Single Versus Multi‑visit Endodontic Treatment of Teeth with Apical Periodontitis: An In vivo Study with 1‑year Evaluation
- *Corresponding Author:
- Dr. Gurdeep SG
Department of Conservative Dentistry and Endodontics, JCD Dental College, JCD Vidyapeeth, Sirsa, Haryana, India.
E-mail: gsg1985@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Citation Gill GS, Bhuyan AC, Kalita C, Das L, Kataki R, Bhuyan D. Single versus multi-visit endodontic treatment of teeth with apical periodontitis: An in vivo study with 1-year evaluation. Ann Med Health Sci Res 2016;6:19-26.
Abstract
Background: Apical periodontitis (AP) is one of the most prevalent diseases of the teeth. Treatment of AP is based on the removal of the cause, i.e., bacteria from the root canals. Achievement of adequate bacterial eradication in one appointment treatment remains a controversy.
Aim: This prospective study was conducted with the objective to compare the periapical healing of teeth with AP treated in (a) single visit versus (b) two visits, either with or without Vitapex as an intracanal medicament.
Subjects and Methods: Patients were selected randomly from the Department of Conservative Dentistry and Endodontics. Forty‑three patients (81 teeth) met the inclusion criteria, i.e., AP (both symptomatic and asymptomatic) visible radiographically size ≥2 mm × 2 mm, not suffering from any immune‑compromising disease, age between 16 and 65 years and tooth not accessed previously. Patients were randomly divided into three groups, i.e., single‑visit group (Group 1), multi‑visit group without any intracanal medicament (Group 2), and multi‑visit group with Vitapex as interim intracanal medicament (Group 3). Comparison was done radiographically using periapical index (PAI). The primary outcome measure was the change in periapical radiolucency after 1 year assessed by PAI scores. The Mann–Whitney U‑test was used to evaluate differences between groups at baseline (immediate postoperative) and at the 12‑month follow‑up evaluation. Change in PAI score for each group from baseline to 12‑month follow‑up evaluation was tested with the Wilcoxon signed rank test. The secondary outcome measures, proportion of teeth in each group that could be considered improved (decreased PAI score) or healed (PAI <2), were assessed with the Chi‑square test.
Results: No statistically significant difference in periapical healing was found between three groups.
Conclusion: After 1‑year evaluation, no difference in periapical healing was found between single‑visit treatment and multi‑visit treatment groups with the given sample size.
Keywords
1-year evaluation, Apical periodontitis, Multi-visit treatment, Single visit, Vitapex
Introduction
Apical periodontitis (AP) is one of the most prevalent diseases of the teeth with prevalence as high as one radiolucency per patient noted in a recent study.[1] It is the main prognostic factor in initial endodontic treatment, healed rate in teeth with preoperative radiolucency is significantly lower than teeth without AP.[2] Ørstavik and Pitt Ford have stated that the “ultimate biological aim of root canal treatment as either to prevent or cure AP (in cases where disease is already present).”[3] Treatment of AP aims at the removal of cause, i.e., bacteria present in the canal.Role of bacteria in the causation and the persistence of AP are well-established.[4,5] Mechanical debridement combined with antibacterial irrigation (0.5–6% sodium hypochlorite) can render 40–60% of the treated teeth bacteria-negative.[6,7] In addition to mechanical debridement and antibacterial irrigation, use of calcium hydroxide as intracanal medicament between canals has been shown to reduce the bacterial count further by 80–100%.[8,9] This has been the basis of the multi-visit treatment of AP. However, many studies have questioned the effectiveness of the calcium hydroxide in the healing of AP.[6,10-12] Moreover, the tooth may also be susceptible to reinfection through the temporary filling and dressing during the interim period in case of multiple visits.
Single-visit root canal treatment of the AP relies on mechanical debridement, disinfection with antimicrobial irrigating solution, and the antimicrobial activity of the sealer or the zinc (Zn+2) ions of Gutta-percha for eradication of bacteria.[12-14] Remaining bacteria may be deprived of nutrition and space to multiply.[15] It has become common practice and offers several advantages such as high patient acceptance[16] and reduced flare-up rate.[17,18]
Achievement of adequate bacterial eradication in one appointment treatment is the main controversial question. Although there might be a reasonable biologic argument to prefer multiple appointment root canal therapy for infected teeth with AP, clinical research has been equivocal.[19-21] The direct evidence comparing the healing rates following single- and multiple-visit root canal treatment should provide insight as to which regimen is more effective for the treatment of such a prevalent problem.
