Smoking and Severity of COVID-19 Infection: A Short Systematic Review and Meta-analysis
2 Medical Intern, University of Bisha, Bisha, Saudi Arabia
3 Medical Intern, Alfarabi College, Riyadh, Saudi Arabia
4 Medicine Resident, King Fahad Hospital, Albaha, Saudi Arabia
5 Medical Intern, Ibn Sina National College, Jeddah, Saudi Arabia
6 Medical Intern, Imam Muhammad Ibn Saud Islamic University, Riyadh, Saudi Arabia
7 Medical Intern, Shaqra University, Riyadh, Saudi Arabia
8 Pediatric Surgery Resident, MCH Dammam, Dammam, Saudi Arabia
9 Medicine Resident, MGH Madinah, Madinah, Saudi Arabia
10 Resident Physician, Ad Diriyah Hospital, Riyadh city, Saudi Arabia
Citation: Alghamdi SA, et al. Smoking and Severity of COVID-19 Infection: A Short Systematic Review and Meta-analysis. Ann Med Health Sci Res. 2020;10:1083-1088.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: There has been sizeable speculation regarding the association between the severe Acute breathing Syndrome Coronavirus 2 (SARS-CoV-2) pathogen, coronavirus disorder (COVID-19), and smoking. Aim: This work aims to determine the link between smoking and COVID-19 infection. Materials and Methods: A systematic search was performed over different medical databases to identify Internal Medicine studies, which studied the outcome of the Smokers group versus the Non-Smokers group of COVID-19 patients. Using the meta-analysis process, either with fixed or random-effects models, we conducted a meta-analysis on the prevalence of severe cases as a primary outcome, and on mortality rate as a secondary outcome. Results: Eleven studies were identified involving 146793 patients, 11973 in the Smokers group, and 134820 in the Non-Smokers group. The meta-analysis process revealed that the pooled prevalence of severity among COVID-19 patients was (27.7%), and there is a significant increase in COVID-19 severe cases in the Smokers group compared to the Non-Smokers group (OR=2.11, P=0.032). The pooled mortality rate among COVID-19 patients was (17.2%), and there is a significant increase in mortality in the Smokers group compared to the Non-Smokers group (OR=1.76, P=0.026). Conclusion: To conclude, Patients with any smoking history are vulnerable to severe COVID-19 and worse in-hospital outcomes. In the absence of current targeted therapies, preventative and supportive strategies to reduce morbidity and mortality in current and former smokers are crucial.
Keywords
Smoking; Severity COVID-19; Mortality
Introduction
Coronavirus disease 2019 (COVID-19) is now a declared pandemic caused by intense acute respiratory syndrome coronavirus 2 (SARS-CoV- 2). Due to its extremely high infectivity, COVID-19 has caused over 292 142 infections and 12 784 deaths worldwide as of twenty-two March 2020 (world health company coronavirus disorder situation reports). SARSCoV- 2 primarily invades the pulmonary alveolar epithelial cells. although most infections with SARS-CoV-2 are thought to be subclinical or mildly symptomatic, it could result in acute respiratory distress syndrome and occasionally into multiorgan failure. [1]
As the COVID-19 pandemic accelerates, governments are warning people at high hazard to be particularly stringent in observing social distancing measures because if they turn out to be ill they’re much more likely to need critical care including ventilation and to die. most information on COVID-19 are from China, and although most showed cases have been classified as mild or moderate, 14% are severe and 5% important.2 Case fatality rates are difficult to evaluate with reality but could be as high as 1%, that is much greater than seasonal influenza at about 0.1%. [2]
There has been sizeable speculation regarding the association between the severe Acute breathing Syndrome Coronavirus 2 (SARS-CoV-2) pathogen, coronavirus disorder (COVID-19), and smoking. We provide an outline of the available literature regarding the association among smoking, the threat of SARSCoV- 2 infection, and hazard of extreme COVID-19 and poor scientific effects, intending to inform public health policy and exercise, particularly in England. [3]
The harms of tobacco use are well-established. Tobacco causes eight million deaths each yr from cardiovascular sicknesses, lung disorders, cancers, diabetes, and hypertension. Smoking tobacco is also a known risk thing for intense disorder and dying from many respiratory infections. Within the COVID-19 pandemic, questions have been asked about scientific outcomes for smokers, and whether they are equally susceptible to contamination, and if nicotine has any biological impact on the SAR-CoV-2 virus (the virus that causes COVID-19). At the time of writing, one medical trial to check the consequences of nicotine has been introduced, but no trial registration record was found as of 12 May 2020. [4]
This work aims to determine the link between smoking and COVID-19 infection.
