative blood loss, prolonged operative time, the overall performance of bowel resection, perioperative blood transfusion, and patients’ other medical co-morbidities. [3]
Diabetes prevalence is increasing in the United States, and the appropriate control of patients with diabetes has become increasingly important for the prevention of hospital-acquired infections. Much has been published in current years about the impact of diabetes on increased rates of surgical site infection (SSI) and the potentially related impact of hyperglycemia on SSI. Surgical site infections are envisioned to have an annual financial impact of extra than 3 billion dollars nationally and are the largest contributor to the general value of healthcareassociated infections. [4]
This work aims to determine the risk of Surgical Site Infection (SSI) in Diabetes Mellitus (DM) patients.
Literature Review
Our review came following the (PRISMA) statement guidelines. [5]
Study eligibility
The included studies should be in English, a journal published article, and a human study describing DM patients. The excluded studies were non-English, or animal studies.
Study identification
Basic searching was done over the PubMed, Cochrane library, and Google scholar using the following keywords: Surgical Site Infection, Diabetes Mellitus.
Data extraction and synthesis
RCTs, clinical trials, and comparative studies, which studied the outcome of SSI group versus Non-SSI group of DM patients, will be reviewed.
Outcome measures included the prevalence of SSI in diabetic patients as a primary outcome and on the risk of DM in SSI patients in comparison to non-SSI patients as a secondary outcome.
Study selection
We found 327 records, 248 excluded based on title and abstract review; 79 articles are searched for eligibility by full-text review; 31 articles cannot be accessed; 29 studies were reviews and case reports; 10 were not describing functional outcome; leaving 9 studies that met all inclusion criteria.
Statistical analysis
After the pooling of data, Odds ratios (OR), Proportions (%), with 95% confidence intervals (CI) were calculated, using MedCalc statistical software (Belgium). After the Q test of heterogeneity, the I2-statistics (either the fixed-effects model or the random-effects model) were done within the meta-analysis process.
Results
The included studies were published between 2011 and 2020. Regarding the type of included studies, 1 studies (out of 9 studies) were prospective, while 8 studies were retrospective [Table 1]. [2,6-13]
| N | Author | Type of study |
Number of patients | Age (average years) |
Type of surgery | ||
|---|---|---|---|---|---|---|---|
| Total | SSI group | Non-SSI group | |||||
| 1 | George et al. [6] | Retrospective | 556 | 14 | 542 | 57.7 | Urologic surgery |
| 2 | Deierhoi et al. [7] | Retrospective | 5750 | 709 | 5041 | 65 | Colorectal surgery |
| 3 | Chaichana et al. [8] | Retrospective | 401 | 21 | 380 | 56.8 | Neurosurgery |
| 4 | Figuerola-Tejerina et al. [9] | Prospective | 1657 | 72 | 1585 | 70 | Cardiac Surgery |
| 5 | Krieger et al. [10] | Retrospective | 41375 | 1521 | 39854 | 30 | Cesarean surgey |
| 6 | Lai et al. [11] | Retrospective | 923 | 26 | 897 | 54 | Spine surgery |
| 7 | Gachabayov et al. [12] | Retrospective | 690 | 164 | 526 | 61 | Colorectal surgery |
| 8 | Liu et al. [2] | Retrospective | 256 | 64 | 192 | 58 | Spine surgery |
| 9 | Yang et al. [13] | Retrospective | 26881 | 927 | 25954 | -- | Orthopaedic surgery |
| #Studies arranged via publication year. | |||||||
| N | Author | Primary outcome | Secondary outcome | ||
|---|---|---|---|---|---|
| SSI prevalence | OR of DM | ||||
| SSI / DM patients | SSI group | Non-SSI group | |||
| 1 | George et al. [6] | 14 | 85 | 5 | 80 |
| 2 | Deierhoi et al. [7] | 709 | 1403 | 195 | 1208 |
| 3 | Chaichana et al. [8] | 21 | 54 | 5 | 49 |
| 4 | Figuerola-Tejerina et al. [9] | 72 | 432 | 36 | 396 |
| 5 | Krieger et al. [10] | 1521 | 4623 | 222 | 462 |
| 6 | Lai et al. [11] | 26 | 399 | 17 | 382 |
| 7 | Gachabayov et al. [12] | 35 | 112 | -- | -- |
| 8 | Liu et al. [2] | -- | -- | 16 | 25 |
| 9 | Yang et al. [13] | -- | -- | 188 | 1730 |
Table 2: Summary of outcome measures in all studies.
