Role of MRI in Staging Urinary Bladder Tumors
Citation: Mehraj A, et al. Role of MRI in Staging Urinary Bladder Tumours. Ann Med Health Sci Res. 2017; 7: 116-121
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Accurate preoperative evaluation of proven bladder carcinoma is important because therapy depends on the clinical stage of the disease. Various imaging modalities have been used for such staging, and as such there is a need to look for the single best modality. Aim and objective: To determine the sensitivity, specificity and overall accuracy of MRI in staging urinary bladder carcinoma, and to evaluate its role in making comparison between superficial vs. invasive tumors and organ confined vs. non organ confined tumors. Material and Methods: This prospective study was undertaken on 25 patients of proven bladder carcinoma who were candidates for radical cystectomy. They were investigated in a sequential manner which included all routine investigations beside transabdominal ultrasonography, cystoscopy and biopsy (TUR / cystoscopic) and magnetic resonance imaging (MRI). Radical cystectomy was performed in all patients. MRI staging was correlated with the pathologic staging. Results: Analysis of our results revealed a highly significant (P<-0.001) MRI accuracy of 96% for deep muscle invasion, 84% accuracy for perivesical fat invasion and 84% accuracy of MRI detection of lymph node metastases. However, 88% accuracy of MRI for contiguous organ involvement was found to be of relatively lower significance (P<-0.05). Overall accuracy of MRI in the staging of bladder carcinoma was 60% with an overestimation of the tumor in 20% patients and an underestimation in 20% patients. Conclusion: MRI is an efficient non-invasive modality for imaging of bladder anatomy and bladder carcinoma. It has a high accuracy, sensitivity and specificity for differentiating invasive from noninvasive bladder carcinoma, and determining the involvement of adjacent organs. A larger prospective study is however, required for determining the exact role of MRI in the staging of bladder carcinoma.
Keywords
MRI; Urinary bladder; Carcinoma; Staging
Introduction
Urinary bladder cancer ranks 9th in worldwide cancer incidence. It is the 7th most common malignancy in men and the 17th most common in women. [1] Bladder carcinoma accounts for 5.6% of cancer in males and 1.8% of cancer in females in India, with an actual crude rate (ACR) incidence of about 1 in 174 men and 1 in 561 women. [2] A detailed study of the bladder cancer cases registered from 2005 to 2010 in our tertiary care hospital revealed that bladder cancer ranks as the 7th leading cancer and accounts for 5.9% of all prevalent cancers in the Kashmiri population. [3]
Magnetic resonance imaging gives an excellent insight into the anatomy and pathology of urinary bladder as it provides high fluid-tissue contrast resolution and clearly delineates urinary bladder musculature. Its multi planar capacity allows depiction of complex pelvic anatomic relationships. This gives improved characterization of urinary bladder abnormalities and more accurate demonstration of the extent of luminal, mural and perivesical pathology. Although transabdominal and transvaginal ultrasound are the techniques employed for the initial investigation of pelvic pathology and are usually sufficient for evaluation of benign disease, with MRI being used for problem-solving; MRI has become invaluable in the evaluation of malignant disease within the pelvis. [4]
Aims and Objectives
To compare preoperative MRI findings with the final diagnosis and staging after surgical exploration and histopathological examination of the retrieved surgical specimen in terms of its:
• Sensitivity
• Specificity
• Overall Accuracy
To evaluate the role of MRI in making comparison between
• Superficial v/s invasive tumors.
• Organ confined v/s non organ confined tumours.
Materials and Methods
This prospective study was carried out at the Department of Urology and Department of Radio diagnosis and Imaging, Sher-i- Kashmir Institute of Medical Sciences, Soura, Srinagar, Kashmir for a period of 2 years.
Protocol
All patients presenting with bladder mass on clinical examination and / or radiological investigations were subjected to the following steps.
STEP 1: Clinical and radiological evaluation
Prior to imaging a thorough and accurate clinical history and examination is essential. Recent endoscopic procedures give rise to hemorrhage and edema which can give a misleading appearance on MRI, so history about any intervention was sought. MRI was done after three weeks gap of any invasive procedure on the urinary tract.
MRI was performed with a super conductive magnet system (Magneton Avanto, Tim 76 × 18, Siemens) operating at 1.5 Tesla using body coils. The patients were kept with a moderately full bladder. Adequate distension of urinary bladder improves evaluation of the wall and visualization of focal lesions. Over distension, not only results in patient discomfort and restlessness during the examination causing the patient to move, but may also cause small focal lesions to go undetected due to stretching. Patients were kept in supine position. Urinary catheters, if any, were clamped before the examination to ensure sufficient bladder filling.