Literature Review
Our review came following the (PRISMA) statement guidelines. [5]
Study eligibility
The included studies should be in English, a journal published article, and a human study describing COVID-19 patients. The excluded studies were non-English or animal studies.
Study identification
Basic searching was done over the PubMed, Cochrane library, and Google scholar using the following keywords: Smoking, severity COVID-19, mortality.
Data extraction and synthesis
RCTs, clinical trials, and comparative studies, which studied the outcome of the Smokers group versus the Non-Smokers group of COVID-19 patients, will be reviewed.
Outcome measures included the prevalence of severe cases (as a primary outcome), and mortality rate (as a secondary outcome).
Study selection
We found 100 records, 36 excluded based on title and abstract review; 64 articles are searched for eligibility by full-text review; 24 articles cannot be accessed; 17 studies were reviews and case reports; 12 were not describing functional outcome; leaving 11 studies that met all inclusion criteria.
Statistical methodology
The pooling of data, Proportions (%), Odds Ratios (ORs), with 95% confidence intervals (CI) were done, using MedCalc ver. 18.11.3 (MedCalc, Belgium). According to heterogeneity across trials using the I2-statistics; a fixed-effects model or randomeffects model were used in the meta-analysis process.
Results
The included studies were published in 2020. Regarding the type of included studies, all studies were retrospective [Table 1].
Table 1: Patients and study characteristics.
| N | Author | Type of study | Number of patients | Age (average years) | Male patients | ||
|---|---|---|---|---|---|---|---|
| Total | Smokers group | Non-Smokers group | |||||
| 1 | L. Chen et al. [6] | Retrospective | 1859 | 111 | 1748 | 59 | 934 |
| 2 | M. Chen et al. [7] | Retrospective | 123 | 17 | 106 | 62.5 | 61 |
| 3 | Fu et al. [8] | Retrospective | 170 | 89 | 81 | -- | 99 |
| 4 | Guan et al. [9] | Retrospective | 1099 | 137 | 962 | 46.7 | 459 |
| 5 | Li et al. [10] | Retrospective | 102 | 7 | 95 | 62 | 59 |
| 6 | Liu et al. [11] | Retrospective | 78 | 5 | 73 | 42.7 | 39 |
| 7 | Parra-Bracamonte et al. [12] | Retrospective | 142690 | 11557 | 131133 | 50 | 79280 |
| 8 | Yang et al. [13] | Retrospective | 52 | 2 | 50 | 59.7 | 35 |
| 9 | Zhang, Cao, et al. [14] | Retrospective | 289 | 28 | 261 | 57 | 154 |
| 10 | Zhang, Dong, et al. [15] | Retrospective | 140 | 9 | 131 | 56.3 | 71 |
| 11 | Zhou et al. [16] | Retrospective | 191 | 11 | 180 | 56.3 | 119 |
#Studies arranged alphabetically.
Regarding patients’ characteristics, the total number of patients in all the included studies was 146793 patients, 11973 in the Smokers group, and 134820 in the Non-Smokers group [Table 1].
The mean age of all patients was (55.2 years), with 81310 (55.4%) male patients [Table 1].
A meta-analysis study was done on 11 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=146793) [Table 2].