The main objective of the present study was to compare the periapical healing of teeth with AP treated in (a) single visit and in (b) multiple visits with and without intracanal medicament (Vitapex, J. Morita Co., Tokyo, Japan) using periapical index (PAI).
Subjects and Methods
Patient selection
After informed consent, study subjects were selected randomly from among the patients referred to the Department of Conservative Dentistry and Endodontics for initial nonsurgical endodontic treatment. The study was conducted between 2010 and 2013 in Conservative Dentistry and Endodontics Department. Ethical clearance for the study was obtained from the Institutional Review Board.
The primary criterion for inclusion of subjects in the study was the presence of radiographically demonstrable AP (minimum size - 2.0 mm × 2.0 mm) in maxillary anterior or mandibular anterior tooth/teeth. Both symptomatic and asymptomatic patients were included in the study. Patients were excluded from the study if (a) they had a diagnosis of diabetes, (b) they had a diagnosis of immune-compromising disease, (c) they were <16 or >65-year-old, or (d) the tooth had been previously accessed or treated. Once the eligibility was confirmed, the study was explained to the patient, and the patient was invited to participate. After written and verbal informed consent was obtained, the patients were randomly assigned to the treatment groups by throwing of a dice viz., Group 1 (single-visit treatment group), Group 2 (multi-visit treatment group without any intracanal medicament), and Group 3 (multi-visit treatment group with Vitapex as an intracanal medicament).
Clinical procedure
All patients were treated by one investigator (gsg) according to a standard regimen including elements of access, rubber dam, and establishment of asepsis. Local anesthesia (2% lidocaine with 1:100,000 epinephrine) was administered to the patient. Initial caries excavation was performed, rubber dam isolation was obtained, and a standard access cavity was prepared. Initial canal working length was established by using the Root ZX electronic apex locator (J. Morita Co., Tokyo, Japan) and a #15 stainless steel K-file. Working length was confirmed and adjusted as needed by using radiographs. Canals were instrumented using stainless steel K-files and H-files using step-back technique. Canals were irrigated with 5.0 mL 2.5% sodium hypochlorite after each instrumentation cycle, and canal patency was maintained by passing a #10 stainless steel file up to working length. After the completion of canal instrumentation, all canals were irrigated with 5.0 mL, 17% ethylenediaminetetraacetic acid (EDTA) (Glyde, Dentsply Maillefer, Ballaigues, Switzerland) for 1 min followed by a final irrigation with 5.0 mL 2.5% sodium hypochlorite. Canals were then dried with sterile paper points. Obturation was done with Gutta-percha and zinc oxide eugenol sealer using lateral condensation technique.
Teeth in Group 1 were obturated at the same appointment by using the lateral condensation technique using Gutta-percha and access cavities were restored using anterior composite restorations.
In Group 2, instrumentation was completed at the first appointment. The canal was left empty, and access cavity was closed using Cavit-G (3M ESPE) for at least 1 week before the second appointment. On the second appointment, the obturation was completed using lateral condensation technique and tooth/teeth restored with composite restoration.
In Group 3, instrumentation was completed at the first appointment. Vitapex was placed in the canal to remain for at least 1 week before second appointment. At the second appointment, the Vitapex paste was removed by using circumferential filing with Hedstrom-files and copious irrigation with 2.5% sodium hypochlorite followed by 5.0 mL 17% EDTA and a final rinse of 5.0 mL 2.5% sodium hypochlorite. Complete removal of the Vitapex paste was confirmed radiographically. The canals were dried with sterile paper points, and obturation was performed with the same technique described for Group 1. After completion of treatment, the teeth were restored with a composite restoration.