Each outcome was measured by:
Proportions (%)
• For the prevalence of SSI in diabetic patients.
Odds Ratio (OR)
• For risk of DM in SSI patients in comparison to non-SSI patients.
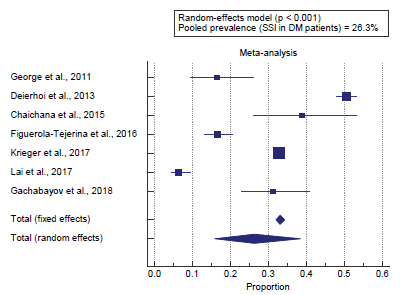
Concerning the primary outcome measure, we found 7 studies reported the prevalence of SSI in diabetic patients. I2 (inconsistency) was 99% with a highly significant heterogeneity Q test (p < 0.001), so random-effects model was carried out; with a pooled prevalence of SSI in diabetic patients = 26.3% (95% CI = 15.755 to 38.507). Using the random-effects model, the meta-analysis process revealed a pooled prevalence of SSI in diabetic patients of 26.3% (p < 0.01) [Figure 1].
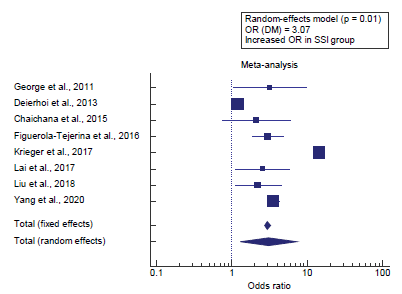
Concerning the secondary outcome measure, we found 8 studies reported DM in the SSI group compared to the Non-SSI group. I2 (inconsistency) was 98.4% with a highly significant Q test for heterogeneity (p < 0.0001), so random-effects model was carried out; with overall OR= 3.07 (95% CI = 1.304 to 7.243). Using the random-effects model, the meta-analysis process revealed a highly significant increase in DM in the SSI group compared to the Non-SSI group (p = 0.01) [Figure 2].
Discussion
This work aims to determine the risk of Surgical Site Infection (SSI) in Diabetes Mellitus (DM) patients.
The included studies were published between 2011 and 2020. Regarding the type of included studies, 1 studies (out of 9 studies) were prospective, while 8 studies were retrospective.
Regarding patients’ characteristics, the total number of patients in all the included studies was 78489 patients, with 3518 patients in the SSI group, and 74971 patients in the Non-SSI group. The mean age of all patients was (56.5 years).
A meta-analysis study was done on 9 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=78489).