Table 2: Summary of outcome measures in all studies.
| N | Author | Primary outcome | Secondary outcome | ||
|---|---|---|---|---|---|
| Severe COVID-19 cases | Mortality rate | ||||
| Smokers group | Non-Smokers group | Smokers group | Non-Smokers group | ||
| 1 | L. Chen et al. [6] | -- | -- | 25 | 183 |
| 2 | M. Chen et al. [7] | -- | -- | 7 | 24 |
| 3 | Fu et al. [8] | -- | -- | 16 | 18 |
| 4 | Guan et al. [9] | 17 | 50 | -- | -- |
| 5 | Li et al. [10] | -- | -- | 1 | 14 |
| 6 | Liu et al. [11] | 3 | 8 | -- | -- |
| 7 | Parra-Bracamonte et al. [12] | -- | -- | 1506 | 15366 |
| 8 | Yang et al. [13] | 0 | 32 | -- | -- |
| 9 | Zhang, Cao, et al. [14] | 8 | 70 | 12 | 37 |
| 10 | Zhang, Dong, et al. [15] | 6 | 52 | -- | -- |
| 11 | Zhou et al. [16] | 5 | 49 | 5 | 49 |
Each outcome was measured by:
Odds Ratio (OR):
• For COVID-19 severity and smoking.
• For mortality and smoking.
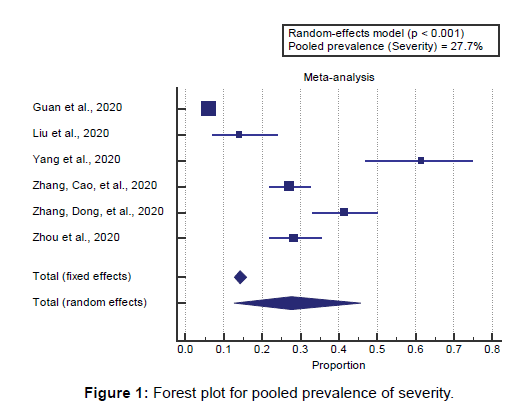
Concerning the primary outcome measure, We found 6 studies reported COVID-19 severity with a total number of patients (N=1849). I2 (inconsistency) was 98% with a highly significant Q test for heterogeneity (p<0.0001), so the random-effects model was carried out. Using the random-effects model, the pooled prevalence of severity among COVID-19 patients was (27.7%) [Figure 1].
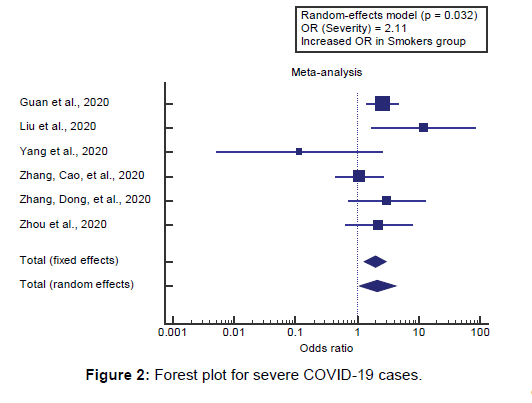
Using the random-effects model, the meta-analysis process revealed a significant increase in COVID-19 severe cases in the Smokers group compared to the Non-Smokers group (OR=2.11, P=0.032) [Figure 2].
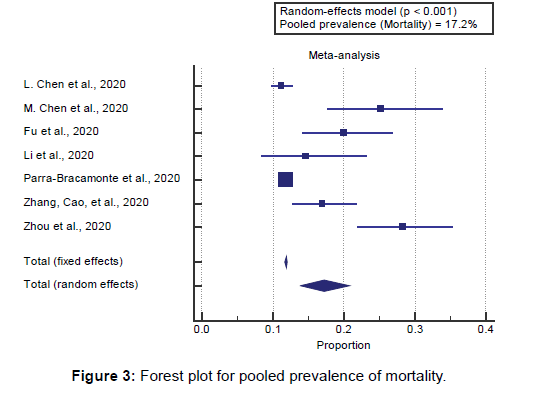
Concerning the secondary outcome measures, we found 7 studies reported mortality rates with a total number of patients (N=145424). I2 (inconsistency) was 91% with a highly significant Q test for heterogeneity (p<0.0001), so the randomeffects model was carried out. Using the random-effects model, the pooled mortality rate among COVID-19 patients was (17.2%) [Figure 3].
