Role of Antifungal in Management of Leukoplakia: A Retrospective Study
2 Department of Oral Medicine and Radiology, Saveetha Dental College and Hospital ,Saveetha Institute of Medical and Technical Sciences, Chennai, India, Email: jayanthkumar@saveetha.com
Received: 31-Aug-2021 Accepted Date: Sep 13, 2021 ; Published: 20-Sep-2021
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Oral leukoplakia is one of the most common potentially malignant disorders seen in our Indian Subcontinent. It is present in relation to the consumption of tobacco products, mainly smoking. The most common site for the occurrence of leukoplakia is the buccal mucosa. There is a hypothesis that red component of leukoplakia may be attributed to the fungal hyphae. The aim of this study was to analyze the management of leukoplakia using antifungal drug. The study picked out 99 leukoplakia patients from the 89000 cases of leukoplakia case sheets available. The study sample consisted of 94 male and 5 females with leukoplakia. The majority of the patients were in the age of 40-50 years with a mean of 48.66 years. The study sample had 77 homogenous variants and 22 non-homogenous variants. The vast majority of patients were males with the homogenous variant. However gender based analysis showed no association (P>0.05). An association analysis shows that there is no statistically significant association between the usage of antifungals in leukoplakia and the clinical variant (P>0.05). As a conclusion, within the limitations of the study, antifungal were used to a limited extent in the management of leukoplakia which implies that there was a limited chance of super added fungal infection.
Keywords
Antifungal; Homogenous lesion; Leukoplakia
Introduction
An important key to general health and overall quality of life is oral health. It has the potential to impact on overall quality of life. [1,2] Poor oral hygiene in the form of dental caries or poor periodontal health has been an important contributor for several mucosal diseases. [3,4] Oral leukoplakia has been defined as a predominantly white lesion of the oral mucosa that cannot be characterized as another definable lesion. It belongs to the category of oral potentially malignant disorders. [5,6] OPMDS are considered as the early tissue changes that happen due to various habits such as smoking tobacco, chewing tobacco or stress. [5,7] The OPMDS are associated with salivary changes and also genetic changes which can predispose to the development of a malignancy. [8,9] They have also been known to coexist with other potentially malignant disorders such as actinic cheiloisis. [10]
Elderly males in the age range of 35-45 years are affected most commonly. In India, it is 0.2%-4.9% prevalent, with buccal mucosa and commissures as the most common site, followed by lips, tongue, palate, alveolar ridge, gingiva, soft palate and floor of the mouth. [5,11] Leukoplakia, one of the most common white lesions encountered by the dentists and still holds an enigma around itself. Proper recognition of the type of leukoplakia helps in successful treatment of the lesion. [12] Hence, it is important for the dentist to identify the type of leukoplakia as it can help in treatment planning and also in predicting the malignant potential of the lesion. [13] Leukoplakia shows histological characteristics like epithelial hyperplasia, and/or hyperkeratosis, with or without epithelial dysplasia or carcinoma. Oral leukoplakia can be divided into simple homogenous leukoplakia and non- homogenous variant. The homogenous lesions are thin, flat and have predominant white plaque with a very poor potential to transform into malignant. Non homogenous leukoplakia has a higher risk of dysplastic transformation. [14,10]
This includes speckled leukoplakia, mix white and red lesion, nodular leukoplakia, verrucous leukoplakia that usually shows rough corrugated surfaces. [15] Chronic hyperplastic candidiasis or candidal leukoplakia is a variant of oral candidosis that typically presents as a white patch on the oral mucosa commissures. The major etiologic agent of the disease is the oral fungal pathogen Candida predominantly belonging to Candida albicans, although other systemic co-factors, such as vitamin deficiency and generalized immune suppression, may play a contributory role. Clinically, the lesions do not present with symptoms and regress after proper antifungal therapy and correction of underlying nutritional or other deficiencies if lesion is left untreated, a small number show dysplastic changes and develop into carcinomas. Malignancy is characterized by three; anaplasia, invasiveness, and metastasis. [16,17]
The mainstay in the treatment of leukoplakia is by habit cessation and the administration of antioxidants. Vitamin A has an inhibitory effect on inflammation and epithelial proliferation. [18,19] Leukoplakia, candidiasis, lichen planus, white spongy nevus, lupus erythematosus, andmorsicatio buccarum are the most important white lesions in the differential diagnosis of oral cancer. [20] Previously our team has a rich experience in working on various research projects across multiple disciplines. [21-35] Now the growing trend in this area motivated us to pursue this project. The aim of this article was to study the usage of antifungals in the management of oral leukoplakia. The objectives were to see if any particular variant of leukoplakia had any usage of antifungals and any particular gender had the usage of antifungals.