Radiographic technique
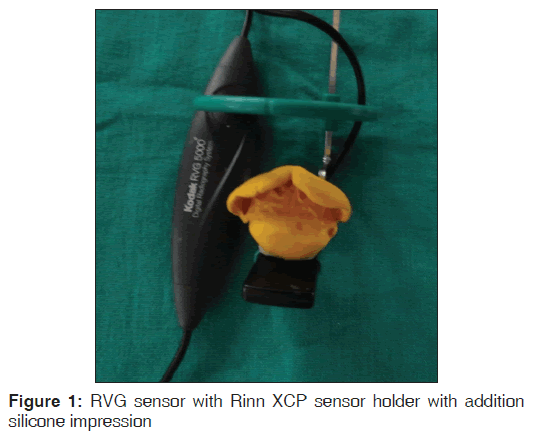
All radiographs were done using Kodak RVG5000 size#2 sensor and Gnatus X-ray machine operating at (70 KVp-7 mA-0.08-1540VA) with exposure settings kept constant at 0.32 s. Immediately after obturation, digital radiographs were taken using Rinn XCP sensor holder (Rinn Corp., Elgin, IL, USA) stabilized with polyvinyl siloxane impression material (AFFINIS-Coltene Whaledent) to standardize image geometry. Impression of each patient was preserved for follow-up radiograph in a polythene packet. Follow-up radiographs after 1 year recall were done with the individual custom index and recorded exposure settings [Figure 1].
Outcome measures and data analysis
The primary outcome measure for this study was change in apical bone density (radiographically) at 12 months. Secondary outcome measures were the presence of clinical symptoms or abnormal findings at 12 months (spontaneous pain, presence of sinus tract, swelling, mobility, or sensitivity to percussion or palpation).
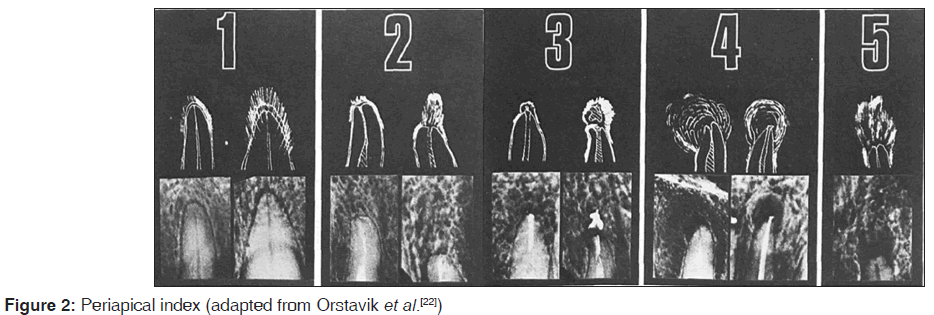
Radiographic evaluation [Figure 2] was done using the PAI scoring system.[22,23] This is a 5-point scale radiographic interpretation designed to determine the absence, presence, or transformation of a disease state. Radiographs to be assessed were compared with a set of five radiographic images with corresponding line drawings and their associated score on a photographic print (derived from Brynolf’s histologic-radiographic co-relation study).[24]
Radiographic images were evaluated blindly and independently by 4 experienced endodontists by assigning a score according to which of the reference images it appears to match. Before evaluation of the study images, each examiner graded a series of twenty radiographic images not associated with the study sample and representing a wide range of periapical bone densities. Instructions for grading images with the PAI scoring system were adapted from Orstavik et al.[22] and are presented in Figure 2. The following specific written instructions were given to the examiners:
• Find the reference radiograph where the periapical area most closely resembles the periapical area you are studying. Assign the corresponding score to the observed root
• When in doubt, assign a higher score
• All teeth must be given a score.
Approximately, 1 week after the calibration session, each examiner independently scored the randomly assembled study images. All study images were coded by the investigator and evaluated randomly and individually on a 15.6” LCD monitor by the four experienced endodontists. The examiners then met as a group and reviewed all scores to enhance calibration and inter-rater agreement. Consensus was reached on images that were not initially scored the same by all examiners.
To assess intrarater agreement, 4 weeks after the first session the examiners again scored all study images. This method generated a total of 6 PAI scores for each image, 2 from each of the three examiners. Agreement between and within examiners was determined by using the intraclass correlation coefficient (ICC). Intrarater reliability was measured with the single measure ICC (SPSS 13 for Windows, SPSS Inc., Chicago, IL, USA), and inter-rater agreement was measured with the average measure ICC (also known as the inter-rater reliability coefficient).
