Screening for Cervical Cancer: A Review of Outcome among Infertile Women in a Tertiary Hospital in North-West Nigeria
- *Corresponding Author:
- Dr. Daniel C Nnadi
Department of Obstetrics and Gynecology, Usmanu Dan-Fodio University Teaching Hospital, Sokoto,Nigeria.
E-mail:dc_nnadi@yahoo.com
Abstract
Background: Cervical cancer is the most common genital tract malignancy in the developing countries of the world. Interestingly, it has a pre-invasive stage, which can be detected through screening. The etiological organism of the disease is the human papilloma virus (HPV) that is sexually transmitted and sexually transmitted infections play a major role in the causation of infertility in developing countries. Aim: The aim of this study is to determine the prevalence of abnormal cervical smear among infertile women at Usmanu Dan-Fodiyo University Teaching Hospital (UDUTH) Sokoto, Nigeria. Materials and Methods: This is a cross-sectional study involving the assessment of cervical smears taken from infertile women attending the gynecological out‑patient clinic of UDUTH sokoto over a 12‑month period. cross‑sectional study involving the assessment of the cervical smears taken from infertile women attending the gynecological out‑patient clinic of UDUTH Sokoto over a 12‑month period. Statistical analysis of the results was carried out using the EPI-INFO 3.5.1 (CDC, Atlanta Georgia, USA). Chi square test was used for association at p‑value< 0.05 at 95 % confidence interval Results: A total of 162 patients were screened during the study period. Their ages ranged from 15 to 46 years with a mean of 27.9 (6.2) years and modal age of 25‑34 years. Majority of the subjects 88/159 (55.4%) were in the lower socio‑economic class and 75/159 (47.2%) of the women were nullipara. Out of the 159 subjects with adequate smears, 58/159 (36.8%) were normal while 44/159 (27.8%) had inflammatory lesions. Cervical intraepithelial lesions were observed in 18/159 (11.3%) of the smears while 25 (15.7%) had evidence of HPV infection. Conclusions: Considering the relatively high incidence 18/159 (11.3%) of cervical intraepithelial lesions seen among the subjects, there is the need to integrate cervical smear in the general infertility work-up.
Keywords
Cervical cytology, Infertility, Nigeria
Introduction
Cervical cancer is one of the common gynecological cancers world-wide, especially in the developing countries such as Nigeria, where not only do the pre-disposing factors abound, but there is hardly any organized screening program.[1-3] It is the second leading female cancer world-wide and the most common female malignancy in the developing countries.[2,4] Cervical cancer is a leading cause of cancer related death in women in most developing countries of the world and has over 500,000 new cases and more than 300,000 deaths globally each year.[5] Many of those who die are young mothers. The age standardized incidence rate in developing countries range between 25 and 43 cases/100,000 women in contrast to North America where it is 7.7/cases/100,000 women.[2,5]
In the low-resource countries, majority of the patients present with advanced disease at relatively young ages.[3,4] In Zaria Nigeria, cervical cancer accounted for 77% of gynecological malignancies with over 88% of cases presenting above stage 11a of the disease,[6,7] while in Kano, cervical cancer has overtaken breast cancer as the most common cancer in women.[8] Adewole in Ibadan reported that cervical cancer is the most common malignant tumor seen in women with a relative ratio frequency of 19.9%.[9]
In the developed countries, the incidence of cervical cancer and associated morbidity and mortality has each decreased over the years since 1973.[10] The decrease is largely due to the success of mass screening programs using the conventional Papanicolaou (Pap) test to detect pre-invasive or early stage of the disease.[11] Cervical cancer is a preventable disease, because a detectable and treatable pre-invasive disease stage of about a period 10-15 years precedes the invasive form.[12] During this period, there may be shedding of cells from the cervix. Such cells form the basis for the Pap smear. It is now widely accepted that cytological methods of screening for cervical cancer and its precursors have become the mainstay of population-based prevention programs.[12]
Sexual transmitted infections play an important role in the etiology of cervical intra-epithelial lesions and hence cervical cancer. Many epidemiological studies indicate the involvement of the human papilloma virus (HPV).[11,12]
