Situs Inversus Totalis with Tetralogy of Fallot Complicated with Right Cerebral Abscess
Citation: Wilson E. Sadoh, Olufemi K. Olaniyi, Promise Monday. Situs Inversus Totalis with Tetralogy of Fallot Complicated with Right Cerebral Abscess. Ann Med Health Sci Res. 2017; 7: 29-31
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Situs inversus totalis (SIT) is a rare anomaly in which there is a reversal of abdominal and thoracic organs. The condition may come to light when affected patients who uncommonly have congenital heart disease (CHD), manifest with one. A case of a 10 year old boy with SIT and tetralogy of Fallot (TOF) that was complicated with cerebral abscess is presented. The successful management of the cerebral abscess and the presentation of the anomaly are highlighted.
Keywords
Situs inversus totalis; Tetralogy of Fallot; Cerebral abscess
Introduction
Situs inversus totalis is the complete reversal of the position of the viscerae in the abdominal and thoracic cavities [1]. It is rare and uncommonly associated with CHD. We report a case of SIT with TOF complicated by cerebral abscess in a tertiary centre. The associated complication is highlighted in this report.
Case Report
A 10 year old boy presented to the children’s emergency room with a seven year history of being easily fatigued on exertion and bluish discoloration of the lips, fever and headache of six days duration. A day after the onset of headache, he developed generalised tonic clonic convulsion that lasted 15 minutes and was aborted spontaneously. Subsequently, he had weakness of the left side of the body and inability to walk.
On examination, he was conscious, had conjunctival congestion, central cyanosis and grade 4 digital clubbing. He had a bulge on the right hemi-thorax with the apex beat in the 6th right intercostal space, mid-clavicular line. He had a grade 3/6 ejection systolic murmur loudest over the right mid-sternal border.
Neurological examination showed a left hemi-paresis with grade 3 power on the left upper and lower limbs. He had neither cranial nerve deficit nor signs of meningeal irritation. The other systems were unremarkable. A diagnosis of cyanotic CHD; probably TOF with possible cerebral abscess was made.
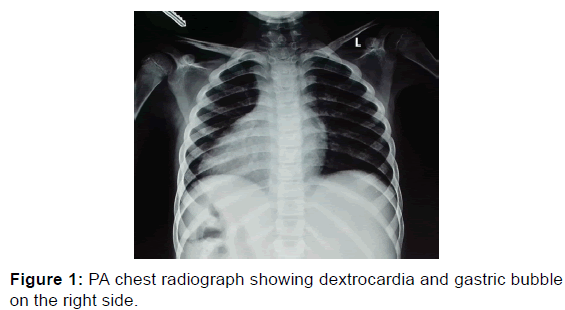
The chest radiograph revealed dextrocardia with a right sided gastric shadow and left sided liver [Figure 1]. Abdominal ultrasound confirmed a reversal of the position of abdominal visceral organs. Liver was located in the left upper quadrant and the spleen on the right upper quadrant. The ileocaecal junction was in the left lower quadrant.
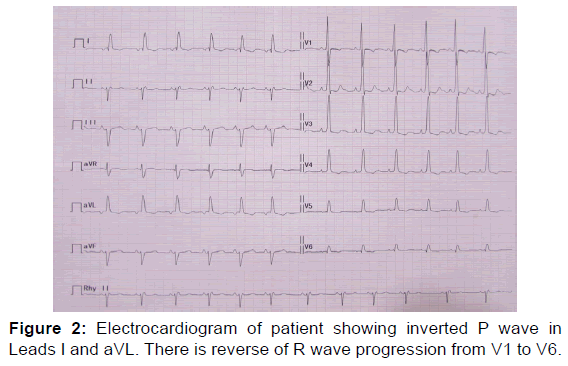
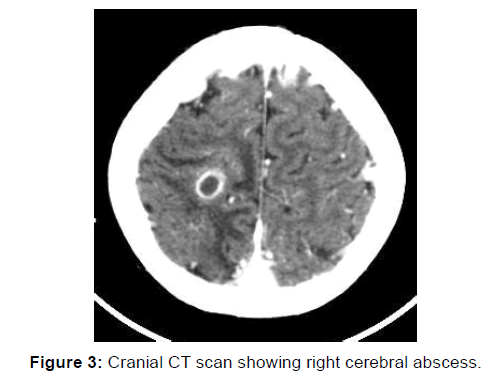
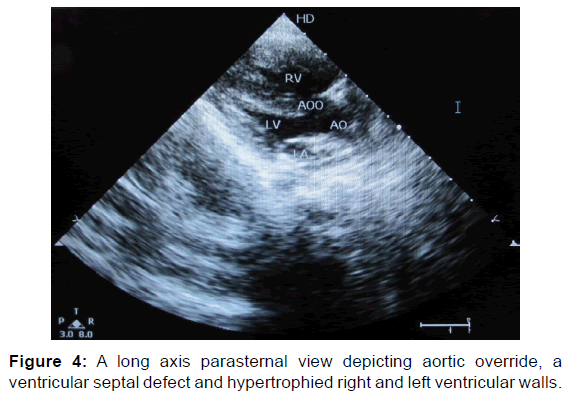
Electrocardiogram (ECG) with normally placed leads revealed a sinus rhythm with inverted p wave in leads I and aVL while it was upright in aVR. There was a reversal of the R wave progression pattern in V1 to V6 [Figure 2]. Echocardiography confirmed dextrocardia, right ventricular hypertrophy, a large ventricular septal defect, pulmonary valvular and infundibular stenosis and overriding aorta [Figure 3]. Cranial CT scan showed a large solitary oval hypodense lesion with ring enhancement and surrounding vasogenic oedema in the right parietal lobe. It measured 3.9 × 4.0 cm, and there was a mild contralateral shift of the midline structures [Figure 4].