After the second independent scoring session, the examiners met as a group to reach consensus on cases that did not receive unanimous agreement on the PAI score. Consensus was reached on all images. The consensus score for each image was considered the true score and was used for statistical analysis. The identifying code for each image was not broken until after the consensus score was determined. Computations of necessary sample sizes for comparisons among treatments indicate that sample sizes of 55 per group would be sufficient to detect differences in rates of 5% or more, with a power of P = 0.20.[25]
The Mann–Whitney U-test was used to evaluate differences between groups at baseline (immediate postoperative) and at the 12-month follow-up evaluation. Change in PAI score for each group from baseline to 12-month follow-up evaluation was tested with the Wilcoxon signed rank test. The secondary outcome measures, proportion of teeth in each group that could be considered improved (decreased PAI score) or healed (PAI < 2), were assessed with the Chi-square test. Clinical symptoms and abnormal findings at the 12-month follow-up examination were recorded but not subjected to statistical analysis.
Results and Statistical Analysis
The conventional procedure should produce a success rate of approximately 80%.
Eighty-one teeth in forty-three patients met the inclusion criteria and were included in the study after getting consent from the patients. There were two treatment failures (five teeth) before the 1 year period, one each in Group 2 and Group 3. Periapical surgery was done in one patient due to persistant draining sinus, within 3 months of obturation, other patient had an accident and both teeth had to be extracted because of fracture. Ten patients (16 teeth) were lost to follow-up. We defined failure as the need for any additional treatment before or at the 12-month follow-up evaluation period.
In this study, 60 teeth (Group 1 = 21, Group 2 = 18, Group 3 = 21) presented for the 1 year follow-up examination. Because these numbers were unlikely to be large enough for statistical differences between the groups, a power analysis evaluation was performed.
Agreement between and within examiners was determined by using the ICC. Single and average measure inter-reliability score of 0.91 and 0.95, in this study, represent a very high level of agreement between the examiners.[26]
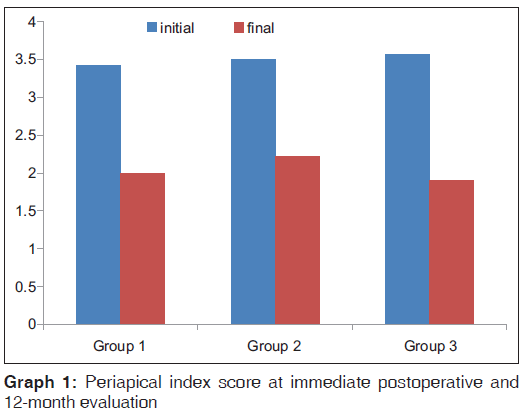
Mean PAI score for Group 1 was 3.42 at baseline and decreased to 2 by the end of 1 year, a decrease of 1.42. Similarly, the decrease in PAI for Group 2 and Group 3 was 1.28 and 1.67, respectively. The decrease in PAI was statistically significant in all groups (P < 0.001) [Table 1 and Graph 1].
| Groups | Immediate postoperative mean PAI (SD) | 1 year recall mean PAI (SD) | Change in PAI score with 95% CI |
|---|---|---|---|
| 1 | 3.42 (0.67) | 2 (1.224) | 1.42 |
| 2 | 3.5 (0.67) | 2.22 (1.35) | 1.28 |
| 3 | 3.57 (0.7859) | 1.90 (1.09) | 1.67 |
Table 1: Periapical index score at immediate postoperative and 12-month evaluation
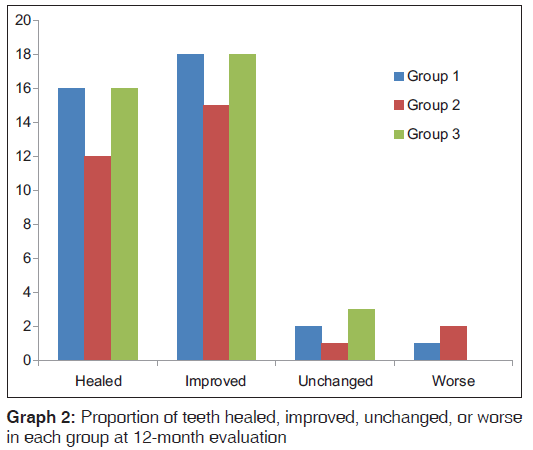
In Group 1 and 3, 76.2% (16/21) teeth could be considered healed (PAI = 2), whereas in Group 2, only 66% (12/18) teeth could be considered healed. There was no statistically significant difference in healing among the groups [Table 2 and Graph 2].