T1 weighted and T2 weighted spin echo sequences are the mainstay of bladder imaging. T1 weighted spin echo sequences and a multi section technique was used with repetition times (TRs) ranging from 500 to 700 msec and echo times (TEs) of 10 to 16 msec (TR/TE=500-700/10-16). T2 weighted spin echo sequences were taken with TR/TE of 2200-5000/20-100. The section thickness in axial, saggital and coronal views were set at 5mm with 2 mm spacing. In most of the cases, 1 ampoule (0.1 mmole per kg of body weight) amounting to 100 ml of Gadolinium diethylene tri amine penta acetic acid (Gd-DTPA; Omniscan,) was injected intravenously. Axial post contrast T1 weighted images were then taken immediately to catch the images during the tumor enhancement phase before the contrast appeared in the urine. Saggital and coronal views were added if the tumor was situated in the dome or the bladder base. Axial and coronal large field of vision (typically 38 – 49) T1 weighted images of the abdomen and pelvis were taken in order to evaluate the upper abdominal viscera, particularly the kidneys for the presence of hydronephrosis and to identify any lymph node enlargement and bone metastases.
Following MRI findings were noted by two experienced radiologists
• Depth of urinary bladder wall invasion
• Presence of extravesical extension
• Presence of local invasion e.g. prostate, seminal vesicles, rectum, pelvis side walls, uterus, vagina, intestines, etc
• Presence of lymph node invasion and evaluation of the size and number of involved nodes
Finally a TNM staging was done on the basis of MRI findings.
STEP 2: Treatment and pathological assessment
After getting the MRI of 34 patients done, 9 patients were excluded from the study. Among these, 5 patients had very advanced lesions in the bladder, and hence were not fit for surgery, 3 patients had early disease and 1 patient did not give consent for surgery.
A histological diagnosis was obtained in all the patients prior to surgery. All the 25 patients included in the study underwent radical cystectomy with various types of diversions. Intra operative findings were noted and compared with MRI findings. The resected specimens were preserved and sent for histopathological examination. The pathological examination included examination of the urinary bladder and other excised organs, lower ureters, prostate, seminal vesicles and posterior urethra in males or lower ureters, urethra, uterus with its appendages and anterior vaginal wall (or whole vagina) in females. Pathological examination of the perivesical tissue and thorough examination of all the lymph nodes was carried out. Finally a TNM staging was done on histological basis.
STEP 3: Comparison of the findings from pathological examination to the MRI examination
The histopathological staging was finally correlated with MRI staging, and accuracy, specificity and sensitivity of MRI in the staging of bladder carcinoma was determined.
Observations
A total of twenty five patients of urinary bladder carcinoma who were candidates for radical cystectomy were included in the study. Nine other patients who underwent MRI of urinary bladder were excluded from the study due to various reasons. Following observations were made during the study. Out of twenty five patients, 22 (88%) were males and 3 (12%) were females. Age of the patients ranged from 32 to 68 years. Majority of the patients were above 60 years of age (32%). Hematuria was the most common presenting symptom among the studied patients; 23(88%) patients presented with this symptom. The other symptoms included LUTS in 4 (16%), Pain abdomen in 5 (20%) and Acute urinary retention in 3 (12%) patients. Routine investigations like CBC, LFT, KFT, ECG and X-ray chest were mostly unremarkable in all patients. Microscopic examination of urine confirmed the presence of hematuria in all the 25 (100%) patients while only 11 (44%) patients showed presence of malignant cells in urine. Transabdominal ultrasonography was carried out in all the studied patients in order to document the initial evidence of urinary bladder tumor, besides ruling out distant abdominal metastasis. There was no evidence of distant metastases to Liver and Para aortic lymph nodes in any patient, and none of the patients had ascites. Besides this, transabdominal ultrasonography was also used to evaluate the genitourinary system. Hydroureteronephrosis was detected in 6(24%) patients on right and 6(24%) patients on left side. In all 25 patients ultrasound detected masses at various locations in the bladder. Tumor size varied from 10 mm to 100 mm. In 15(60%) patients, there were multiple masses within the bladder, while in 10(40%) patients there was a single mass. Prostate was enlarged in 10(45.45%) out of 22 male patients, but showed tumor infiltration in none. Seminal vesicles were normal in all the male patients.
