Scalpel Depigmentation and Surgical Crown Lengthening to Improve Anterior Gingival Esthetics
- *Corresponding Author:
- Dr. Pradeep K
Department of Conservative Dentistry and Endodontics, Manipal College of Dental Sciences, Manipal University, Manipal - 576 104, Karnataka, India.
E-mail: drpradeepk@yahoo.co.in
This is an open access article distributed under the terms of the Creative Commons AttributionNon CommercialShare Alike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
A smile is a mesmerizing expression of joy, success, courtesy and reveals self-confidence. The harmony of the smile is determined not only by the shape, position and the color of teeth, but also by the gingival architecture. Gingival tissues form an important part of what we can consider to be a pleasing smile. The elegance of this pleasant smile could be, affected by highly pigmented gingiva. This gingival pigmentation occurs as a result of melanin granules, which are produced by melanoblast. Although melanin pigmentation does not present a medical problem, demand for cosmetic therapy is commonly sort by people with moderately pigmented gingiva. This case report highlights, a case of excessive gingival display and hyperpigmentation treated with anterior crown lengthening and gingival depigmentation using the scalpel technique.
Keywords
Depigmentation, Gingiva, Melanin, Scalpel technique
Introduction
In the present era of dentistry, esthetics holds a significant aspect and clinicians are more concerned about achieving it. An attractive smile and a healthy appearing gingiva are an important factor. Framing the teeth, within the confines of the gingival architecture, has a tremendous impact on the esthetics of the smile. A conservative display of approximately 2-3 mm of the keratinized tissue is considered as part of the ideal esthetic smile. [1,2] Excessive gingival display in contrast can severely compromise the appearance of the individual. Ideally, the inferior border of the upper lip when smiling should rest at the level of the apices of the six maxillary anterior teeth. Maxillary canines and central incisors should have their gingival apices at the same level, whereas the lateral incisors should fall slightly below the imaginary line connecting the apices of the canines and the central incisor. A range of up to 3 mm above the gingival zenith is considered aesthetically pleasing. [3]
The excessive gingival display is commonly associated with vertical maxillary excess, gingival hyperplasia and altered passive eruption. Correction of vertical maxillary excess requires osseous resection surgeries whereas excessive gingival display due to gingival enlargement or altered passive eruption can be effectively corrected by gingivectomy procedures. [4]
Gingival hyper pigmentation is seen in some populations can be attributed to genetic traits. Melanoblasts are non-keratinocytes, which are responsible for gingival pigmentation. [5] This pigmentation may be prevalent across all the races, at any age and is devoid of any gender predilection. [6-8]
The various techniques available to correct excessive gingival display and hyperpigmentation are listed in Table 1. Selection of technique should be based on clinical experience and individual preferences. [9]
Case Report
A 19-year-old healthy female patient was referred from the department of orthodontics for the correction of smile line. Past dental history revealed patient had undergone orthodontic treatment for Angle’s class II division two malocclusion with facially erupted maxillary canine in the first quadrant [Figure 1]. On intra oral examination, patient had a class I smile line in relation to maxillary anterior region. Soft-tissue examination revealed chronic generalized marginal gingivitis. The class I smile line refers to very high smile line i.e., more than 2 mm of marginal gingiva visible or more than 2 mm apical to the cemento enamel junction visible for the reduced, but healthy periodontium. [1] The apico coronal distance of maxillary anteriors was much shorter compared with the anatomic crown. The treatment protocol suggested for this case included complete oral prophylaxis along aesthetic crown lengthening and gingival depigmentation in relation to maxillary the left premolar to the right premolar region.