Materials and Methods
The archived patient records of the department of oral medicine and radiology, Saveethadental college were collected and the data was assessed from the time period of June 2019-April 2020. From the record of 86000 cases, all known cases of leukoplakia were picked up. Ethical clearance was obtained from the institutional ethics committee of Saveetha dental college. The Cross checking of data including digital entry and intra oral photographs was done by an additional reviewer The main advantages of this study were that the data was all pre-validated and the main disadvantages were that it was an unicentric study and only a single ethnicity of the population was studied. The selected samples were examined by three people; 1 reviewer, 1 guide and 1 researcher the patient data were picked up from the case sheets and the variables recorded were the age, gender, tobacco usage type and the site of the lesion. The data was randomly cross verified by either recalling the patients or having telephonic conversations with the patient.
The internal validity of the study was established as the data was collected from a verifiable and standardised database. The external validity is established as the data is from a clinical setup which is duplicable. A pretested format was used to record the data. Data analysis was done using SPSS PC Version 23.0 (IBM, 2016) software for statistics. Both independent and dependent variables were recorded and analysed. The final statistical analysis included means to find out if there was correlation between usages of antifungal drug in the management of leukoplakia using Chi-square test with significance level at 0.05.
Results and Discussion
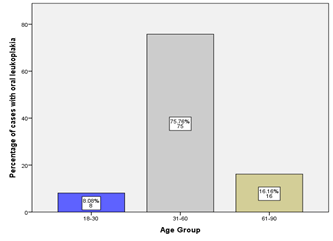
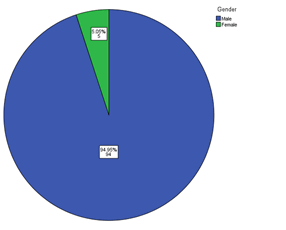
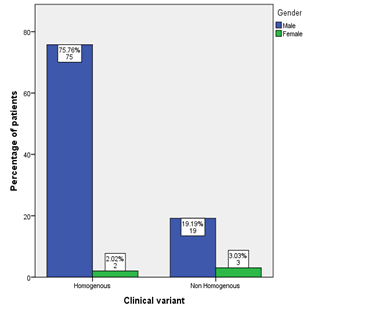
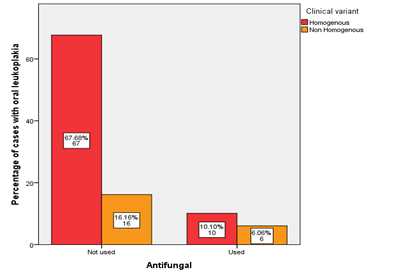
On analysis of the collected data it was found that there were 99 patients who had reported with oral leukoplakia during the time period of June 2019 to March 2020. The age of the patients ranged from 18-84 years [Figure 1]. A gender analysis reveals that 95(95.95%) of them are males and 4(4.04%) are females [Figure 2]. It is consistent with the fact that males have a predominant usage of tobacco habit. Study population consisted of 99 patients totally, divided in homogenous variant and non-homogenous variant. In this study it was observed that there was 77 homogenous variant of leukoplakia and 22 non- homogenous variant of leukoplakia. However, no association could be made out between the gender and the variant (P>0.05) [Figure 3]. There is no significant association between the usage of antifungals and clinical variant of leukoplakia (P>0.05) [Figure 4].
Figure 3:A bar graph showing the association between the clinical variant of leukoplakia and the gender. X axis represents the clinical variant; Y axis represents the percentage of cases. The majority of the patients were of the homogenous type. A chi-square association was done (chi-square-3.524, df-1, p-0.06 (p>0.05) which shows there was no statistically significant association between the gender and clinical variant.
Figure 4:Bar graph showing the association between the usage of antifungals and the clinical variant of leukoplakia. X axis denotes the usage of antifungal and Y axis denotes the percentage of cases with oral leukoplakia. Antifungals were not used in a majority of patients. A chi-square association was done (chi-square-2.336, df-1, p-0.202 (p>0.05)) which shows there was no statistically significant association between the usage of antifungals and variant of leukoplakia.