All patients underwent Cystoscopy and showed the presence of bladder tumor which was situated on the posterior wall in 11 (44%) patients, left lateral wall in 6 (24%), right lateral wall in 3 (12%), left posterolateral wall in 5 (20%),right posterolateral wall in 4 (16%), anterior wall in 2 (8%),left anterolateral wall in 2 (8%),right anterolateral wall in 1 (4%),trigone in 3 (12%),neck in 2 (8%) and dome in 1 (4%) patients. Ureteric orifices could not be localized in 8 (32%) patients due to an overlying bladder tumor.
All the patients underwent a Trans urethral resection of bladder tumour prior to radical cystectomy, which besides serving as a method for obtaining tissue biopsy, provided us with an initial idea about the depth of tumour invasion. All the tumors were histologically shown to be TCC, with 12(48%) of grade 2 and 13(52%) of grade 3 variety. All the 25(100%) patients showed evidence of muscle infiltration.
Magnetic Resonance Imaging (MRI)
Assessment of T staging: Of the 25 patients who were evaluated with MRI, 3 (12%) patients showed a bladder tumor with focally disrupted low intensity band of bladder wall (T2a) on T2-weighted image,6 (24%) patients revealed a bladder tumor with thickening of adjacent wall on T1-weighted image and complete disruption of low intensity band of bladder wall on T2- weighted image corresponding to stage T2b. Abnormal intensity in perivesical fat with irregular interface corresponding to stage T3b was found in 13 (52%) patients, while 3 (12%) patient showed evidence suggesting T4a lesion, 2 in seminal vesicles and 1 in cervix.
Assessment of N staging: MRI detected the presence of enlarged, metastatic lymph nodes in 7 (28%) patients out of whom 5 (20%) had single regional enlarged lymph node (N1) and 2 (8%) had multiple regional enlarged lymph nodes (N2).
Operative details
All patients underwent radical cystectomy with bilateral pelvic lymph- adenectomy with construction of an ileal conduit in 15 (60%), Mainz II diversion in 6 (24%) and ileal neobladder in 4(16%) patients. Operative details revealed tumor involving bladder wall (T2b) in 9(36%) patients, tumor involving perivesical fat (T3b) in 14 (56%) patients, and tumor infiltration into the adjacent organs (T4a) in 2 (8%) patients with involvement of seminal vesicles in 1 (4%) patient and cervix in 1 (4%) patient.
Histopathologic details
Histopathological T staging: The resected cystectomy specimens and the pelvic lymph nodes revealed TCC in all patients. The tumor was found invading the superficial muscle (T2a) in 2 (8%) patients and the deep muscle (T2b) in 5(20%) patients. Microscopic invasion of perivesical fat (T3a) was found in 3 (12%) patients while 11 (44%) patients had macroscopic invasion of perivesical fat (T3b). 4 (16%) patients had involvement of contiguous organs (T4a). Infiltration of seminal vesicles was found in 3 (12%) patient. Cervix was infiltrated in 1 (4%) patient.
Histopathological nodal staging: Among 25 patients, lymph node metastases were detected in 7 (28%) patients. Stage N1 was found in 4 (16%) patients while 3 (12%) patients had stage N2 lymph node involvement.
Correlation of tumor staging
Invasion (Stage T2b or above ) or absence of involvement (Stage T2a or below) of deep muscle layer was staged on the basis of MRI appearance with an accuracy of 96% and sensitivity and specificity of 95.7% and 100% respectively [Table 1].
| MRI Diagnosis | Pathologic Diagnosis | Accuracy | Sensitivity | Specificity | P-value | ||
|---|---|---|---|---|---|---|---|
| Positive | Negative | Total | |||||
| Positive | 22 | 0 | 22 | ||||
| Negative | 1 | 2 | 3 | 96% | 95.70% | 100% | 0 |
| Total | 23 | 2 | 25 | ||||
Table 1: Correlation of MRI and pathologic diagnosis of tumor extension into deep muscle layer.
