Sleep, Sleepiness and Medical College Students: A Comparative Study among Medical and Paramedical Students of a Tertiary Care Teaching Hospital from a West Indian Metropolitan City
- *Corresponding Author:
- Arun Chutani
Department of Physiology, SETH G.S. Medical College and K.E.M. Hospital, Parel, Mumbai, India.
Tel: 9101412754388
E-mail: docarun26@gmail.com
Citation: Chutani A, Shenvi DN, Singhal A. Sleep, Sleepiness and Medical College Students: A Comparative Study among Medical and Paramedical Students of a Tertiary Care Teaching Hospital from a West Indian Metropolitan City. Ann Med Health Sci Res. 2017; 7:85-91.
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Background: Behavioural, physiological and neurocognitive processes occur during sleep which can be impaired by the absence of sleep. Accommodation and travelling stress can additionally compromise sleep duration along with the demanding curriculum. Aim: To compare sleep quality and quantity of medical versus paramedical and hostellers versus day scholar students of a Medical college in a metropolitan city. Subjects and Methods: Validated questionnaires (PSQI, ESS and Sleep 50) along with sleep diary and demographic sheet were used to study sleep duration, daytime sleepiness and sleep associated problems in 271 students of medical and paramedical course. Results: Study group included MBBS (76.4%, 207/271) and OT/ PT (23.6%, 64/271) students. Average (SD) sleep duration for MBBS students was 6:38 hrs (52 minutes) and of OT/PT students was 7 hrs (46 minutes). Short sleepers were 47.9% (130/271) students with 21% (57/271) sleeping <6 hours per day. Travel time of Hostellers was a maximum 40 minutes while day scholars was up to 4 hours/day. Poor sleep quality was reported by 20.7% students and Excessive Day time Sleepiness (ESS) by 24.4% students. More number of MBBS day scholars reported poor sleep quality and ESS than the hostellers. No student reported any sleep disturbance. Conclusion: The pressure of first year curriculum, transition to medical curriculum coupled with long and strenuous travel time take a toll on the sleep physiology of the medical students. College authorities have a limited role in this as a metropolitan city is saturated in terms of accommodation facilities. It is a social, academic and administrative problem.
https://bluecruiseturkey.co
https://bestbluecruises.com
https://marmarisboatcharter.com
https://bodrumboatcharter.com
https://fethiyeboatcharter.com
https://gocekboatcharter.com
https://ssplusyachting.com
Keywords
PSQI, ESS, Sleep-50, Sleep quality, Sleep duration
Introduction
Sleep is an active, repetitive and reversible behaviour vital for health and life. Behavioural, physiological and neurocognitive processes occur during sleep which are susceptible to be impaired by the absence of sleep.[1,2] Sleep quality as well as quantity is strongly related to psychological and physical health and other measures of well‑being.[3,4] The architecture and internal structure of sleep is a function of age in apparently healthy individuals, although other factors may contribute to it. The requirement of sleep in most adults is approximately seven to eight hours, per night.[5,6] Deprivation of sleep and disturbance of the circadian rhythm can seriously impair daytime functioning. Overall, human sleep deprivation experiments have proven that sleep deprivation causes sleepiness and impairment of performance, vigilance, attention, concentration, reduced energy levels, altered immune function, poor wound healing, mood changes (increased impatience and irritability), increased risk of depression or anxiety, and a higher occurrence of accidents and falls.[2,7-9] Deprivation of sleep, which is a striking problem of the modern society, leads to detrimental effects on the hormonal, metabolic and immunological profile of an individual.[2]
The adverse effects of sleep deprivation are also clearly visible in the younger generation as well. College years are a transition time, a time when students experience a significant increase in autonomy and start assuming responsibilities as young adults. [10] Hence, students often consider their first year of college as a major stressful period in their lives due to academic curriculum and other factors associated with college life affecting the sleep.[6]
Sleep is of particular interest in medical students because of the relationship between sleep and stress and the potential impact of stress on learning the art of quality patient care. Cognition and fine learning skills are impaired due to sleep loss creating lacunae in learning the technical aspects of medical academic curriculum and patient care.[2,6] It has been shown that short sleep duration, poor sleep quality and loss of sleep, all, have negative impact on the academic performance of the medical students.[2,6,9,11-13]
There can be a many social factors that can affect and worsen the stress of medical college students, which have not been highlighted or studied in previous similar researches. Of particular note are the living conditions in a metropolitan city such as housing, hostel accommodations and travelling long distances in the event of costly accommodations in the heart of the city thereby adding to the already compromised sleep of the medical students. In the Western Indian metropolitan city where this study was done most students generally live in the suburbs due to the exorbitant prices and rent of housing in the centre of the city. The irony of the situation is that Medical colleges are located in the heart of the city with costly neighbourhoods which many can’t afford. Hence housing and long-distance travelling become significant social factors that add to the stress of a demanding academic curriculum and in effect translate into inability to obtain adequate rest causing sleep deprivation. Along with this is the added stress of commuting in the overburdened and time consuming local transport system.