Infection by oncogenic strains of HPV (especially types 18 and 16), which generally occurs in teenage or early twenties and thirties, causes cellular changes that may lead to cervical cancer after 20 or more years.[12] Several risk factors associated with cervical cancer have also been studied extensively. Many are now thought to be mere proxies of the HPV infection apart from age, smoking, parity and nutritional status, which may be independent co-factors in the progression of HPV infection.[12,13]
Lack of funds, manpower and poor health-care policies have impeded the implementation of cervical cancer screening programs in many developing countries especially those in sub-Saharan Africa.[14]
In Nigeria, there is no public health programs organized primarily to screen for cervical cancer and where they exist, the acceptance and utilization by the target population is limited by a number of factors. These include lack of awareness, cost of accessing the service and fear of the result.[13]
The World Health Organization (WHO) stated that most cases of female infertility in developing countries are due to pelvic inflammatory disease (PID).[15] Most cases of PID result from sexually transmitted infections, unsafe abortions and puerperal sepsis. It has been reported that endocervical gonorrhea was detected in 20% of infertile women in a Nigerian hospital.[16]
Since the causative agent of the cervical cancer is HPV (a sexually transmitted organism), infertile women could constitute a high risk group for the development of cervical cancer and thus should benefit from regular cervical cytology.
The aim of this study is to determine the prevalence of abnormal cervical smears among infertile women at Usmanu Dan-fodiyo University Teaching Hospital (UDUTH) Sokoto.
Materials and Methods
Setting
The UDUTH is tertiary health institution situated in the North-Western region of Nigeria. It provides tertiary healthcare services to Sokoto, Kebbi, Zamfara and Niger states. It also receives referrals from the Niger republic, a neighboring country. The institution is accredited for both the undergraduate and postgraduate medical training. It runs a residency training program in the various specialties including histopathology.
Screening for cervical cancer by cytological evaluation was introduced into the hospital in December 2004. The screening program is basically opportunistic and thus the uptake was low.
Study design
It was a cross-sectional study spanning over 12 months (January 2010 to December 2010). All the infertile patients who were attending the gynecological outpatient clinic during the study period were identified and counseled about the study. Patients were selected by simple random technique. The sample size was determined by the formula N = Z2pq/d2, where “p” was the prevalence of abnormal cervical lesions as determined by earlier studies and was equaled to 12%. This generated the sample size. A total of 162 women met the set criteria (which included written consent and absence of vaginitis, abnormal uterine bleeding and diagnosed cancer of the genital tract) and were recruited into the study.
Patients were entered into the study proforma. The proforma included the subject’s hospital number, age, marital status, level of education, occupation of both patient and spouse, parity, address of residence and tribe. Other relevant information included the gynecological history, nature and duration of infertility.
Patients were asked to come for the test 5 days after the cessation of their last menses and to abstain from coitus 24 h before the test. The smears were taken on each clinic day by a resident doctor who had undergone training on cervical smear procedure. On presentation, patient was asked to empty her bladder and was placed in the dorsal position. A gentle pelvic examination was performed and the cervix exposed with a Cusco’s vaginal speculum. A scrape smear was taken with the help of a wooden spatula inserted at the external cervical os and gently rotated over the surface of the cervix making sure that the squamocolumnar junction was well-scrapped. The smear was then thinly and uniformly spread over the middle of two pre-labeled glass slides and immediately immersed in 95% ethyl alcohol for fixation and sent to the histopathology department for cytology. The smears were stained using the Pap method.
The modified Bethesda system, which utilizes the terminology, squamous intraepithelial lesions (SIL) was utilized for uniformity.
The proforma was filled and the patient was given a follow-up appointment to the gynecological clinic for the result of the test. A single histopathologist read the slides. The results were made available to the patients after 2 weeks. The hospital’s committee on ethics approved of the study.