Invasion (Stage T3b or above) or absence of involvement (Stage T2b or below) of perivesical fat was correctly diagnosed with an accuracy of 84% and sensitivity and specificity of 83% and 85.7% respectively [Table 2].
| MRI Diagnosis | Pathologic Diagnosis | Accuracy | Sensitivity | Specificity | P-value | ||
|---|---|---|---|---|---|---|---|
| Positive | Negative | Total | |||||
| Positive | 15 | 1 | 16 | ||||
| Negative | 3 | 6 | 9 | 84% | 83% | 85.7% | 0.001 |
| Total | 18 | 7 | 25 | ||||
Table 2 : Correlation of MRI and pathologic diagnosis of tumor invasion of peri-vesical fat.
Invasion (Stage T4a or above) or absence of involvement (Stage T3b or below) of adjacent organs was correctly diagnosed on the basis of MRI appearance in 2 of 4 cases. The MRI accuracy was 88% with a sensitivity of 50% and specificity of 95.2% [Table 3].
| MRI Diagnosis | Pathologic Diagnosis | Accuracy | Sensitivity | Specificity | P-value | ||
|---|---|---|---|---|---|---|---|
| Positive | Negative | Total | |||||
| Positive | 2 | 1 | 3 | ||||
| Negative | 2 | 20 | 22 | 88% | 50% | 95.2% | 0.011 |
| Total | 4 | 21 | 25 | ||||
Table 3 : Correlation of MR and pathologic diagnosis of tumor extension into adjacent organs.
Pelvic lymphadenopathy was correctly diagnosed by MRI in 5 patients, while as 2 patients, who were shown to have an enlarged lymph node on MRI proved to be non-malignant on histology. In 2 other patients MRI missed metastatic lymph nodes measuring in the range of 0.8 to 1.2 cm, which were shown positive on histology [Table 4]. Pelvic lymphadenopathy was found only in patients with tumor extending through the bladder wall.
| MRI Diagnosis | Pathologic Diagnosis | Accuracy | Sensitivity | Specificity | P-value | ||
|---|---|---|---|---|---|---|---|
| Positive | Negative | Total | |||||
| Positive | 5 | 2 | 7 | ||||
| Negative | 2 | 16 | 18 | 84% | 71.4% | 88.9% | 0.003 |
| Total | 7 | 18 | 25 | ||||
Table 4: Correlation of lymph node metastases at MRI and pathologic examination.
The degree of tumor extension was correctly staged on the basis of the MRI findings in 15 of 25 (60%) patients [Table 5].
| Pathologic diagnosis | MRI diagnosis | |||
|---|---|---|---|---|
| Correct | Overestimated | Underestimated | Total | |
| T0 | - | - | - | - |
| Tis | - | - | - | - |
| T1 | - | - | - | - |
| T2a | 2 | 0 | 0 | 2 |
| T2b | 4 | 1 | 0 | 5 |
| T3a | 0 | 3 | 0 | 3 |
| T3b | 7 | 1 | 3 | 11 |
| T4a | 2 | 0 | 2 | 4 |
| T4b | - | - | - | - |
| Total | 15 | 5 | 5 | 25 |
Table 5: Overall correlation of MRI and pathologic diagnosis.
Statistical analysis
Correlations among variables were assessed using the chisquare test, using SPSS software. There was a highly significant correlation (P< -0.001) between MRI and Pathologic diagnosis of deep muscle and perivesical fat invasion. However, the MRI diagnosis of adjacent organ invasion and lymph node metastases was of relatively lower significance (P< -0.05).
Discussion
Accurate preoperative evaluation of proven bladder carcinoma is important because therapy depends on the clinical stage of the disease. There is a significant error rate (up to 50%) in the clinical staging of primary bladder tumors. [5] Whilst accurate for superficial tumors (T1 and lower), the main error occurs in muscle invasive tumors (T2a and higher) with difficulty in assessing infiltration, lymphadenopathy and distant disease. MRI has been shown to be accurate in staging primary bladder cancer when compared to pathological specimens and this accuracy is not dependant on magnetic field strength. [6,7]
This prospective study was conducted with the aim of determining the accuracy of MRI in the staging of bladder carcinoma by correlating the MR diagnosis with that of the pathologic diagnosis.