The final diagnosis of SIT with TOF, complicated with right cerebral abscess was made. He was commenced on intravenous antibiotics for three weeks. Right parietal borehole drainage of cerebral abscess was done and yielded 20 mls of sterile purulent material. The haematocrit was 71% for which he had partial exchange blood transfusion using normal saline. The postexchange PCV was 50%.
The patient started physiotherapy in the second week of admission and began to ambulate by the third week. He is being prepared for surgical intervention of the CHD on out-patient.
Discussion
In SIT, the organs in both the thorax and abdomen are transposed from their normal position. It is situs inversus partialis when only the position of organs in the abdomen or thorax are reversed. [1] Situs inversus totalis is present in 1/10000 – 1/50000 of the general population [1]. In the abdomen, the liver and gall bladder are on the left while the spleen and stomach are located on the right, [1] as was demonstrated in the chest radiograph and ultrasound evaluations of this patient. Dextrocardia was also shown on the chest radiograph.
The exact cause of SIT is not known. It seem to result from the clockwise rather than the counter clockwise embryonic rotation of the midgut resulting in mirror image positioning of the internal organs [2].
In SIT, individuals are phenotypically normal. The anomaly comes to light by accident when they present to medical facilities for unrelated conditions as was the case in this report [2]. Situs inversus totalis may form part of Kartagener syndrome, in which the other components are sinusitis and bronchiectasis. [1] The present case did not have these other conditions.
Structurally normal heart is seen in SIT with only 3-5% of patients having co-existing CHD as against the relatively high incidence of CHD seen in situs inversus with levocardia [1,3]. Previous case reports had mostly normal hearts or transposition of great arteries or TOF when a CHD was present [1,4]. The index patient has TOF, complicated by cerebral abscess. Cerebral abscess is a common complication of cyanotic CHD as has been previously reported [5].
This case was complicated by cerebral abscess because of the long standing uncorrected TOF [6]. Serious neurologic complications in an uncorrected TOF include cerebral thromboses and brain abscess. The former occur most often in patients younger than 2 years because of polycythemia and dehydration while the later usually occur in patients older than 2 years [6]. as was in the present case being a 10 year old with polycythemia.
The diagnosis of SIT can be confirmed on chest radiographic and ultrasonographic evaluations as was demonstrated on the chest radiograph, echocardiogram and abdominal ultrasound findings of this patient. Other modalities of imaging such as CT with contrast and MRI can be useful in difficult cases. They are the most reliable methods of confirming abscess formation in the brain as was demonstrated in this patient. Abnormal findings such as the inverted P wave in lead I and aVL and the reverse R wave progression in the chest leads are subtle pointers to dextrocardia. It is pertinent to note that reversal of R wave progression with evidence of right ventricular hypertrophy is a normal finding in TOF. Early, identification of individuals with SIT is important to avoid catastrophes during surgery as target organs for potential surgery are located in opposite position of normal. It is noteworthy that prompt and adequate management of the cerebral abscess ensured the survival of the patient.
Conclusion
A case of Situs Inversus Totalis of a 10 year old boy with TOF that was complicated by cerebral abscess because of the longstanding uncorrected CHD is reported. The successful management of the complication is highlighted.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Maldijian PD, Saric M. Approach to dextrocardia in adults. Review. Am J Roentgenol 2007; 188:S39- S49
- Chin AJ. Heterotaxy syndrome and primary ciliary dyskinesia. Published May 2014; http://emedicine.medscape.com/article/896757-overview#showall Accessed November 20th, 2016.
- Ramrakha P, Hill J, eds. Congenital heart disease. In: Oxford Handbook of Cardiology. 2nd ed. Oxford, UK: Oxford University Press; 2012:596
- Uchenna DI, Jesuorobo DE, Anyalechi JI. Dextrocardia with situs inversus totalis in an adult Nigerian: a case report. Am J Med Med Sci 2012; 2: 59-61
- Basheer M, Agarwalla SK. A rare association of pentalogy of Fallot with situs inversus totalis complicated by brain abscess in an adolescent – case report. J CLin Diag Res 2016; 10: SD06-SD07 Doi:10.7860/JCDR/2016/23712.9098
- Bernstein D. Cyanotic congenital heart lesions: Lesions associated with decreased pulmonary blood flow. In: Kliegman RM, Behrman RE, Jenson HB (eds.) Nelson Textbook of Pediatrics. 19th ed. WB Saunders Elsevier, PA: Philadelphia, USA. 2011;424:1573-1578.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.