This study attempts to assess the sleep patterns in first year medical and paramedical students of a Medical college in the backdrop of a West Indian metropolitan city known for its pressures on daily life. It also attempts to compare and comment on the sleep quality and quantity of medical versus paramedical and hostellers versus day scholars in particular reference to the amount of time spent in travelling to and from the medical college.
Materials and Methods
This study was conducted from January 2013 to March 2014 in the Department of Physiology of this particular medical college. The study group included students of first year Bachelor of Medicine and Bachelor of Surgery (MBBS) and First year physiotherapy (PT) and occupational therapy (OT).
The sample population was selected after careful deliberation of the fact that first year students are the transitional ones between a premedical and medical curriculum and hence face maximum difficulties in terms of the academic stress and transitional lifestyle. This will in great likelihood effect the sleep physiology of this particular cohort/group of medical students hence they form the ideal population for this particular study.
In light of the earlier studies, the minimum sample size was calculated to be 250,[14,15] employing the following formula(based on central limit theorem):
n = Z21-α/2 p(1-p) / d2
where, p: expected proportion = 0.63
d: absolute precision = 5
1 -α/2: desired confidence level = 93
Institutional ethics committee approval was duly taken for the study.
A sleep diary to gather data about the sleep duration and sleep schedule was provided to the study population and collected after 3 weeks. Subsequently, the participants were handed ‘sleep survey packets’ containing a demographic sheet and 3 pre-validated, pretested and standardised questionnaires. This served as internal control for each other. The 3 questionnaires employed were for testing and investigating the sleep patterns and abnormalities, if any.
• Pittsburgh sleep quality index (PSQI) questionnaire was used for studying the sleep quality, and a score of more than 5 in PSQI indicates poor sleep quality in the past month.
• Epworth sleepiness scale (ESS) questionnaire was used to study the daytime sleepiness; a score of more than 10 depicts increased day time sleepiness.
• Sleep 50 questionnaire was used to study sleep associated problems. This is significant only if a score of ≥ 15 is present on impact. Sleep 50 is important in highlighting organic sleep disorders and those arising from psychiatric conditions rather than physiological sleep abnormalities or disturbances.
The definition of sleep duration was taken as the sum total of sleep time during the night and the total duration of the day time naps.
Based on the sleep duration sleeping time of < 7 hours/day was considered ‘Short Sleep’, > 8 hours/ day as ‘Long Sleep’ and between 7-8 hours/day was considered as ‘Average Sleep’.
After a successful pilot run on a small fraction of students (25) for the feasibility of the study it was projected onto the larger study group.
Exclusion criteria included students having any chronic illness, undergone any major surgery in past one year, taking drugs like steroids or hormones or had any acute illness in past one month. All students without exclusion criteria and willing to participate in the study were included in the study.
A total of 300 students (230 MBBS + 70 OT/PT) were willing to participate in the study after the exclusion criteria were met.
Informed consent was taken from all the 300 participants before handing them the sleep diary and sleep survey packets.
The data was gathered after 3 weeks and scrutinised and analysed.
Statistical analysis was done using SPSS version 16.0 (SPSS Inc. USA- Chicago). Correlation between the groups and parameter were studied using Pearson’s method and chi square test was used to study significance of observations. Statistical significance was considered at p value<0.05.