The normal bladder wall is depicted as a thin (2 mm thick) linear low-intensity structure that is easily differentiated from urine, which displays higher intensity on T2-weighted images. [8,9]
Contrast-enhanced MR and diffusion weighted MR (DW-MRI) can likely distinguish between non-muscle invasive bladder cancer and muscle invasive cancer with >80% accuracy. [10] Invasion of the deep muscle layer (Stage T2b) was considered present when the low-signal-intensity line was disrupted completely by high signal intensity in the region underlying the tumor in the absence of extension into the perivesical fat. [9,11] Such a finding was found on MR imaging in 7 (28%) of our patients. Deep muscle invasion was correctly assessed in 22 of 23 cases. In one cases, it was underestimated as stage T2a. Underestimation by MRI in this case was a result of interpretational error possibly due to poor image quality. However, misinterpretation may also occur at this point due to a chemical shift artifact that usually occurs at the water- fat interface (between the bladder and perivesical fat) as a result of the difference in resonance frequency between fat and water protons. [12] The chemical shift artifact can be recognized as a dark band along the lateral wall on one side and a bright band along the lateral wall on the opposite side on transverse image. In extreme cases, the chemical shift artifact may lead to apparent thickening of the bladder wall on one side and absence of the bladder wall on the contra lateral side. Knowledge of this artifact coupled with additional imaging along different planes helps avoid misinterpretation of this artifact as deep muscle invasion.
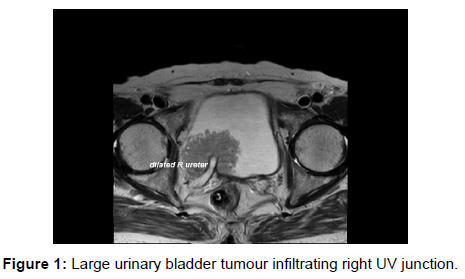
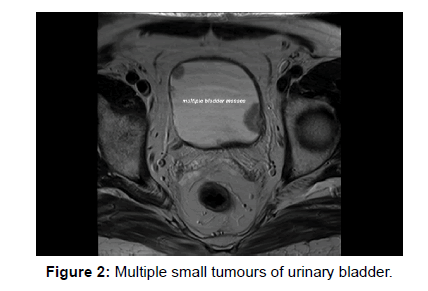
Invasion of perivesical fat by tumor was considered to be present when a soft-tissue mass with signal intensity similar to that of primary tumor on both T1- and T2-weighted images extended into the perivesical fat. Invasion (Stage T3b or above) or absence of involvement (Stage T2b or below) of perivesical fat was correctly diagnosed in 15 of 18 cases. There were, however, 3 false negative cases that had microscopic invasion of perivesical fat which was missed on MR images. [Figures 1 and 2].
Involvement of adjacent organs by the tumor was assessed on both T1- and T2-weighted images. Direct extension of the tumor to an adjacent organ with changes in the normal signal intensity or anatomic configuration of that organ on MR images was considered evidence of involvement of these organs. In 2 of our patients MRI could not interpret the involvement of seminal vesicles, which were later shown to have microscopic infiltration by the tumor on histological examination. There was also 1 false positive case reported by MRI, showing the involvement of seminal vesicle, due to poor quality and motion artifacts (uncooperative patient). One limitation of MR imaging is in the evaluation of tumor extension into the peri urethral glands. Even when the bladder base is well delineated on the saggital image, there is frequently slight indistinctness between the bladder base and the prostatic urethra. [9]
Bilateral pelvic node dissection was performed in all patients, and a thorough examination of the pathologic specimens demonstrated lymph node metastasis in 7 (28%) patients, lymphadenopathy was considered to be present on MRI when the short axis of a node in the transverse plane was 1 cm or more. However, no specific threshold size was defined for the obturator, iliac or lumbar lymph nodes. A larger study is needed to define the normal size of the different types of nodes in the territories of bladder lymphatic drainage. In our limited study, lymph node metastases were confirmed in 7 (28%) patients while it was diagnosed correctly by MR imaging in 5 (20%) patients. In 2 patients, metastatic lymph nodes were missed because of small size. MRI may be superior to CT in the identification of enlarged lymph nodes because of the flow void phenomenon that can be seen in blood vessels, when this occurs, enlarged lymph nodes are seen clearly next to blood vessels and nodal tissue often is clear. Buy et al. reported 97.5% accuracy by MRI in the detection of metastatic lymph nodes with a sensitivity of 83% and a specificity of 100%. [13]
With the use of MR imaging and our staging criteria, we were able to correctly stage the tumor in 60% cases of bladder carcinoma. Overestimation was found in 20% and underestimation of the tumor 20% cases. The largest published series of Buy et al., comparing MRI findings with pathological staging reported that 60% of patients were correctly staged using the TNM system. [13]