Procedure
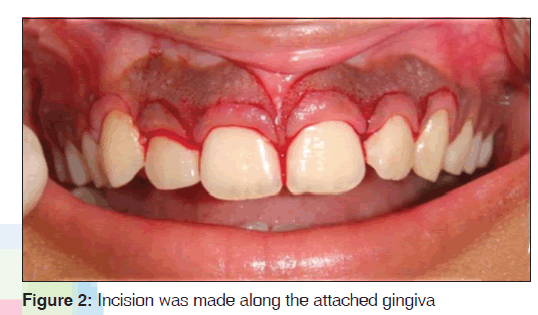
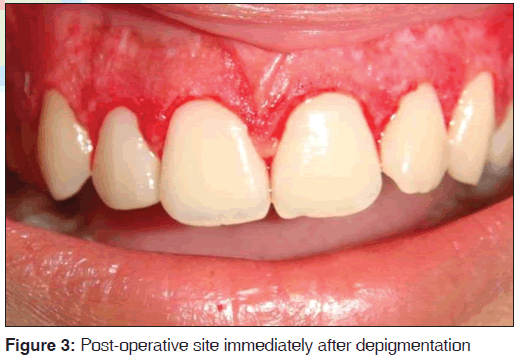
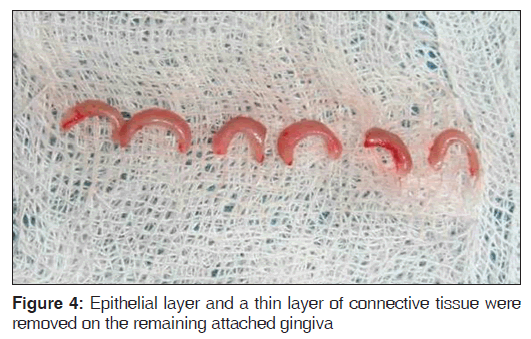
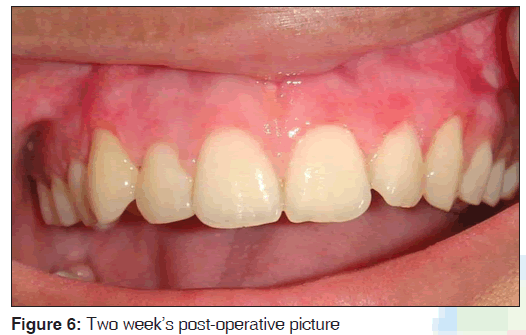
Prior to commencement of the surgical procedure, the patient consent was obtained. The surgical area was anesthetized and a pocket marker was used to mark bleeding points on the maxillary labial surface extending from the left premolar to right premolar region. An external bevel incision at an angle of 45°, using a No. 15 bard parker blade was made along the bleeding points [Figure 2]. Once the gingivectomy procedure was completed to an aesthetically pleasing level, gingival depigmentation procedure was carried out using a No. 11 bard parker blade and a high speed hand piece with a diamond bur [Figure 3]. Local hemostatic agents were used to control hemorrhage during the procedure. The exposed surface was irrigated with saline. The bur was applied over the gingival surface with light feather brushing strokes in a constant motion. Care was taken to see that the epithelial layer along with remnants of the pigment layer was removed [Figure 4]. The surgical wound was protected by a periodontal dressing [Figure 5]. Post-operative instructions were given and the patient was prescribed with antibiotics (amoxicillin 500 mg, thrice daily for 5 days) and analgesics (ibuprofen 400 mg, thrice daily for 3 days). The patient was advised to use chlorhexidine mouth wash (clohex 0.2%; Dr. Reddy’s Lab, Hyderabad, India) for 2 weeks post-operatively to aid in plaque control. Patient was reviewed after 2 weeks, the surgical area revealed satisfactory healing and pigmentation was absent on the newly formed epithelium [Figure 6]. The results were very pleasing and the gingival appearance was satisfactory after 3 months treatment [Figure 7].
Discussion
Pigmented gingival tissue, many at times forces the patients to seek cosmetic treatment. The intensity and distribution of pigmentation of the oral mucosa is variable, not only between races, but also between different individuals of the same race and within different areas of the same mouth. [11] Physiologic pigmentation is probably genetically determined, but the degree of pigmentation is partially related to mechanical, chemical and physical stimulation. [5,12] The normal color of gingiva is determined by the degree of vascularization, the thickness of the keratinized layer and the amount of the pigment containing cells. Melanin pigmentation is mainly caused by melanin deposition by active melanocytes located mainly in the basal layer of the oral epithelium. Pigmentations can be removed for esthetic reasons. Several treatment modalities have been used for this aim. The choice of technique for depigmentation of the gingiva should be based on operator experience, patient’s economic conditions and individual preferences.