Results
After consideration of the exclusion criteria and the consent of the participants, 300 sets of sleep diary and sleep survey packets were distributed to the study group. Of these 300 packets, 278 packets were returned but only 271 (90.3%) were completely filled. Among these 271 students, 207 (76.4%) were MBBS students and 64 (23.6%) were OT/PT students.
Among the 271 students 142 (52.4%) were males and 129 (47.6%) were females. In the MBBS course males (57%, 118/207) were more than females (43%, 89/207) whereas in OT/PT course the number of females (62.5%, 40/64) surpassed males (37.5%, 24/64).
Age of students participating in the study ranged from 18 to 23 years with the mean (SD) age of 18.8 (0.98) years.
In the study group 52.4% (142/271) students were hostellers and 47.6% (129/271) were day scholars [Table 1].
| Sleep Duration/Residence | Short Sleepers | Average Sleepers | Long Sleepers | p-value | |||
|---|---|---|---|---|---|---|---|
| <6 hrs | 6-7hrs | 7-8 hrs | 8-10 hr, >10hrs | ||||
| MBBS (207) | Day scholars (76) | 28 (36.8%) | 28 (36.8%) | 19 (25%) | 1 (1.3%) | <0.0001 | 0.041 |
| Hostellers (131) | 21 (16%) | 32 (24.4%) | 76 (58%) | 2 (1.5%) | |||
| Total | 49 (23.7%) | 60 (29%) | 95 (45.9%) | 3 (1.4%) | |||
| OT/PT (64) | Day scholars (53) | 6 (11.3%) | 11 (20.8%) | 35 (66%) | 1 (1.9%) | 0.56 | |
| Hostellers (11) | 2 (18.2%) | 2 (18.2%) | 6 (54.5%) | 1 (9.1%) | |||
| Total | 8 (12.5%) | 13 (20.3%) | 41 (64.1%) | 2 (3.1%) | |||
OT/PT-Occupational Therapy / Physiotherapy students, hrs-hours
Table 1: Sleep duration in MBBS and OT/PT students.
Of the MBBS students 23.7% (49/207) were sleeping less than 6 hours while only 12.5% (8/64) of OT/PT were in this category; and the difference was found to be statistically significant (p value=0.04). Statistically significant difference was observed in sleep duration between hostellers and day scholars of MBBS group with more number of day scholars sleeping for shorter duration (p value<0.0001) [Table 1].
Average sleep duration for day scholars was less than the hostellers in the MBBS students and it was statistically significant with p value=0.02 and 0.0008 for male and female students respectively. No such difference was observed in the OT/PT students group [Table 2].
| Course | Gender | Day scholars (mean +std dev.) |
Hostellers (mean +std dev.) |
p value |
|---|---|---|---|---|
| MBBS | Male | 6hrs + 45mins | 6:50hrs + 50 mins | 0.02* |
| Female | 6:15hrs + 40 mins | 7hrs + 40mins | 0.0008* | |
| OT/PT | Male | 7hrs + 45mins | 6:50hrs + 50 mins | 0.90 |
| Female | 7hrs + 45mins | 7:15hrs + 55 mins | 0.60 |
OT/PT-BOTH and BPTH students, hrs ? hours, std dev.- standard deviation, * -significant
Table 2: Gender and Residence based comparison of Sleep duration in MBBS and OT/PT groups.
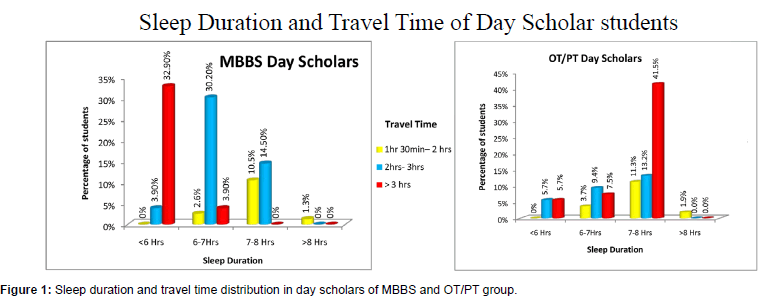
On analysis of the demographic data for travel time, hostellers had a maximum travel time of 40 minutes to and from combined, while day scholars travel time was up to 4 hours/day [Figure 1].