Like CT, MRI cannot distinguish between minimal or more extensive superficial muscle invasions. There is debate as to whether distinction between minimal or more extensive muscle involvements can be made. Hayashi et al. evaluated the accuracy of a new staging criterion sub mucosal linear enhancement (SLE) on gadolinium enhanced T1-weighted magnetic resonance imaging using an endorectal surface coil. They noted a markedly enhanced layer within the bladder wall after administering Gd-DTPA. They concluded that if SLE was used as a staging criterion, it was possible to determine whether the tumor was limited to the sub mucosa (T1), or had reached the superficial (T2a) or the deep muscle (T2b). [14]
The use of multi planar reconstruction (three dimensional sequences) have resulted in improved local staging and can be used to select patients for MRI – guided biopsy or those considered for laparoscopic lymph node dissection. [11] Two studies (Barentsz et al. and Jager et al.) have shown that enhanced three dimensional, magnetization prepared – rapid acquisition gradient-echo (MP – RAGE ) images improved the staging accuracy of bladder carcinoma in part because of improved detection of suspicious lymph nodes. [15,16] Newly developed lymphotropic contrast agents like ultra-small super paramagnetic iron oxide (USPIO) particles have been shown to accumulate in benign nodes but not in malignant nodes. [17]
Similarly, there is growing interest in the applications of Diffuse Weighted Imaging (DWI) in oncologic area for last ten years. DWI has important advantages which require no contrast medium and long imaging time. Also it provides qualitative and quantitative information that can be helpful for tumor assessment. Accurate prediction for T staging of urinary bladder carcinoma can be made by means of DWI and Apparent Diffusion Coefficient (ADC) quantification. ADC value is a beneficial method for providing information about grade of bladder carcinomas. [18-21]
MRI parameters like higher MRI T stage, MRI tumor size, tumor extent and hydronephrosis are significantly related to outcome of the disease. [18] In future, the more accurate prognostic assessment of patients afforded by MRI may assist us to assess which patients will undergo cystectomy and which will benefit from radiotherapy alone.
Certain limitations inherent to the present study were small number of patients, failure to delineate the metastatic lymph nodes vividly and a learning curve needs to be broached to eliminate the interpretational errors. [22,23]
Multiparametric magnetic resonance imaging appears more accurate than current methods for local and nodal staging and monitoring tumor response to treatment, but requires further investigation. [19] Use of newer technologies such as contrast enhanced, endorectal MRI with phased array coils and ultrasmall super paramagnetic iron oxide (USPIO) particles hold promise in future for improving the staging accuracy of bladder cancer as also to provide accurate prognostic assessment. However, a larger prospective study using newer MRI technologies is required to determine the exact role of MRI in the staging of bladder cancer.
Conclusion
MR imaging is one of the first modality of choice in imaging of urinary bladder tumours. MR imaging with dynamic gadolinium enhancement readily shows the extent of bladder tumour and the involvement of adjacent organs. Clinical staging, including transurethral resection, can assess involvement of deep muscle, but staging is inaccurate in detecting extravesical disease. Patients with extravesical tumours show significantly higher recurrence rates and lower survival rates compared with those who have organ-confined tumours. MR bladder imaging thus plays a critical role in improving staging accuracy.
MR imaging has many advantages over other modalities for detecting and staging bladder tumours because of its intrinsic high soft tissue contrast, direct multiplanar imaging capabilities, and the availability of a non-nephrotoxic, renally excreted contrast agent. Because of these advantages MR imaging has the potential to become the modality of choice in staging all pelvic malignancies.
However because of the limited resources of the health care system, this technique should be used only to obtain information that directly influences the therapeutic management and outcome. To obtain this goal, knowledge of urologists on MR imaging and knowledge of radiologists on clinical management are needed; therefore, continuous education and communication between these two specialties is a necessity.
A larger prospective study is however required for determining the exact role of MRI in the staging of urinary bladder tumors.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Ploeg M, Aben KK, Klemeney LA. The present and future burden of urinary bladder cancer in the world; J Urol 2009; 27: 289-293.
- Kamarana NM, Karnal MR, Kurkure AP: National cancer registry project 2000; ICMR 2003.
- Pandith AA, Shah ZA, Khan NP, Wani MS, Yousuf A, Rasool R, et al. FGFR3 germ line mutations identified in skeletal dysplasia significantly cause low grade and low stage bladder cancer by somatic mutations. Urotoday Int journal 2010; 3.