Statistical analysis of the results was carried out using the EPI-INFO 3.5.1 (CDC, Atlanta Georgia, USA). Chi square test was used for association at p-value< 0.05 at 95 % confidence interval.
Results
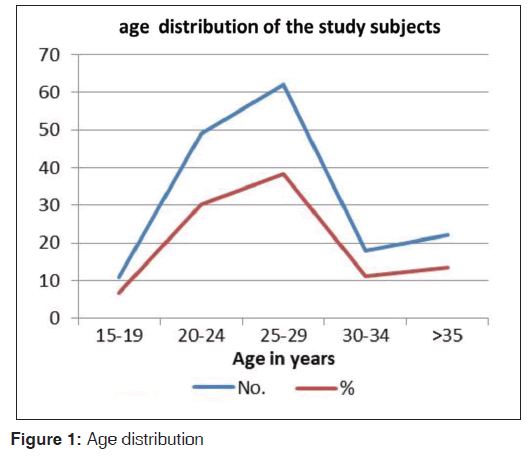
A total of 162 patients were screened during the study period and 159 had adequate smears thus constituting the subjects of the study. Their ages ranged from 15 to 46 years with a mean of 27.9 (6.2) years and modal age of 25-34 years [Figure 1].
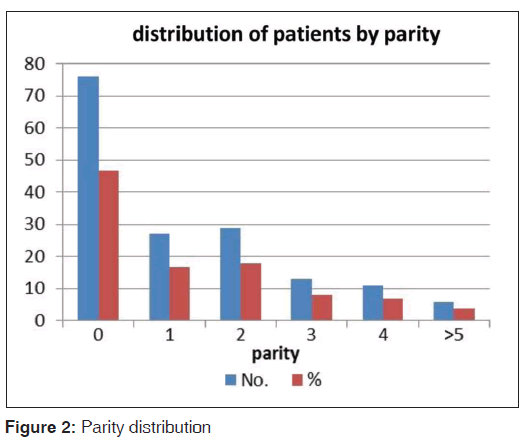
The distribution of patients by parity is shown in Figure 2. Majority of the subjects 75/159(447.2%) were nullipara.
Most of the patients screened (88/159 (55.4 %) belonged to the low socio-economic class.
Most of the subjects, 94/159 ( (59.1%), had secondary infertility while the rest had primary infertility.
Cytological reports of the cervical smears as depicted in Table 1 showed that 58/159 (36.4%) were normal, 25/159 (15.7%) had evidence of infection by HPV and 18/159 (11.3%) had features of SIL. Out of the 18 cases of SIL, 11 were low grade SIL, while 4 were high grade SIL as shown in Table 2.
| Cytology | Number | Percentage |
|---|---|---|
| Normal | 58 | 36.5 |
| Inflammatory | 44 | 27.8 |
| Metaplasia | 14 | 8.8 |
| HPV | 25 | 15.7 |
| SIL | 18 | 11.3 |
| Total | 159 | 100 |
HPV: Human papilloma virus, SIL: Squamous intraepithelial lesions
Table 1: Cytological reports
| SIL | Number | Percentage |
|---|---|---|
| LGSIL | 36 | 83.7 |
| HGSIL | 7 | 16.3 |
| HGSIL | 43 | 100 |
| Total | 43 | 100 |
Majority of the abnormal cervical smear (83.7%) were SIL: Squamous intraepithelial lesion, LGSIL: Low grade squamous intraepithelial lesion. HGSIL: high grade squamous intraepithelial lesion
Table 2: Classification of the abnormal cervical smear according to the Bethesda system
Table 3 shows the relationship between the age and parity of the patients and abnormal cervical cytology.