We found 7 studies reported the prevalence of SSI in diabetic patients using the random-effects model, the meta-analysis process revealed a pooled prevalence of SSI in diabetic patients of 26.3% (p < 0.01). Which came in agreement with Bhakta et al., [1] Ghuman et al., [14] Akhter et al., [15] Al-Niaimi et al., [3] Klemencsics et al. [16] and Krieger et al. [10]
Bhakta et al. reported that a within-group analysis of the use of multivariable adjustment of the three diagnoses in question becomes used to research the independent variables associated with SSI. Only obesity, diabetes mellitus, and smoking were discovered to be significantly associated with SSI. For patients with colon most cancers, male sex, obesity, diabetes mellitus, smoking had been significantly associated with SSI. [1]
Ghuman et al. reported that, the results of univariate and multivariate analysis of potential SSI risk factors. Smoking, diabetes mellitus, and incision location were found to be significant factors with unadjusted odds ratios of 3.75 (p = 0.004), 2.75 (p = 0.009), and 1.37 (p = 0.03). [16]
Akhter et al. reported that a history of diabetes mellitus in patients conferred a much higher rate of SSIs, specifically, out of control serum glucose degrees inside the perioperative period, undiagnosed diabetes, and postoperative hyperglycemia inside forty-eight hours of surgical procedure had been related to a higher hazard of SSIs. [15]
Al-Niaimi et al. reported that surgical site infections have been and remain a cause of widespread postoperative morbidity and mortality inside the gynecologic oncology patient population. After controlling for perioperative antibiotic use, other studies have identified different independent hazard factors for SSI, including excessive BMI, perioperative blood transfusion, low socioeconomic status, and prolonged operative time, along with the presence of diabetes mellitus (DM). [3]
Klemencsics et al. reported that the prevalence of SSI was 3.5% and 3.9% in the test and the validation cohorts, respectively. The very last multivariable regression model predictive (p=.003) for SSI contained the patient’s age, body mass index (BMI), and the presence of 5 comorbidities, such as diabetes. [16]
Krieger et al. reported that the Pregnancies of patients who eventually developed SSI were more likely to have been complicated with hypertensive disorders of pregnancy, diabetes mellitus. [10]
Concerning the secondary outcome measure, we found 8 studies reported DM in the SSI group compared to the Non-SSI group. Using the random-effects model, the meta-analysis process revealed a highly significant increase in DM in the SSI group compared to the Non-SSI group (p = 0.01). Which came in agreement with Boreland et al., [17] Martin et al., [4] Akhter et al., [15] Liu et al. [2] and Meng et al. [18]
Boreland et al. reported that Serum glucose ranges > 200 mg/ dL in the instant (<48 h) postoperative period contribute to an elevated threat of surgical site infections. Poor glycemic control previous to surgical operation contributes to poor control after hospital discharge and increases the prevalence of complications such as poor wound healing and higher rates of surgical site infections, and in the end readmission to the health facility and elevated mortality. [17]
Martin et al. reported that the overall estimate for the association between elevated blood glucose and SSI in the pre-or intraoperative period was OR= 1.88. The overall estimate for the association between elevated blood glucose in the post-operative period and SSI was 1.45. [4]
Akhter et al. reported that incidence in patients ≥50 years old was 17.8% higher than those <50 years of age (8.9%). Patients with diabetes mellitus were found to have a significantly higher incidence of SSIs of 21.1% com¬pared with non-diabetics (8.7%). [15]
Liu et al. reported that the finding of diabetes mellitus as a risk issue for SSI was consistent with previous research. Diabetes could result in microangiopathic alternates and end in local tissue ischemia, which finally delayed the wound healing. Furthermore, the immune feature in a patient with diabetes was suppressed and it would impair the wound healing. Preoperative high serum glucose was also determined to be a hazard factor for SSI. The reasons for it were similar to those in affected persons with diabetes mellitus. [2]
Meng et al. reported that they searched the PubMed, Embase, and Cochrane library databases, and identified 25 case-control studies. The pooled results revealed that the major factors associated with infection were diabetes mellitus (OR 2.04). [18]
Conclusion
To conclude, our results support the hypothesis of DM is an independent risk factor for SSIs for different surgical procedures. Awareness about DM control helps to improve surgical outcomes for diabetic patients.
Competing Interests
The authors declare that they have no competing interests. All the listed authors contributed significantly to the conception and design of study, acquisition, analysis, and interpretation of data and drafting of the manuscript, to justify authorship.
REFERENCES
- Bhakta A, Tafen M, Glotzer O, Ata A, Chismark AD, Valerian BT, et al. Increased incidence of surgical site infection in IBD patients. Dis Colon Rectum. 2016;59:316-322.
- Liu J-M, Deng H-L, Chen X-Y, Zhou Y, Yang D, Duan M-S, et al. Risk factors for surgical site infection after posterior lumbar spinal surgery. Spine 2018;43:732-737.
- Al-Niaimi AN, Ahmed M, Burish N, Chackmakchy SA, Seo S, Rose S, et al. Intensive postoperative glucose control reduces the surgical site infection rates in gynecologic oncology patients. Gynecol Oncol. 2015;136:71-76.