- Jenkins JPR: Magnetic resonance imaging of the bladder and prostate. Sutton D (Ed): Textbook of Radiology and Imaging. Vol II. 7th ed. Churchill Livingston, 2003; pp: 1007-1016.
- Pagano F, Bassi P, Gallete TP, Meneghim A, Milani C. Results of contemporary radical cystectomy for invasive bladder cancer with an emphasis on the inadequacy of the tumour, nodes and metastasis classification. J Urol 1991; 145: 45-50.
- Barentsz JO, Ruijs SHJ, Strijk SP. The role of MR imaging in carcinoma of the urinary bladder: AJR 1993; 160: 937-947.
- Barentsz JO, Witjes JA, Ruijs JH. What is new in bladder cancer imaging. Urol Clin North Am.1997; 24: 583-602.
- Fisher MR, Hricak H, Tanagho LA. Urinary bladder MR imaging. Prt II: Neoplasms. Radiology 1985b; 157: 471-477.
- Fisher MR, Hricak H, Crooks LE. Urinary bladder MR Imaging. Part I Normal and benign conditions. Radiology 1985a; 157: 467-470.
- Green DA, Durand M, Gumpeni N. Role of magnetic resonance imaging in bladder cancer: Current status and emerging techniques. BJU International. 2012; 110: 1463-1470.
- Rholl KS, Lee JK, Heiken JP, Ling D, Glazer HS. Primary bladder carcinoma: Evaluation with MR Imaging. Radiology 1987; 163: 117-121.
- Babcock EE, Brateman L, Weinreb JC, Hmer SD, Nunnally RL. Edge artefacts in MR images: chemical shift effect. J Comput Assisr Tomogr 1985; 9: 252-257.
- Buy JN, Moss AA, Guinet C. MR Staging of bladder carcinoma: Correlation with pathologic findings. Radiology 1988; 169: 695-700.
- Hayashi N, Tochigi H, Shiraishi T, Takeda K, Karamura J. A new staging criterion for bladder carcinoma using gadolinium- enhanced magnetic resonance imaging with an endorectal surface coil: A comparison with ultrasonography BJU Int: 2000; 85: 32-36.
- Barentsz JO, Jager G, Mugler JP. Staging urinary bladder cancer: Value of T1-weighted three-dimensional magnetization prepared-rapid gradient-echo and two-dimensional magnetization spin-echo sequences. AJR 1995; 164: 109-115.
- Jager GJ, Barentsz JO, Oosterhof GO, Witjes JA, Ruijs JH. Pelvic adenopathy in prostatic and urinary bladder carcinoma: MR imaging with a three-dimensional T1-weighted magnetization- prepared-rapid gradient-echo sequence. AJR 1996; 167: 1503-1507.
- Weissleder R, Elizondo G, Wittenberg J, Lee AS, Josephson L, Brady TJ. Ultra small super- paramagnetic iron oxide: an intravenous contrast agent for assessing lymph nodes with MR imaging. Radiology, 1990; 175: 494.
- El-Assmy A, Abou-El-Ghar M, Refaie H, El-Diasty T. Diffusion-weighted MR imaging in diagnosis of superficial and invasive urinary bladder carcinoma: A preliminary prospective study. Sci World J 2008; 8: 364-370.
- Zulkif B, Mehmet R, Ahmet KP. The role of diffusion weighted magnetic resonance imaging in oncologic settings. Quant Imaging Med Surg J, 2013.
- Wong JJ, Cheong Y, Woodward PJ, Manning MA. From the archives of the AFIP: Neoplasms of the urinary bladder: Radiologic–pathologic correlation. Radiographics 2006; 26: 553-580.
- Koh DM, Collins DJ. Diffusion-weighted MRI in the body: applications and challenges in oncology. Am J Roentgenol, 2007; 188: 1622-1635
- Robinson P, Collins CD, Ryder WDJ, Carrington BM, Hutchinson CE, Bell D, et al. Relationship of MRI and Clinical Staging to outcome in invasive bladder cancer treated by radiotherapy. Clin Radiology 2000; 55: 301-306.
- Panebianco V, Barchetti F, De Haas RJ, Pearson RA, Kennish SJ, Giannarini G, et al. Improving staging in bladder cancer: The increasing role of multiparametric magnetic resonance imaging. Eur Urol Focus 2016; 2: 113-121.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.