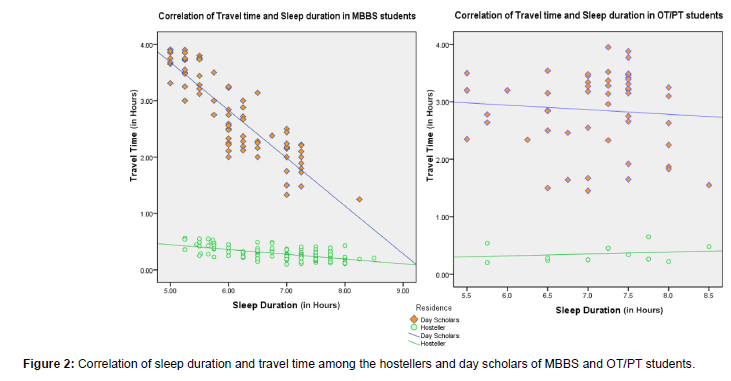
Figure 2 shows correlation of sleep duration and travel time among the MBBS hostellers and day scholars with an obvious effect of travel time on sleep duration in the MBBS day scholar group but not so in the MBBS hostellers and also the OT/PT group.
Poor sleep quality, as observed using raised Global PSQI score, was seen in 31.6% (24/76) day scholars as compared to 19.1% (25/131) hostellers of MBBS group with no such difference in OT/PT students [Table 3].
| Global PSQI Score | Normal Score (<5) | Raised Score (>5) | p-value | ||
|---|---|---|---|---|---|
| MBBS (207)n (%) |
Day scholars (76) | 52 (68.4%) | 24 (31.6%) | 0.04 | 0.02 |
| Hostellers (131) | 106 (80.9%) | 25 (19.1%) | |||
| Total | 158 (76.3%) | 49 (23.6%) | |||
| OT/PT (64) n (%) |
Day scholars (53) | 48 (90.6%) | 05 (9.4%) | 0.4 | |
| Hostellers (11) |
09 (81.8%) | 02 (18.2%) | |||
| Total | 57 (89.1%) | 07 (10.9%) | |||
OT/PT-Occupational Therapy / Physiotherapy students, n ? number
Table 3: Residence and Course wise-Global PSQI scoring.
ESS questionnaire based analysis showed 35.5% (27/76) day scholars having increased day time sleepiness as compared to 22.9% (30/131) of the hostellers with a significant difference among the two groups as depicted by p value=0.04 [Table 4].
| ESS Score | Normal Score (<10) |
Raised Score (>10) |
p value | ||
|---|---|---|---|---|---|
| MBBS (207)n (%) |
Day scholars (76) | 49 (64.5%) | 27 (35.5%) | 0.04 | 0.02 |
| Hostellers (131) | 101 (77.1%) | 30 (22.9%) | |||
| Total | 150 (72.5%) | 57 (27.5%) | |||
| OT/PT (64) n (%) |
Day scholars (53) | 45 (90.6%) | 08 (9.4%) |
0.6 | |
| Hostellers (11) |
10 (90.9%) | 01 (9.1%) |
|||
| Total | 55 (85.9%) | 09 (14.1%) | |||
OT/PT-Occupational Therapy / Physiotherapy students, n ? number
Table 4: Residence and Course wise-ESS scoring .
In the present study, no student reported high enough scores on Sleep-50 questionnaire to label any sleep disturbance warranting medical intervention.
Discussion
The present study was undertaken on 300 students, but only 271 students, including 207 MBBS students and 64 OT/PT students, completely filled the study questionnaires and the sleep diary.