| Age (years) | Number | SIL | Percentage |
|---|---|---|---|
| 15-19 | 11 | 2 | 1.3 |
| 20-24 | 47 | 3 | 1.9 |
| 25-29 | 62 | 7 | 4.4 |
| 30-34 | 18 | 13 | 8.2 |
| ≥35 | 21 | 18 | 11.3 |
| Total | 159 | 43 | 27.0 (χ2 34.6, |
| P<0.001 | |||
| Parity | |||
| 0 | 58 | 2 | 1.3 |
| 1 | 32 | 5 | 3.1 |
| 2 | 28 | 7 | 4.4 |
| 3 | 20 | 10 | 6.3 |
| 4 | 16 | 14 | 8.8 |
| ≥5 | 5 | 5 | 3.1 |
| Total | 159 | 43 | 27.0 (χ2 54.5, |
| P<0.001 |
SIL: Squamous intraepithelial lesions
Table 3: The relationship between age/parity and abnormal cervical smear
There was a progressive rise in the frequency of SIL with increasing age with a peak in patients above 35 years. This was found to be statistically significant (χ2 34.6, P < 0.001). The frequency of SIL also showed a rising trend with increasing parity. This relationship was significant statistically at χ2 54.5, P < 0.001. Abnormal cervical smear was significantly more common in subjects with secondary infertility, 41/94 (0.44%) compared with those with primary infertility, 0.03% (2/65); P < 0.001.
Discussion
Age is one of the most important risk factor to be considered when formulating a cervical cancer screening policy.[17] The WHO states that where resources are limited, cervical cancer prevention programs should focus on (1) screening women between the ages of 30 and 49 years at least once in their lifetime, gradually expanding the program to other age groups and then to more frequent screening,[18] and (2) ensuring that women with positive results of testing for pre-cancer are successfully treated. A collaborative study of screening programs in eight developed countries concluded that such programs should be aimed at women aged at least 35 years, but should start some years before this age of 35 years.[19] Among the women screened in this study, this group (35 years and above) accounted for 14% while those aged 34 years and below constituted 86%, but SIL were more prevalent (11.3%) in the latter age group. Studies have shown that the age specific incidence of SIL showed a high incidence in the lower age groups, which justifies the case to routinely screen women attending the infertility clinic.[19]
A total of 75 patients (47.2%) were nulliparous, while 6 (3.8%) were grand multipara. This is a reflection of the criterion (infertility) used in the selectio n of the study subjects. The incidence of SIL in this study was 11.3%. In a high-risk group screened for SIL in UCH, Ibadan, Omigbodun reported incidence of 9.3%.[20] Incidence of 2.6% has been reported among pregnant women attending antenatal care at Ile-Ife.[21] Although no previous studies have been documented on the prevalence of SIL among infertile women in Nigeria, the relatively high incidence of 11.3% found in this study underscores the need for similar studies in different centers. There was also a relationship between the type of infertility and abnormal cervical cytology. Abnormal cervical smear was significantly more common in subjects with secondary infertility, 41/94(43.6%) compared with those with primary infertility, 2/65 (0.03%), P < 0.01. There is a high incidence of secondary infertility in Sokoto, which may be related to the increased rate of puerperal sepsis as a result of home delivery, which is prevalent here.[22]
HPV infection was found in 15.7% the subjects in this study. Saito et al.[11] reported an incidence of 6.6% in Japanese women. The advent of methods of HPV-deoxyribonucleic acid (DNA) detection by polymerase chain reaction has led to increasing interest in the role of testing for this virus in screening. One of the most promising uses of HPV DNA testing is to determine which women with low-grade cytological abnormalities require colposcopic evaluation. Inflammatory cells were present in 27.8% of the smears suggesting chronic cervicitis, which the study subjects were prone to. A relatively high incidence of inflammatory cells (62.6%) found in the Enugu study may be due to the high incidence of genital infection in the zone.[19]
In conclusion, the relatively high incidence of squamous intraepithelial lesions found in this study emphasizes the need to include cervical cancer screening services during infertility work-up. It is high time a national screening policy be formulated and implemented since cervical cancer is the most common gynecological cancer in the country.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Edozien LC, Adewole IF. Cervical carcinoma in Nigeria – A need for early detection. Afr J Med Med Sci 1993;22:87-92.