There are several studies which show an associated Candida albicans infection in patients with oral leukoplakia, and it has been suggested that some clinical variant of leukoplakia are the result of invasion by hyphae of Candida Albicans. [36] Candidiasis is known to be a common oral mycotic infection which manifests in many different forms. It is also a normal commensal of the oral cavity. [37] An important factor contributing to infection of candida in leukoplakia is the breach of integrity of oral mucosa. Cancer of the oral cavity is found to develop in 9%–40% of candidal leukoplakias compared with the 2%–6% risk of malignant transformation for leukoplakias in general.[38]
In this study it was observed that a total of 99 patients were used as study samples with 99.9% males and 5.1% females. Among the 99 patients/ homogenous variants of leukoplakia was 77.8% and non-homogenous variants was 22.2%. In the management of leukoplakia, among 16.2% of the study population, n 16.2% antifungal drug was used as a way of management while the remaining 83.8% of the samples, antifungal drug was not used as a therapy.
According to a study done by Cornea et al, it is reported that oral leukoplakias were associated with candida infection. [7,8] similarly in another study by Mehta at al it was found that 7%-50% of the leukoplakias have been found to be associated with candida hyphae [9] Candida infection seen was in 47% of patients with oral leukoplakia according to a study by Dilhari et al. Candida albicans, which is 97.7% was the most common type of candida species followed by Candida tropicalis which was 5.3% Majority of candida–infected lesions were seen in the buccal; mucosa region. [10] According to a study done by Wu et al. the results revealed that 59 patients which are 15.9 % with oral leukoplakia were infected by candida the tongue was 66.1%.
Antifungals are not just used to treat candidiasis but also have been used to manage several other OPMDS like Actinic cheilosis etc., [10] an early management of leukoplakia is needed to prevent a malignant transformation and distant metastasis. [2,18] Our institution is passionate about high quality evidence based research and has excelled in various fields. [39-45] We hope this study adds to this rich legacy.
Limitations include data may have discrepancies and are limited to one geographic area. Future scope, larger scope of exploration in regards with leukoplakia with a more widely carried out study in different parts of the world not just confined to a single geographical location. Though the study is from a single patient database, there have been several studies done in the past from the same database which has given very conclusive results. [12,46]
Conclusion
Within the limitations of the study we find that antifungals have not been significantly used in the management of leukoplakia. There is no gender specific or variant specific association between the usages of antifungals in the management of leukoplakia. This implies that the super added candidal infection is not seen in cases of leukoplakia.
REFERENCES
- Ruff RR, Sischo L, Broder HL. Minimally important difference of the child oral health impact profile for children with orofacial anomalies. Health Qual Life Outcomes. 2016;14:140.
- Misra SR, Shankar YU, Rastogi V, Maragathavalli G. Metastatic hepatocellular carcinoma in the maxilla and mandible, an extremely rare presentation. Contemp Clin Dent. 2015;6:S117–21.
- Subashri A, Maheshwari TN. Knowledge and attitude of oral hygiene practice among dental students. Research J. Pharm. and Tech. 2016; 9:1840–1842.
- Rohini S, Kumar VJ. Incidence of dental caries and pericoronitis associated with impacted mandibular third molar-A radiographic study. Research J Pharm Tech. 2017;10:1081–1084.
- Steele JC, Clark HJ, Hong CHL, Jurge S, Muthukrishnan A, Ross Kerr A, et al. World workshop on oral medicine VI: An international validation study of clinical competencies for advanced training in oral medicine. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:143-151.
- Dharman S, Muthukrishnan A. Oral mucous membrane pemphigoid–Two case reports with varied clinical presentation. J Indian Soc Periodontol. 2016;20:630-634.
- Chaitanya NC, Muthukrishnan A, Krishnaprasad CMS, Sanjuprasanna G, Pillay P, Mounika B. An insight and update on the analgesic properties of vitamin C. J Pharm Bioallied Sci. 2018;10:119–125.
- Venugopal A, Uma Maheswari TN. Expression of matrix metalloproteinase-9 in oral potentially malignant disorders: A systematic review. J Oral Maxillofac Pathol. 2016;20:474–479.
- Maheswari TNU, Venugopal A, Sureshbabu NM, Ramani P. Salivary micro RNA as a potential biomarker in oral potentially malignant disorders: A systematic review. Ci Ji Yi Xue Za Zhi. 2018;30:55–60.
- Muthukrishnan A, Kumar LB. Actinic cheilosis: Early intervention prevents malignant transformation. BMJ Case Reports. 2017;20.