In the present study, average (SD) sleep duration of MBBS students was 6:38 hours (52 minutes) and of OT/PT students was 7 hours (46 minutes). This observation of shorter sleep duration in medical students is in congruence with the findings of various researchers.[6,12,16]
In the study group of 271 students, 47.9% (130) were short sleepers of which 83.8% (109/130) belong to the MBBS group. Overall 52.6% (109/207) of the MBBS students were short sleepers. Zailinawati et al. reported similar findings of 49% medical students sleeping less than 7 hours while Giri et al. reported short sleep duration in even higher number of medical students (80%).[3,16]
On further stratification of the data it was observed that almost 21% (57/271) of the total group was sleeping <6 hours per day of which 86% (49/57) were of the MBBS group [Table 1]. Unfortunately, students are often ignorant of the deleterious effects of sleep deprivation on their cognitive and intellectual domains.[6,13] Lack of sleep also affects a person physically, degrading their coordination and agility.[6,17] In some studies, sleepiness has been linked to as much as 42% of automobile fatalities.[2,9]
Among the MBBS group more number of day scholars (73.7%, 56/76) were short sleepers as compared to the hostellers (40.5%, 53/131) and the difference was found to be statistically significant (p value<0.0001).
From observation and analysis regarding the distance of residence from the medical school and travel time taken by the day scholars of MBBS group it was observed that 36.8% (28/76) of the day scholars were travelling for duration of more than 3 hours per day while the travel time of the hostellers was a maximum of 40 minutes. Hostellers thereby tend to make up for the lost sleep time at night more easily during the day even though their sleep hours are more erratic and their involvement in the extracurricular activities is more.[18] This is due to the proximity of the living accommodations provided to them by the medical college as compared to the day scholars, who cannot be granted the same due to administrative reasons.
For the day scholars, however, there is added burden of time lost in travelling besides the academic curriculum which keeps the students from obtaining appropriate sleep. Travel time and academic curriculum are the two-constant unchangeable non-modifiable factors that cannot be compromised or cut short. Other modifiable factors such as the social interaction and lifestyle and extracurricular activities can be modified to accommodate the above mentioned two non-modifiable factors. The social interaction can be cut short to a limited extent only. Students go back home and interact with their parents over dinner or meet their peer group which helps them to ventilate themselves emotionally and mentally. This interaction generally takes place during the late hours of the evening only as parents and/or peers also come home late from work/colleges. Thus, often students have to choose between social interaction and sleep which leads to an unavoidable compromise of the other.
In the study group, 20.7% (56/271) students reported poor sleep quality. MBBS students showed poor sleep quality in 23.6% (49/207) students which was significantly higher than OT/PT students (10.9%, 7/64) [Table 3]. Various published researches show poor sleep quality in as less as 7% to as high as 64% medical students.[2,6,12-14,16,19-22] Poor Sleep Quality is linked to increased tension, irritability, depression, confusion and generally lower sleep satisfaction.[11,23]
Most researchers have reported poor sleep quality in high number of medical students, stressing the reason to be the demanding academic aspects of the medical curriculum in a limited time period.[12-14,19] Our study takes these observations one step further and substantiates it with ample data. The novel aspect of our study is that it explored the added burden of travel time as an important social factor affecting the sleep duration and quality of the day scholar medical students besides an overburdened medical curriculum in this metropolitan city. This aspect has not been highlighted in the previous studies on this topic.
The residence based observations of PSQI scores showed that MBBS day scholar group had a higher percentage of students with poor sleep quality than the hostellers which was statistically significant at p value=0.04 [Table 3]. This observation holds significance in the view of the architectural layout and population density of a metropolitan city which takes its toll on day scholar students in addition to the stressful MBBS course they are undergoing. The high cost of living around the medical college forces the families of day scholars to take up residence in far out suburbs which was substantiated by the data from the demographic sheet. Thus, the long travelling distance and the high population density pressure on the public transport system makes travelling prolonged and tedious, leading to both stress and loss of productive hours. Productive hours here imply time that could be utilised for meaningful work/ studies or time that could be used for rejuvenating rest or social activities.