| Status | Group 1 | Group 2 | Group 3 |
|---|---|---|---|
| Healed % (PAI <2) | 76.19 (16/21) | 66.67 (12/18) | 76.19 (16/21) |
| Improved %(decreased PAI) | 85.7 (18/21) | 71.4 (15/21) | 85.7 (18/21) |
| Unchanged %(same PAI) | 9.52 (2/21) | 5.56 (1/18) | 14.29 (3/21) |
| Worse %(increased PAI) | 4.76 (1/21) | 11.11 (2/18) | 0.00 (0/21) |
Table 2: Proportion of teeth healed, improved, unchanged, or worse in each group at 12-month evaluation
Clinical symptoms and abnormal findings at the 12-month follow-up examination were recorded but not subjected to statistical analysis. One tooth in Group 2 was discolored after 1 year except that there were no abnormal findings.
Discussion
AP is one of the most prevalent diseases affecting the teeth. Prevalence increases with age and by the age of 50 years, it is more than 50%.[27] It is equally well established that prognosis for complete healing of teeth with pretreatment diagnosis of AP is approximately 10–15% lower than for teeth without AP.[28,29] With billions of teeth affected with the disease, a treatment regimen, which can result in successful and predictable healing can help save many teeth. This prospective study was done to compare the effectiveness of two commonly used nonsurgical primary endodontic treatment regimens for the treatment of AP, i.e., single visit and traditional multi-visit treatment regimen.
Only teeth with definite periapical lesions (AP) were included in the study making the comparison between treatment protocols viable. The expectation that teeth treated in two visits with an interappointment dressing of Vitapex paste would result in improved healing when compared with one-visit root canal therapy was not supported by this study. No statistically significant differences were found between the three treatment groups in the healing of AP; our findings are consistent with the majority of well-controlled clinical studies.[11,12,30-32] When comparison was done between initial and final (1 year recall) PAI score in each group, statistically significant improvement in PAI score was found in every group (including Group 2), which corroborates the study of Gesi et al.[33] that with proper use of aseptic operating procedures, proper instrumentation, and filling, an inter-appointment dressing with calcium hydroxide does not seem to influence outcome.
Leaving the canal empty without obturation or use of any additional medicament (Group 2) was numerically (though not statistically significant with given sample size) the worst method of treatment, which are consistent with the study of Trope et al.[11]
Main problems with prospective studies are the recall rate, adequate sample size, and control of the baseline status. Sixty teeth out of the original sample of 81 teeth were included in the final analysis with a recall rate of 74% which is more than the median recall rate of 52.7% Ng et al.[34] and Penesis et al.[31] but less compared to the studies by Weiger et al.[12] and Paredes-Vieyra and Enriquez.[32]
Although the sample size in this study was small, it is typical when compared with similar studies,[11,12,30] but the sample size of the present study was not large enough for statistical significance. Because even inferior protocols result in about 60% success, it requires a large sample size to show statistically significant differences in results for different treatment protocols. These numbers are extremely difficult to achieve in a prospective study like this one considering the time constraints, limited resources, and subject dropouts associated with long recall period. To compensate for this problem, a power analysis [35] of the results was performed to calculate the adequate sample size required to make the results clinically significant. In general, a sample size of 49 per group would have resulted in significant differences between the single visit and multiple visit groups.
To minimize the bias, patients were randomly assigned to treatment groups, and root canal therapy was performed according to a standardized regimen. Conventional hand instrumentation was done as it was planned as a baseline study so that subsequently studies using rotary instruments can be done and influence of different techniques compared with the study.
Only anterior teeth were included in the study similar to Sjögren et al.[6] To control the baseline apical status, only teeth with visible radiolucent area of 2.0 mm × 2.0 mm were included similar to Penesis et al.,[31] which assured an initial PAI score =3. The only known independent variable was number of visits and use of Vitapex as intracanal medicament. Fortunately, the number of teeth in each group was reasonably evenly distributed during treatment and after 1 year recall, neither group varied significantly from the study dropouts.