- Muthukrishnan A, Kumar LB, Ramalingam G. Medication-related osteonecrosis of the jaw: A dentist’s nightmare. BMJ Case Reports. 2016.
- Subha M, Arvind M. Role of magnetic resonance imaging in evaluation of trigeminal neuralgia with its anatomical correlation. Biomed Pharmacol. 2019;12:289-296.
- Patil SR, Yadav N, Al-Zoubi IA, Maragathavalli G, Sghaireen MG, Gudipaneni RK, et al. Comparative study of the efficacy of newer antioxitands lycopene and oxitard in the treatment of oral submucous fibrosis. Pesquisa Brasileiraem Odontopediatria e Clínica Integrada. 2018;18:1–7.
- Muthukrishnan A, Warnakulasuriya S. Oral health consequences of smokeless tobacco use. Indian J Med Res. 2018;148:35.
- Choudhury P. Vanishing roots: First case report of idiopathic multiple cervico–apical external root resorption. J Clin Diagn Res. 2015;9:17-19.
- Chattopadhyay A, Caplan DJ, Slade GD, Shugars DC, Tien H-C, Patton LL. Incidence of oral candidiasis and oral hairy leukoplakia in HIV-infected adults in North Carolina. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:39-47.
- Sanjaya PR, Gokul S, GururajPatil B, Raju R. Candida in oral pre-cancer and oral cancer. Med Hypotheses. 2011;77:1125–1128.
- Chaitanya NC, Muthukrishnan A, Babu DBG, Kumari CS, Lakshmi MA, Palat G, et al. Role of vitamin E and vitamin A in oral mucositis induced by cancer chemo/radiotherapy- A meta-analysis. J Clin Diagn Res. 2017;11:ZE06–ZE09.
- Mogavero A, Maiorana MV, Bertan C, Bozzi F, Pierotti MA, Gariboldi M. Abstract 1161: Metformin has an inhibitory effect on cell proliferation but does not induce death in colorectal cancer. Molecular and Cellular Biology. 2015.
- Komori A, Welton WA, Kelln EE. The behavior of the basement membrane of skin and oral lesions in patients with lichen planus, erythema multiforme, lupus erythematosus, pemphigus vulgaris, benign mucous membrane pemphigoid, and epidermolysis bullosa. Oral Surg Oral Med Oral Pathol. 1966;22:752–763.
- Ponnulakshmi R, Shyamaladevi B, Vijayalakshmi P, Selvaraj J. In silico and in vivo analysis to identify the antidiabetic activity of beta sitosterol in adipose tissue of high fat diet and sucrose induced type-2 diabetic experimental rats. Toxicol Mech Methods. 2019;29:276–290.
- Mathew MG, Samuel SR, Soni AJ, Roopa KB. Evaluation of adhesion of Streptococcus mutans, plaque accumulation on zirconia and stainless steel crowns, and surrounding gingival inflammation in primary molars: randomized controlled trial. Clin Oral Investig. 2020;24:3275–3280.
- Subramaniam N, Muthukrishnan A. Oral mucositis and microbial colonization in oral cancer patients undergoing radiotherapy and chemotherapy: A prospective analysis in a tertiary care dental hospital. J Investig Clin Dent. 2019;10:e12454.
- Girija ASS, Shankar EM, Larsson M. Could SARS-CoV-2-Induced hyperinflammation magnify the severity of coronavirus disease (Covid-19) Leading to acute respiratory distress syndrome? Front Immunol. 2020;11:1206.
- Dinesh S, Kumaran P, Mohanamurugan S, Vijay R, Singaravelu DL, Vinod A, et al. Influence of wood dust fillers on the mechanical, thermal, water absorption and biodegradation characteristics of jute fiber epoxy composites. J Polym Res. 2020;27.
- Thanikodi S, Singaravelu D Kumar, Devarajan C, Venkatraman V, Rathinavelu V. Teaching learning optimization and neural network for the effective prediction of heat transfer rates in tube heat exchangers. Therm Sci. 2020;24:575–581.
- Murugan MA, Jayaseelan V, Jayabalakrishnan D, Maridurai T, Kumar SS, Ramesh G, et al. Low velocity impact and mechanical behaviour of shot blasted SiC wire-mesh and silane-treated aloevera/hemp/flax-reinforced SiC whisker modified epoxy resin composites. Silicon Chem. 2020; 12:1847–1856.