Giri et al. have reported sleep quality better in females than males.[3] However the present study (from the analysis of PSQI score) did not observe any gender based difference in sleep quality, which is similar to observations by Abdussalam et al.[19]
Excessive day time sleepiness (EDS), indicating sleep loss, as assessed by ESS questionnaire was seen in 24.4% (66/271) of the total study group. Researchers have reported that Sleep loss, as measured by a raised score of more than 10 on ESS, negatively impacts academic performance in medical students.[6,12]
In the present study, a raised ESS was seen in 27.5% of the MBBS students which was significantly higher than 14.1% in OT/PT students [Table 4]. This observation for MBBS students’ correlates well with the study by Bahamman et al. who reported raised ESS in 22.4% and 21% medical students respectively. [6,14] Abdussalam et al. and Giri et al. reported poor ESS scores in 32.88 % and 30.6% of medical students respectively.[3,19] Zailinawati et al. reported observed that daytime sleepiness occurred in 35.5% of medical students and that two-third of the respondents (65.4%) reported moderate to high chance of dozing during the afternoon lecture.[16] Similar observations were also reported by Bahammam who said that 68.8% medical students reported sleepiness during classes.[24]
On analysing ESS data based on gender of student, no significant correlation was found in the present study which is similar to the observations of Abdussalam et al.[19]
However, analysis based on residential data of the students, showed that more number of MBBS day scholars reported poor ESS [Table 4]. This finding was significant. The completeness of quality rest, that the night time sleep is supposed to provide, is lost due to the lingering fatigue caused by travelling long distance daily and demanding academic work. This manifests as excessive day time sleepiness/craving for sleep in day scholars, which perpetuates as a vicious cycle of under-rest and day time sleepiness.
In the present study, no student reported high enough scores on Sleep-50 questionnaire to label any sleep disturbance warranting medical intervention while Veldi et al. reported the prevalence of habitual leg restlessness (22%), nightmares (8%), sleeptalking (<9.9%) and sleepwalking (<0.5%) in their study and Chinawa et al. have observed that almost 11.3% of the medical students experienced unusual sleep behaviours such as sleep walking, talking or night terrors.[20,25]
If these compromised sleep patterns are compared with eating habits or the sports activities over a period of time, then it can be area of further research which may point out life style illness or disorders in the long run in the same cohort. This extrapolation needs to be further investigated and compared between hostellers and day scholars in light of many other factors.
The sample size of the present study is a good representation of population of medical students. Nevertheless, as the sample size of any study increases, then statistically speaking, variations in the results are bound to happen as extreme behaviours on both sides of the spectrum also fall under the normal distribution of the population. In other words, increasing the sample size of a study makes the distribution of values more Gaussian or symmetrical in nature around the mean distribution. This is a potential limitation of the study and also opens the area of further research if the same study is conducted in a broader set up in a multi-centric way and across the realm of similar academically demanding courses.
Conclusion
All factors remaining the same, travelling time and stress due to the overburdened and crowded local commutation system emerges as the significant variable that not only affects but disrupts the sleep quality and shortens sleep duration to a significant extent, and may have long term implications that need to be explored in greater detail. It also forms an area of further research in terms of policy discussion and curriculum formation. This is a factor that is not in the hands of any student as it is such a social factor that has to be looked into from a bigger perspective.
The MBBS student’s academic curriculum is more demanding on the students’ time and sleep than the paramedical courses. The shortened time duration of first year curriculum, transition from a premedical to medical curriculum coupled with irredeemable social factors such as the long and strenuous travel time mentioned above take a toll on the sleep physiology of the medical students.
College authorities also have a limited role in its correction as the problem of hostel accommodation is redeemable only to a limited extent in a metropolitan city that is saturated in terms of housing and accommodation facilities.
In light of this discussion, the study has a social relevance in terms of the potential academic & health implications on medical students and highlights a problem which cannot be approached from just one side. In the heart of this issue are the medical students who are the doctors of tomorrow. It is a social, academic and administrative problem.
References
- Curcioa G, Ferraraa M, Gennaroa LD.Sleep loss, learning capacity and academic performance. Sleep Med Rev.2006;10:323-337.
- Moura de Araújo MF, Lima CS, Alencar PG, Moura de Araújo T, Fragoso VC, Damasceno MC. Sleep quality assessment in college students from Fortaleza-CE. Text Context Nursing, Florianópolis.2013;22:352-360.