Calcium hydroxide is currently acknowledged as the best intracanal medicament in endodontic treatment procedures. It is effective against most endopathogens but has a limited activity against Candida albicans and Enterococcus faecalis. Leonardo et al.[36] recommended the addition of other substances to the paste to increase or maintain the paste consistency of the material which does not harden or set in the root canal, to improve flow, maintain pH of calcium hydroxide, to improve radio-opacity, to make clinical use easier and not alter the excellent biological properties of calcium hydroxide itself. Hence, Vitapex was used as an intracanal medicament which contains iodoform (synergistic action), silicone oil (silicone oil based calcium hydroxide is effective in the elimination of E. faecalis),[37] and radiopacifiers, which increase the paste radiopacity, which helps in confirming insertion and complete removal from the root canal using radiograph.
Vitapex was placed in the root canals of Group 3 for a period of 7 days before obturation as in the studies by Law and Messer,[9] Siqueira et al.[38] for calcium hydroxide dressings.
After root canal treatment the probability of healing increases over time,[12,39] however periapical changes are evident by 1 year.[40] Orstavik[41] concluded that 1-year follow-up predicts long-term success and the risk of disease development at 2 years or later is not greater than general risk based on epidemiological studies. As the number of dropouts increases with the time and recall rate falls, many studies have used 1-year recall period like the present study.[11,31,42]
Evaluation of results was done using PAI scoring system. PAI scoring system given by Orstavik et al.[22] is based on a histological correlation study of Brynolf[24] with a PAI score of 1–2 defined as healed or minimally inflamed and scores 3–5 defined as diseased. This index was used by 58 studies from 1986 to 2009 and is accepted as a valid tool to determine outcome and reveal changes in bone density after root canal treatment.[43]
However, PAI is still a subjective outcome and is prone to observer variation. To overcome this disadvantage as much as possible, calibration of examiners was done and consensus score was taken as a true score. Agreement between and within examiners was determined by using the ICC. Single and average measure inter-reliability score of 0.91 and 0.95, respectively, in this study, represent a very high level of agreement between the examiners, even before meeting for a consensus score for each image similar to that in the study by Penesis et al.[31]
In most studies, PAI scores are generally dichotomized as healed (PAI 1, 2) and diseased (PAI 3, 4, 5), but it may obscure the small amount of change that may be clinically significant. The process of calibrating observers and arriving at a consensus is also very time-consuming.
Measurement of density as a continuous variable can be more expressive than the PAI scoring system[44,45,46]. Use of digital radiography has added advantages of less radiation exposure, time saving, and freedom from processing errors. However, variations in soft tissue superimposition and physiologic modeling over time may influence the measurements, producing erroneous information.
Nevertheless, the sample and operator may not accurately represent the true population of patients and clinicians. Results can be influenced by many unknown and uncontrolled variables like on an average, every patient contributed two teeth in the study with some patients contributing three or four teeth which increased the dependency of results on subjects. Similarly, diabetic and immune-compromised patients were excluded from the study, but smokers were not despite the evidence that they also experience poorer treatment outcomes.[47,48] All cases in the study were done during the period of postgraduation course (2010–2013) under faculty supervision with the opportunity for consultation and assistance as needed; therefore, the treatment environment might not be truly representative of either specialty or general dental practice setting.
Conclusion
From the present study, it can be concluded that 12 months after initial nonsurgical root canal therapy on teeth with AP, there was no statistically significant difference in periapical healing between single visit treatment and multi-visit treatment with the given sample size.
Acknowledgements
We sincerely acknowledge the support of Dr. Pynshngain Phyllei, Dr. Monali Purkayastha, Dr. Satheesh S. L., Dr. Shefali Jain, Dr. Lakshita Joshi, Dr. Tage Tamo, and non-teaching staff of the Department of Conservative Dentistry and Endodontics, Guwahati.
Financial support and sponsorship
Nil.
Conflicts of interes
There are no conflicts of interest.
References
- Pak JG, Fayazi S, White SN. Prevalence of periapical radiolucency and root canal treatment: A systematic review of cross-sectional studies. J Endod 2012;38:1170-6.
- Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: The Toronto Study. Phase 1: Initial treatment. J Endod 2003;29:787-93.