- Martin ET, Kaye KS, Knott C, Nguyen H, Santarossa M, Evans R, et al. Diabetes and risk of surgical site infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2016;37:88-99.
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. Bmj 2009;339.
- George AK, Srinivasan AK, Cho J, Sadek MA, Kavoussi LR. Surgical site infection rates following laparoscopic urological procedures. J Urol. 2011;185:1289-1293.
- Deierhoi RJ, Dawes LG, Vick C, Itani KM, Hawn MT. Choice of intravenous antibiotic prophylaxis for colorectal surgery does matter. J Am Coll Surg. 2013;217:763-769.
- Chaichana KL, Kone L, Bettegowda C, Weingart JD, Olivi A, Lim M, et al. Risk of surgical site infection in 401 consecutive patients with glioblastoma with and without carmustine wafer implantation. Neurol Res. 2015;37:717-726.
- Figuerola-Tejerina A, Rodríguez-Caravaca G, Bustamante-Munguira J, San Román-Montero JM, Durán-Poveda M. Epidemiological Surveillance of Surgical Site Infection and its Risk Factors in Cardiac Surgery: A Prospective Cohort Study. Rev Esp Cardiol. 2016;69:842-848.
- Krieger Y, Walfisch A, Sheiner E. Surgical site infection following cesarean deliveries: trends and risk factors. J Matern.-Fetal Neonatal Med. 2017;30:8-12.
- Lai Q, Song Q, Guo R, Bi H, Liu X, Yu X, et al. Risk factors for acute surgical site infections after lumbar surgery: a retrospective study. J Orthop Surg Res. 2017;12:116.
- Gachabayov M, Senagore AJ, Abbas SK, Yelika SB, You K, Bergamaschi R. Perioperative hyperglycemia: an unmet need within a surgical site infection bundle. Tech Coloproctol. 2018;22:201-207.
- Yang J, Zhang X, Liang W. A retrospective analysis of factors affecting surgical site infection in orthopaedic patients. J Int Med Res. 2020;48:0300060520907776.
- Ghuman A, Chan T, Karimuddin AA, Brown CJ, Raval MJ, Phang PT. Surgical site infection rates following implementation of a colorectal closure bundle in elective colorectal surgeries. Dis Colon Rectum. 2015;58:1078–1082.
- Akhter MSJ, Verma R, Madhukar KP, Vaishampayan AR, Unadkat PC. Incidence of surgical site infection in postoperative patients at a tertiary care centre in India. J Wound Care. 2016;25:210-217.
- Klemencsics I, Lazary A, Szoverfi Z, Bozsodi A, Eltes P, Varga PP. Risk factors for surgical site infection in elective routine degenerative lumbar surgeries. Spine J. 2016;16:1377-1383.
- Boreland L, Scott-Hudson M, Hetherington K, Frussinetty A, Slyer JT. The effectiveness of tight glycemic control on decreasing surgical site infections and readmission rates in adult patients with diabetes undergoing cardiac surgery: a systematic review. Heart & Lung. 2015;44:430-440.
- Meng J, Kang Y, Cheng H, Gu Y, Zhang X, Wang S. Misdiagnosed ovarian Krukenberg tumor during pregnancy with virilization. European Gynecol Oncol. 2016;37:587-590.
Select your language of interest to view the total content in your interested language
Awards Nomination
20+ Million Readerbase
Google Scholar citation report
Citations : 24805
Annals of Medical and Health Sciences Research received 24805 citations as per google scholar report
Annals of Medical and Health Sciences Research peer review process verified at publons
Indexed in
PubMed Central Index Copernicus Emerging Sources Citation Index
Abstracted/Indexed in
- Include Baidu Scholar
- CNKI (China National Knowledge Infrastructure)
- EBSCO Publishing's Electronic Databases
- Exlibris – Primo Central
- Google Scholar
- Hinari
- Infotrieve
- National Science Library
- ProQuest
- TdNet
- African Index Medicus
 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.