- Vadivel JK, Govindarajan M, Somasundaram E, Muthukrishnan A. Mast cell expression in oral lichen planus: A systematic review. J Investig Clin Dent. 2019;10:e12457.
- Chen F, Tang Y, Sun Y, Veeraraghavan VP, Mohan SK, Cui C. 6-shogaol, an active constiuents of ginger prevents UVB radiation mediated inflammation and oxidative stress through modulating NrF2 signaling in human epidermal keratinocytes (HaCaT cells). J Photochem Photobiol B. 2019;197:111518.
- Manickam A, Devarasan E, Manogaran G, Priyan MK, Varatharajan R, Hsu C-H, et al. Score level based latent fingerprint enhancement and matching using SIFT feature. Multimed Tools Appl. 2019;78:3065–3085.
- Wu F, Zhu J, Li G, Wang J, Veeraraghavan VP, Krishna Mohan S, et al. Biologically synthesized green gold nanoparticles from induce growth-inhibitory effect on melanoma cells (B16). Artif Cells Nanomed Biotechnol. 2019;47:3297–3305.
- Ma Y, Karunakaran T, Veeraraghavan VP, Mohan SK, Li S. Sesame inhibits cell proliferation and induces apoptosis through inhibition of STAT-3 translocation in thyroid cancer cell lines (FTC-133). Biotechnol Bioprocess Eng. 2019;24:646–652.
- Ponnanikajamideen M, Rajeshkumar S, Vanaja M, Annadurai G. In vivo type 2 diabetes and wound-healing effects of antioxidant gold nanoparticles synthesized using the insulin plant Chamaecostus cuspidatus in albino rats. Can J Diabetes. 2019;43:82–96.
- Vairavel M, Devaraj E, Shanmugam R. An eco-friendly synthesis of Enterococcus sp.-mediated gold nanoparticle induces cytotoxicity in human colorectal cancer cells. Environ Sci Pollut Res Int. 2020;27:8166–8175.
- Paramasivam A, VijayashreePriyadharsini J, Raghunandhakumar S. N6-adenosine methylation (m6A): A promising new molecular target in hypertension and cardiovascular diseases. Hypertens Res. 2020;43:153–154.
- Cheng R, Li D, Shi X, Gao Q, Wei C, Li X, et al. Reduced CX3CL1 secretion contributes to the susceptibility of oral leukoplakia-associated fibroblasts to Candida albicans. Front Cell Infect Microbiol. 2016;6:150.
- Bhateja S, Aggarwal N, Arora G, Yasmin T. Candidiasis - The most common fungal infection of oral cavity. Biomedical Journal of Scientific and Technical Research. 2018;8:6487-6491.
- Scully C, EI-Kabir M, Samaranayake LP. Candida and oral candidosis: A review. Crit Rev Oral Biol Med. 1994;5:125–157.
- Vijayashree PJ. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol. 2019;90:1441–1448.
- Ezhilarasan D, Apoorva VS, Ashok Vardhan N. Syzygiumcumini extract induced reactive oxygen species-mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med. 2019;48:115–121.
- Ramesh A, Varghese S, Jayakumar ND, Malaiappan S. Comparative estimation of sulfiredoxin levels between chronic periodontitis and healthy patients - A case-control study. J Periodontol. 2018;89:1241–1248.
- Mathew MG, Samuel SR, Soni AJ, Roopa KB. Evaluation of adhesion of Streptococcus mutans, plaque accumulation on zirconia and stainless steel crowns, and surrounding gingival inflammation in primary molars: Randomized controlled trial. Clin Oral Investig. 2020;24:3275-3280.
- Sridharan G, Ramani P, Patankar S, Vijayaraghavan R. Evaluation of salivary metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Oral Pathol Med. 2019;48:299–306.
- Pc J, Marimuthu T, Devadoss P. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin Implant Dent Relat Res. 2018;20:531-534.
- Ramadurai N, Gurunathan D, Samuel AV, Subramanian E, Rodrigues SJL. Effectiveness of 2% Articaine as an anesthetic agent in children: Randomized controlled trial. Clin Oral Investig. 2019;23:3543–3550.
- Patil SR, Maragathavalli G, Araki K, Al-Zoubi IA, Sghaireen MG, Gudipaneni RK, et al. Three-rooted mandibular first molars in a Saudi Arabian population: A CBCT study. Pesqui Bras Odontopediatria Clin Integr. 2018;18:4133.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.