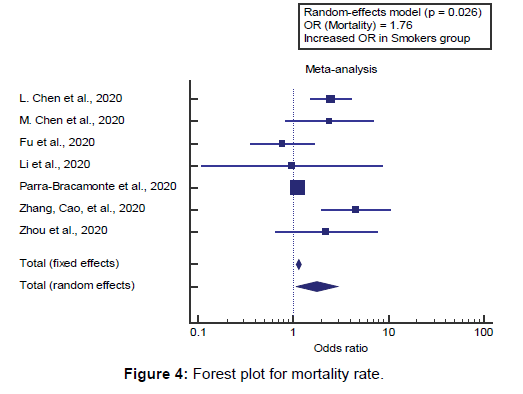
Using the random-effects model, the meta-analysis process revealed a significant increase in mortality in the Smokers group compared to the Non-Smokers group (OR=1.76, P=0.026) [Figure 4]. [6-16]
Discussion
This work aims to determine the link between smoking and COVID-19 infection. Regarding patients’ characteristics, the total number of patients in all the included studies was 146793 patients, 11973 in the smokers group, and 134820 in the nonsmokers group. The mean age of all patients was (55.2 years), with 81310 (55.4%) male patients. The included studies were published in 2020. Regarding the type of included studies, all studies were retrospective.
A meta-analysis study was done on 11 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=146793) concerning the primary outcome measure, we found 6 studies reported COVID-19 severity with a total number of patients (N=1849).
Using the random-effects model, the pooled prevalence of severity among COVID-19 patients was (27.7%).
Using the random-effects model, the meta-analysis process revealed a significant increase in COVID-19 severe cases in the Smokers group compared to the Non-Smokers group (OR=2.11, P=0.032), which came in agreement with Karanasos et al., [17] Reddy et al., [18] Zhao et al., [1] Jordan et al., [2] Cai, [19] Berlin et al., [20] Gallus et al., [21] and Farsalinos et al. [22]
Karanasos et al., reported that in research with low (<15%) incidence of diabetes, smoking increased the threat for severe disease (OR 1.66, I2=34%), findings have been 1) that smoking modestly will increase the hazard of severe disease in hospitalized COVID-19 patients at the same time as mortality data display a similar effect size but are currently inconclusive due to a low sample length, and 2) that this increased hazard for disease severity is extra prominent in younger patients without diabetes. [17]
Reddy et al., reported that they analyzed 47 eligible research reporting on 32,849 hospitalized COVID-19 patients, with 8417 (25.6%) reporting a smoking history, comprising 1501 current smokers, 5676 former smokers, and 1240 unspecified smokers. current people who smoke had an increased hazard of severe COVID-19 (RR 1.80, p=0.012), and severe or critical COVID-19 (1.98, 1.16-3.38; p=0.012). patients with a smoking history had a significantly extended risk of severe COVID-19 (p=0•001), severe or critical COVID-19 (p<0•0001). [18]
Zhao et al., reported that seven researches suggested the relationship between active smoking and the severity of COVID-19. The exact duration of smoking was no longer reported in maximum research. The pooled OR indicates that smoking will increase the threat of severe COVID-19 (fixedeffects model; OR=1.98) with the aid of round two folds. The heterogeneity among the different studies become moderate (I2=44%; P=0.10). [1]
Jordan et al., reported that obesity and smoking were associated with increased risks. In Italy, higher risks have also been reported in men than in women, which could be partly due to their higher smoking rates and subsequent comorbidities. [2] Cai, reported that research at the biology of viral infection and clinical control of the disease has additionally been published, some of which have demonstrated that differences in COVID-19 disease incidence and severity are related to sex, and smoking is related to higher expression of ACE2 (the receptor for severe acute respiratory syndrome coronavirus 2 [SARSCoV- 2]), so that might also be a factor. [19]
Berlin et al., reported that tobacco smoke exposure effects in inflammatory processes in the lung, increased mucosal inflammation, expression of inflammatory cytokines, and tumor necrosis thing α ([TNF]-α), increased permeability in epithelial cells, mucus overproduction, and impaired mucociliary clearance. Knowledge approximately host factors, and especially avoidable host factors which include smoking, may be of significance in lowering viral contamination and the severity of the disease. [20]
Gallus et al., reported that the latest systematic review, published in pre-print on 23 May also 2020, clarified the role of smoking in COVID-19 severity and mortality, summarizing the main findings so far. It examined 22 studies reporting disease severity in hospitalized patients according to smoking popularity. The meta-analysis covered only three fair-high-quality studies. Current people who smoke had been at higher hazard of more severe disorder than never smokers (RR: 1.37). [21]