- Ørstavik D, Pitt Ford TR, editors. Essential Endodontology. Prevention and Treatment of Apical Periodontitis. London: Blackwell Science; 1998.
- Martinho FC, Leite FR, Nascimento GG, Cirelli JA, Gomes BP. Clinical investigation of bacterial species and endotoxin in endodontic infection and evaluation of root canal content activity against macrophages by cytokine production. Clin Oral Investig 2014;18:2095-102.
- Siqueira JF Jr. Endodontic infections: Concepts, paradigms, and perspectives. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:281-93.
- Sjögren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J 1997;30:297-306. Erratum 1998;31:148.
- Byström A, Sundqvist G. Bacteriologic evaluation of the effect of 0.5 percent sodium hypochlorite in endodontic therapy. Oral Surg Oral Med Oral Pathol 1983;55:307-12.
- Rahimi S, Janani M, Lotfi M, Shahi S, Aghbali A, Vahid Pakdel M, et al. A review of antibacterial agents in endodontic treatment. Iran Endod J 2014;9:161-8.
- Law A, Messer H. An evidence-based analysis of the antibacterial effectiveness of intracanal medicaments. J Endod 2004;30:689-94.
- Peters LB, van Winkelhoff AJ, Buijs JF, Wesselink PR. Effects of instrumentation, irrigation and dressing with calcium hydroxide on infection in pulpless teeth with periapical bone lesions. Int Endod J 2002;35:13-21.
- Trope M, Delano EO, Orstavik D. Endodontic treatment of teeth with apical periodontitis: Single vs. multivisit treatment. J Endod 1999;25:345-50.
- Weiger R, Rosendahl R, Löst C. Influence of calcium hydroxide intracanal dressings on the prognosis of teeth with endodontically induced periapical lesions. Int Endod J 2000;33:219-26.
- Fuss Z, Charniaque O, Pilo R, Weiss E. Effect of various mixing ratios on antibacterial properties and hardness of endodontic sealers. J Endod 2000;26:519-22.
- Siqueira JF Jr., Favieri A, Gahyva SM, Moraes SR, Lima KC, Lopes HP. Antimicrobial activity and flow rate of newer and established root canal sealers. J Endod 2000;26:274-7.
- Oliet S. Single-visit endodontics: A clinical study. J Endod 1983;9:147-52.
- Vela KC, Walton RE, Trope M, Windschitl P, Caplan DJ. Patient preferences regarding 1-visit versus 2-visit root canal therapy. J Endod 2012;38:1322-5.
- Albashaireh ZS, Alnegrish AS. Postobturation pain after single- and multiple-visit endodontic therapy. A prospective study. J Dent 1998;26:227-32.
- Eleazer PD, Eleazer KR. Flare-up rate in pulpally necrotic molars in one-visit versus two-visit endodontic treatment. J Endod 1998;24:614-6.
- Sathorn C, Parashos P, Messer HH. Effectiveness of single- versus multiple-visit endodontic treatment of teeth with apical periodontitis: A systematic review and meta-analysis. Int Endod J 2005;38:347-55.
- Figini L, Lodi G, Gorni F, Gagliani M. Single versus multiple visits for endodontic treatment of permanent teeth. Cochrane Database Syst Rev 2007;17(4)CD005296 Cochrane Database Syst Rev. 2007 Oct 17;(4):CD005296 and J Endod 2008;34: 1041–7.
- Su Y, Wang C, Ye L. Healing rate and post-obturation pain of single- versus multiple-visit endodontic treatment for infected root canals: A systematic review. J Endod 2011;37:125-32.
- Orstavik D, Kerekes K, Eriksen HM. The periapical index: A scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol 1986;2:20-34.
- Örstavik D. Reliability of the periapical index scoring system. Eur J Oral Sci 1988;96:108-11.
- Brynolf I. A histological and roentgenological study of the periapical region of human upper incisors. Qdg.ntol Rev1967;18 Suppl 11:1-176.
- Schuurs AH, Wu MK, Wesselink PR, Duivenvoorden HJ. Endodontic leakage studies reconsidered. Part II. Statistical aspects. Int Endod J 1993;26:44-52.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74.