- Giri PA, Baviskar MP, Phalke DB. Study of sleep habits and sleep problems among medical students of Pravara institute of medical sciences loni, western maharashtra, india. Ann med health sci res. 2013;3:51-54.
- Rehulková H, Rehulková O. Quality of sleep in college students. School Health.2011;21:121-127.
- Czeisler CA, Winkelman JW, Richardson GS.Harrison?s principle of Internal Medicine 18th edn, 2012;1:213.
- Surani AA, Zahid S, Surani A, Ali S, Mubeen M, Khan RH. Sleep quality among medical students of Karachi, Pakistan. JPMA. 2015;65:380-382.
- Barker TM. A Description of sleep patterns and sleep hygiene practices for adults in cardiac rehabilitation programs in Southern Montana. Montana State University, Bozeman, Montana April 2008.
- Hill LE, Cumming RG, Lewis R, Carrington S, LeCouteur DG. Sleep disturbances and falls in older people. J Gerontol. 2007;62:62-66.
- Siddiqui AF, Al-Musa H, Al-Amri H, Al-Qahtani A, Al-Shahrani M, Al-Qahtani M. Sleep patterns and predictors of poor sleep quality among medical students in King Khalid University, Saudi Arabia. Malays J Med Sci. 2016;23:94-102.
- Clegg-Kraynok MM, McBean AL, Montgomery-Downs HE. Sleep quality and characteristics of college students who use prescription psychostimulants nonmedically.Sleep Med. 2011;12:598-602.
- Lemma S, Berhane Y, Worku A, Gelaye B, Williams MA. Good quality sleep is associated with better academic performance among university students in Ethiopia. Sleep Breath. 2014;18:257-263.
- Brick CA, Seely DL, Palermo TM. Association between sleep hygiene and sleep quality in medical students. Behav Sleep Med. 2010;8:113-121.
- James BO, Omoaregba JO, Igberase OO. Prevalence and correlates of poor sleep quality among medical students at a Nigerian university. Ann Nigerian Med. 2011;5:1-5.
- Bahamman AS, Al-khairy OK, Al-Taweel AA. Sleep habits and patterns among medical students. Neurosciences.2005;10:447-450.
- Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166:1689-1692.
- Zailinawati AH, Teng CL, Chung YC, Teow TL, Lee PN, Jagmohni KS. Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia 2009;64:108-110.
- Baldus BR. Sleep patterns in U.S. Navy recruits: An assessment of the impact of changing sleep regimens. Master?s thesis 2002.
- Lau EY, Wong ML, Ng EC, Hui CC, Cheung SF, Mok DS. "Social jetlag" in morning-type college students living on campus: Implications for physical and psychological well-being. Chronobiol Int. 2013;30:910-918.
- Abdussalam, Salman MT, Gupta S, Trivedi M, Farooqi M. Poor quality of sleep and its relationship with depression in first year medical students. Adv Life Sci Technol. 2013;12:17-21.
- Veldi M, Aluoja A, Vasar V. Sleep quality and more common sleep-related problems in medical students. Sleep Med. 2005;6:269-275.
- Nojomi M, Bandi MF, Kaffashi S. Sleep pattern in medical students and residents. Arch Iran Med. 2009;12:542-549.
- Wang L, Qin P, Zhao Y, Duan S, Zhang Q, Liu Y, et al. Prevalence and risk factors of poor sleep quality among Inner Mongolia Medical University students: A cross-sectional survey. 2016;244:243-248.
- Brown FC, Soper B, Buboltz WC. Prevalence of delayed sleep phase syndrome in university students. College Student Journal. 2001;35:472.
- BaHammam AS, Alaseem AM, Alzakri AA, Almeneessier AS, Sharif MM. The relationship between sleep and wake habits and academic performance in medical students: A cross-sectional study. BMC Med Edu. 2012;12:61.
- Chinawa JM, Chukwu BF, Obu HA. Sleep practices among medical students in Pediatrics Department of University of Nigeria Teaching Hospital, Ituku/Ozalla, Enugu, Nigeria. Niger J Clin Pract. 2014;17:232-236.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.