Farsalinos et al., reported that, amongst 6515 patients, 440 of whom were current smokers, the pooled prevalence of modern smoking become 6.8% and the POR was 0.21 (P<0.001). In Chinese language research handiest, the POR was 0.20 (P<0.001). Modern-day smokers were more likely to have an adverse final result in comparison to non-current people who smoke (OR 1.53, P=0.022). However, they were much less likely to have an adverse outcome as compared to former smokers (OR: 0.42, P=0.003). [22] Our result came in disagreement with Lippi & Henry. [23]
Lippi & Henry reported that standard, in only one study active smoking was found to be a significant predictor of COVID-19 severity, while in the other 4 research the association was not statistically significant. Despite a trend in the direction of higher threat was considerable, no significant association could neither be discovered between lively smoking and severity of COVID-19 when data of individual research were pooled (OR, 1.69; p=0.254). No significant association can also be determined (89.5% of all sample size) was excluded from statistical analysis (OR, 4.35; p=0.129; I2, 29%, p=0.24). In conclusion, the results of this initial meta-analysis based on Chinese language patients suggest that lively smoking does not seem to be significantly associated with an enhanced chance of progressing towards severe disease in COVID-19. [23]
Concerning the secondary outcome measures, we found 7 studies reported mortality rates with a total number of patients (N=145424).
Using the random-effects model, the pooled mortality rate among COVID-19 patients was (17.2%).
Using the random-effects model, the meta-analysis process revealed a significant increase in mortality in Smokers group compared to Non- Smokers group (OR=1.76, P=0.026), which came in agreement with Alqahtani et al., [24] Organization, [4]
Grundy et al., [3] and Reddy et al. [18] Alqahtani et al., reported that, current smokers. [24]
The organization, reported that, at the time of this review, the available evidence suggests that smoking is associated with increased severity of disease and death in hospitalized COVID-19 patients. Although smoking exposure which includes (current and ex-smokers) was pronounced in 8 studies, with 221 confirmed COVID-19 cases. We assessed the prevalence of current smokers in all studies the usage of meta-evaluation of proportions of current smokers that had shown COVID-19. There was a pooled prevalence of 9%. The overall I2 was 92.49%, p zero.00. Indeed, 22.30% (31/139) of current smokers and 46% (13/28) of ex-smokers had excessive complications. Calculating the RR from these researches confirmed that current smokers (31/108) had been 1.45 times much more likely [RR=1.45] to have excessive complications as compared to former and never people who smoke (147/808) patients. A higher mortality price of 38.5% (5/13) become also been seen among likely related to severity, there is no evidence to quantify the risk to smokers of hospitalization with COVID-19 or of infection by SARS-CoV-2 was found in the peer-reviewed literature. [4]
Grundy et al., reported that eight researches had been recognized. One considered the relationship between smoking and the possibility of SARS-CoV-2 contamination, 3 considered the association between COVID-19 hospitalization and smoking history, and six reviewed the association between smoking history and the development of severe COVID-19. One looks at specifically investigated the risk of mortality. The studies considering the chance of severe disorder indicate that there is a massive association between COVID-19 and current or ever smoking. [3]
Reddy et al., 2020 reported that patients with a smoking history had a significantly increased risk of severe COVID-19 ( p=0.001), severe or critical COVID-19 ( p<0.0001), in-hospital mortality ( p<0•0001), disease progression (p=0.035), and need for mechanical ventilation ( p=0.043) [18]. Our result came in disagreement with Karanasos et al. [17]
Karanasos et al., reported that, for mortality, 5 studies with 838 patients were included. Smoking was not significantly associated with increased mortality (OR 1.45, 95%CI 0.78-2.72, I2=18%). Results were similar for studies explicitly reporting current smoking (2 studies-465 patients; OR 1.57, 95%CI 0.75- 2.31, I2=0%) [17].