Cryosurgery produces considerable swelling and it is also accompanied by increased soft-tissue damage. Since it does not have a tactile effect, depth control is difficult and optimal duration of freezing is not known, but prolonged freezing increases tissue destruction. [13] Lasers is also another option, but they require sophisticated equipment, occupies large space and is expensive. A free gingival graft can also be used to eliminate the pigmented areas. However, it requires an additional surgical site (donor site) and color matching. These treatment modalities, however, are not widely accepted or popularly used. Electrosurgery requires more expertise than scalpel surgery. Prolonged or repeated application of current to tissue induces heat accumulation and unwanted tissue destruction.
Scalpel surgical technique is highly recommended in consideration of the equipment constraints that may not be frequently available in clinics. [11] It is known that the healing period for scalpel wounds is faster than other techniques. However, scalpel surgery may cause unpleasant bleeding during and after the procedure and it is necessary to cover the exposed gingival tissue with periodontal dressing for 7-10 days. [11] Post-surgical repigmentation of gingiva has been previously reported. Repigmentation is described as spontaneous and has been attributed to the activity and migration of melanocytic cells from surrounding areas.
In this present case, it was observed that there was no relapse of the pigmentated areas on the gingival surface on the maxillary anterior region until up to 2 months.
Conclusion
Excessive gingival display and gingival hyper pigmentation are major concerns for large number of patients. Although several techniques are currently in use, the scalpel technique is still the most widely employed. Lasers and cryosurgery may offer less post-operative pain. However, the choice of the technique should be dependent on clinical expertise and patient affordability. Thus, we conclude that depigmentation of hyperpigmented gingiva by scalpel surgery is simple, easy to perform, cost-effective and above all it causes less discomfort and is aesthetically acceptable to the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Liebart MF, Fouque-Deruelle C, Santini A, Dillier FL, Monnet-Corti V, Glise JM, et al. Smile line and periodontium visibility. Periodontol 2000;1:17-25.
- Granstein RD, Sober AJ. Drug- and heavy metal – Induced hyperpigmentation. J Am Acad Dermatol 1981;5:1-18.
- Coslet JG, Vanarsdall R, Weisgold A. Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult. Alpha Omegan 1977;70:24-8.
- Hürzeler MB, Weng D. Functional and esthetic outcome enhancement of periodontal surgery by application of plastic surgery principles. Int J Periodontics Restorative Dent 1999; 19:36-43.
- Dummett CO. Oral pigmentation. First symposium of oral pigmentation. J Periodontol. 1960; 31:356–60.
- Page LR, Corio RL, Crawford BE, Giansanti JS, Weathers DR. The oral melanotic macule. Oral Surg Oral Med Oral Pathol 1977; 44:219-26.
- Trelles MA, Verkruysse W, Seguí JM, Udaeta A. Treatment of melanotic spots in the gingiva by argon laser. J Oral Maxillofac Surg 1993;51:759-61.
- Prinz H. Pigmentation of the oral mucous membrane. Dent Cosm 1932;72:554-61.
- Ishikawa I, Aoki A, Takasaki AA. Potential applications of Erbium:YAG laser in periodontics. J Periodontal Res 2004;39:275-85.
- Kasagani SK, Nutalapati R, Mutthineni RB. Esthetic depigmentation of anterior gingiva. A case series. N Y State Dent J 2012;78:26-31.
- Prasad SS, Agarwal N, Reddy NR. Gingival depigmentation: A case report. People J Sci Res 2010;3:27-9.
- Ciçek Y, Ertaş U. The normal and pathological pigmentation of oral mucous membrane: A review. J Contemp Dent Pract 2003;4:76-86.
- Almas K, Sadig W. Surgical treatment of melanin-pigmented gingiva: An esthetic approach. Indian J Dent Res 2002;13:70-3.







 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.