- Erikssen HM. Epidemiology of apical periodontitis. In: Ørstavik D, Pitt Ford TR, editors. Essential Endodontology. Prevention and Treatment of Apical Periodontitis. London: Blackwell Science; 1998. p. 179-91.
- Marquis VL, Dao T, Farzaneh M, Abitbol S, Friedman S.Treatment outcome in endodontics: The Toronto Study. PhaseIII: Initial treatment. J Endod 2006;32:299-306.
- Chugal NM, Clive JM, Spångberg LS. A prognostic model for assessment of the outcome of endodontic treatment: Effect of biologic and diagnostic variables. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:342-52.
- Peters LB, Wesselink PR. Periapical healing of endodontically treated teeth in one and two visits obturated in the presence or absence of detectable microorganisms. Int Endod J 2002;35:660-7.
- Penesis VA, Fitzgerald PI, Fayad MI, Wenckus CS, BeGole EA, Johnson BR. Outcome of one-visit and two-visit endodontic treatment of necrotic teeth with apical periodontitis: A randomized controlled trial with one-year evaluation. J Endod 2008;34:251-7.
- Paredes-Vieyra J, Enriquez FJ. Success rate of single- versus two-visit root canal treatment of teeth with apical periodontitis: A randomized controlled trial. J Endod 2012;38:1164-9.
- Gesi A, Hakeberg M, Warfvinge J, Bergenholtz G. Incidence of periapical lesions and clinical symptoms after pulpectomy – A clinical and radiographic evaluation of 1- versus 2-session treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:379-88.
- Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: Systematic review of the literature – Part 1. Effects of study characteristics on probability of success. Int Endod J 2007;40:921-39.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988. Calculated Using “Pwr” Package of R-Software. Available from: http:// www.r-project.org. the website is still accessible and version R3.2.4 is latest. [Last accessed on 2014 Nov 05].
- Leonardo MR, Leal JM, Simoes Filho AP. Endodontia Tratamento dos Canais Radiculares. Sa Äo Paulo: Panamericana; 1982.
- Han GY, Park SH, Yoon TC. Antimicrobial activity of Ca(OH) 2 containing pastes with Enterococcus faecalis in vitro. J Endod 2001;27:328-32.
- Siqueira JF Jr., Magalhães KM, Rôças IN. Bacterial reduction in infected root canals treated with 2.5% NaOCl as an irrigant and calcium hydroxide/camphorated paramonochlorophenol paste as an intracanal dressing. J Endod 2007;33:667-72.
- Molander A, Warfvinge J, Reit C, Kvist T. Clinical and radiographic evaluation of one- and two-visit endodontic treatment of asymptomatic necrotic teeth with apical periodontitis: A randomized clinical trial. J Endod 2007;33:1145-8.
- Ørstavik D, Qvist V, Stoltze K. A multivariate analysis of the outcome of endodontic treatment. Eur J Oral Sci 2004;112:224-30.
- Orstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J 1996;29:150-5.
- Waltimo T, Trope M, Haapasalo M, Ørstavik D. Clinical efficacy of treatment procedures in endodontic infection control and one year follow-up of periapical healing. J Endod 2005;31:863-6.
- Wu MK, Shemesh H, Wesselink PR. Limitations of previously published systematic reviews evaluating the outcome of endodontic treatment. Int Endod J 2009;42:656-66.
- Carvalho FB, Gonçalves M, Tanomaru-Filho M. Evaluation of chronic periapical lesions by digital subtraction radiography by using Adobe Photoshop CS: A technical report. J Endod 2007;33:493-7.
- Salceanu M, Doncieu C, Maria V, Radu V. Radiodensitometric study regarding conservative endodontic therapy in periapical lesions. Rom J Oral Rehabil 2010;2:10.
- Delano EO, Ludlow JB, Ørstavik D, Tyndall D, Trope M. Comparison between PAI and quantitative digital radiographic assessment of apical healing after endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:108-15.
- Doyle SL, Hodges JS, Pesun IJ, Baisden MK, Bowles WR. Factors affecting outcomes for single-tooth implants and endodontic restorations. J Endod 2007;33:399-402.
- Walter C, Rodriguez FR, Taner B, Hecker H, Weiger R. Association of tobacco use and periapical pathosis – A systematic review. Int Endod J 2012;45:1065-73.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.