Conclusion
To conclude, Patients with any smoking history are vulnerable to severe COVID-19 and worse in-hospital outcomes. In the absence of current targeted therapies, preventative and supportive strategies to reduce morbidity and mortality in current and former smokers are crucial.
Competing Interests
The authors declare that they have no competing interests. All the listed authors contributed significantly to the conception and design of study, acquisition, analysis, and interpretation of data and drafting of the manuscript, to justify authorship.
REFERENCES
- Zhao Q, Meng M, Kumar R, Wu Y, Huang J, Lian N, et al. The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis. J Med Virol. 2020.
- Jordan RE, Adab P, Cheng KK. COVID-19: Risk factors for severe disease and death. BMJ. 2020.
- Grundy EJ, Suddek T, Filippidis FT, Majeed A, Coronini-Cronberg S. Smoking, SARS-CoV-2 and COVID-19: A review of reviews considering implications for public health policy and practice. Tob Induc Dis. 2020;18.
- Organization WH. Smoking and COVID-19: A scientific brief, 26 May 2020. World Health Organization; 2020.
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. BMJ 2009;339.
- Chen L, Yu J, He W, Chen L, Yuan G, Dong F, et al. Risk factors for death in 1859 subjects with COVID-19. Leukemia 2020;34:2173-2183.
- Chen M, Fan Y, Wu X. Clinical Characteristics And Risk Factors For Fatal Outcome in Patients With 2019-Coronavirus Infected Disease (COVID-19) in Wuhan, China (2/27/2020). Publisher Full Text 2020.
- Fu L, Fei J, Xiang HX, Xiang Y, Tan ZX, Li MD, et al. Influence factors of death risk among COVID-19 patients in Wuhan, China: A hospital-based case-cohort study. MedRxiv 2020.
- Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708-1720.
- Li K, Chen D, Chen S. Radiographic findings and other predictors in adults with COVID-19. medRxiv; 2. Epub Ahead of Print 2020;27.
- Liu W, Tao Z-W, Wang L, Yuan M-L, Liu K, Zhou L, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J. 2020.
- Parra-Bracamonte GM, Lopez-Villalobos N, Parra-Bracamonte FE. Clinical characteristics and risk factors for mortality of patients with COVID-19 in a large dataset from Mexico. Ann Epidemiol. 2020.
- Yang X, Yu Y, Xu J, Shu H, Liu H, Wu Y, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020.
- Zhang J, Cao Y, Tan G, Dong X, Wang B, Lin J, et al. Clinical, radiological and laboratory characteristics and risk factors for severity and mortality of 289 hospitalized COVID-19 patients. Allergy 2020.
- Zhang J, Dong X, Cao Y, Yuan Y, Yang Y, Yan Y, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 2020.
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. The Lancet 2020.
- Karanasos A, Aznaouridis K, Latsios G, Synetos A, Plitaria S, Tousoulis D, et al. Impact of smoking status on disease severity and mortality of hospitalized patients with COVID-19 infection: A systematic review and meta-analysis. Nicotine Tob Res. 2020.
- Reddy RK, Charles WN, Sklavounos A, Dutt A, Seed PT, Khajuria A. The effect of smoking on COVID-19 severity: A systematic review and meta-analysis. Journal of Medical Virology 2020.
- Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir Med. 2020;8:e20.
- Berlin I, Thomas D, Le Faou AL, Cornuz J. COVID-19 and smoking. Nicotine Tob Res. 2020.
- Gallus S, Lugo A, Gorini G. No double-edged sword and no doubt about the relation between smoking and COVID-19 severity. Eur J Intern Med. 2020;77:33-35.
- Farsalinos K, Poulas K, Polosa R, Barbouni A, Caponnetto P, Niaura R. Prevalence of current smoking and association with adverse outcome in hospitalized COVID-19 patients: A systematic review and meta-analysis 2020.
- Lippi G, Henry BM. Chronic obstructive pulmonary disease is associated with severe coronavirus disease 2019 (COVID-19). Respir Med. 2020;167:105941.
- Alqahtani JS, Oyelade T, Aldhahir AM, Alghamdi SM, Almehmadi M, Alqahtani AS, et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: A rapid systematic review and meta-analysis. PloS One 2020;15:e0233147.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.