- World Health Organization. Cervical Cancer Screening in Developing Countries. Report of a WHO Consultation. Geneva: WHO; 2002.
- Ezem BU. Awareness and uptake of cervical cancer screening in Owerri, South-Eastern Nigeria. Ann Afr Med 2007;6:94-8.
- Adefuye PO. Knowledge and practice of cervical cancer screening among professional health workers in a suburban district in Nigeria. Niger Med Pract 2006;50:19-26.
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893-917.
- Mohammed A, Ahmed SA, Oluwole OP, Avidime S. Malignant tumours of the female genital tract in Zaria, Nigeria: Analysis of 513 cases. Ann Afr Med 2006;5:93-6.
- Ifenne DI, Shittu SO, Ekwenpu CC. Cervical smear in pregnancy: The Zaria experience. Niger J Surg Res 2001;3:81-3.
- Mohammed AZ, Edino ST, Ochicha O, Gwarzo AK, Samaila AA. Cancer in Nigeria: A 10-year analysis of the Kano cancer registry. Niger J Med 2008;17:280-4.
- Ajayi IO, Adewole IF. Breast and cervical cancer screening activities among family physicians in Nigeria. Afr J Med Med Sci 2002;31:305-9.
- McCrory DC, Matchar DB, Bastian L, Datta S, Hasselblad V, Hickey J, et al: Evaluation of Cervical Cytology. Summary, Evidence Report\Technology Assessment: No. 5, January 1999. AHCPR Publication Rockville, Maryland USA: (No. 99-E009).
- Saito J, Sumiyoshi M, Nakatani H, Ikeda M, Hoshiai H, Noda K. Dysplasia and HPV infection initially detected by DNA analysis in cytomorphologically normal cervical smears. Int J Gynaecol Obstet 1995;51:43-8.
- An HJ, Kim KR, Kim IS, Kim DW, Park MH, Park IA, et al. Prevalence of human papillomavirus DNA in various histological subtypes of cervical adenocarcinoma: A population-based study. Mod Pathol 2005;18:528-34.
- Misra JS, Srivastava S, Singh U, Srivastava AN. Risk-factors and strategies for control of carcinoma cervix in India: Hospital based cytological screening experience of 35 years. Indian J Cancer 2009;46:155-9.
- Akinola SE, Awotunde OT, Attansey AC, Adeyemi AS, Atanda OO. Gynaecological consultations at the Bowens University Teaching Hospital Ogbomoso, Nigeria. Savan J Med Res Pract 2012;1:32-6.
- Aboulghar MA, Mansour RT, Serour GI, Al-Inany HG. Diagnosis and management of unexplained infertility: An update. Arch Gynecol Obstet 2003;267:177-88.
- Akande EO. Women’s health in Nigeria: Past, present and prospects for the next millennium. The ninth Paul Hendrickse memorial lecture. Afr J Med Med Sci 2000;29:75-82.
- Bradley J, Barone M, Mahé C, Lewis R, Luciani S. Delivering cervical cancer prevention services in low-resource settings. Int J Gynaecol Obstet 2005;89 Suppl 2:S21-9.
- Miller AB. Cervical Cancer Screening Programs: Managerial Guidelines. Geneva: World Health Organization; 1992.
- Akpala CO, Okeke TA, Okafor U. Epidemiological studies of cervical cancer screening program population. Sahel Med J 1999;2:30-3.
- Omigbodun AO, Ogunniyi JO, Adelusi B. Cervical intraepithelial neoplasia in a sexually transmitted disease clinic population in Nigeria. J Obstet Gynaecol East Cent Afr 1988;7:74-6.
- Olatunbosun OA, Ayangade SO, Okwerekwu GA. Cytologic screening for cervical neoplasia in pregnancy. Trop J Obstet Gynaecol 1985;5:63-6.
- Ekele BA, Tunau KA. Place of delivery among women who had antenatal care in a teaching hospital. Acta Obstet Gynecol Scand 2007;86:627-30.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.