Smoking Prevalence and Attitudes Regarding its Control Among Health Professional Students in South‑Western Nigeria
- *Corresponding Author:
- Dr. Olayemi F Awopeju
Department of Medicine, Obafemi Awolowo University, Ile-Ife, Osun State, Nigeria.
E-mail: yemijide@yahoo.com
Abstract
Background: Tobacco use is one of the leading preventable causes of morbidity and mortality globally; about 70% of smokers see physicians each year. Health care professionals have a very unique role in motivating people to quit smoking. Aim: The aims of this study were to document the smoking prevalence and attitudes regarding its control among these set of students who will be tomorrow’s health care providers. Subjects and Methods: A cross‑sectional survey was conducted in two medical schools in South‑Western Nigeria with their accompanied nursing and pharmacy students. All students in the selected schools were eligible to participate and student’s participation was voluntary. The Global Health Professional Students Survey core questionnaire was used to collect data on smoking prevalence and attitudes regarding its control. The data were summarized using percentages and confidence interval (CI) was calculated using standard error of mean. Pearson’s Chi‑square and fisher’s exact were employed to test the significance. Results: Life‑time prevalence of cigarette smoking was 17.9% (121/675) with (95% confidence interval [CI] 15‑20.8). Only 5.04% (34/675) with (95% CI 3.7‑7.1) of the respondents were currently smoking. Ever smokers were significantly less likely than non‑smokers to indicate that tobacco sales to adolescents should be banned (P < 0.01). Fewer smokers than non‑smokers agreed that there should be a complete ban on advertising of tobacco products (P < 0.001). 93.3% of them said that they were taught about danger of smoking but only 48.6% ever heard of using anti‑depressant in tobacco cessation program. Conclusions: Smoking prevalence among health professional students in South‑West Nigeria is relatively low; however, majority believed that health‑care providers serve as role models for their patients and the public.
Keywords
Prevalence, Health- professional students, Smoking, South-western Nigeria
Introduction
Tobacco use is one of the leading preventable causes of premature deaths, diseases, and disabilities around the world.[1] Between 1950 and 2000, approximately 70 million people have died from tobacco use and over the next 50 years another 450 million might die due to smoking related diseases.[2-4] Tobacco use is said to be rising faster in Africa than in any other continent,[5] Nigeria not being an exception. The prevalence of smoking in general population is reported to be 8.9% in Nigeria,[6] however, the distribution of smoking is not the same across all the strata of the society. It varies from 7.7% among female secondary schools;[7] 17.1% among secondary school students;[8] 17.7% among physicians;[9] 20.3% among soldiers[10] to 37.9% among the general population in northern part of the country.[11]
Health-care professionals represent an important part of the population as they are care providers, who are regarded as having a high degree of reliability in health-related matters by the general public and are advantageously placed to advance the anti-smoking message. Smokers employed in hospital settings set a poor example of health-promoting behaviors and have the potential to unintentionally affect the smoking behaviors of others through modeling.[12,13]
It is estimated that about 70% of smokers see physicians, each year with substantial opportunity to influence smoking behavior.[14] Medical advice to quit produces 1 year abstinence rates of up to 5-10%, which would have a significant public health impact if it were provided.[15] However, many barriers are responsible for the reduction of the effectiveness or willingness of health professionals to provide patient counseling, some of which are; time constraints during the consultation,[16] and the smoking status of the health professional themselves.[17] Smoking health professionals may impede their ability to help patients quit smoking.
Although, a study was done recently on tobacco use among health professional students globally only Ghana was included in the survey in sub-Saharan African,[18] and most studies done in Nigeria are old and there are few recent studies. This study will address this gap in knowledge and may also provide a basis for intensifying curriculum change in health professional institutions.
We, therefore, conducted this study to determine the smoking prevalence, attitudes and training among medical, dental, nursing, and pharmacy students in two universities in South-Western Nigeria.
Subjects and Methods
The two universities in South-Western Nigeria that have every group of the health-care professional students were chosen purposefully to participate in the cross-sectional survey. The two schools are Obafemi Awolowo University, Ile Ife and University of Lagos, Lagos;
The sample size for the study was calculated using the formula:[19]
Where n is the required sample size, t is the confidence level at 95% (standard value of 1.96), P is the estimated prevalence of smoking in the schools, this is estimated as 50%, as it is not exactly known, and m is the margin of error at 5% (standard value of 0.05). This give 384 students, because the sampling method was not simple random technique this was multiplied by 2.[20] Another 8% was added to allow for non-responders, this totaled 830.
All the students were eligible to participate and students’ participation was voluntary. At each school, the students were briefed about the purpose of the research. Assurance was given about anonymity and confidentiality of the information to be provided. Verbal and written consents were taken for the students. We used the Global Health Professional Students Survey (GHPSS) questionnaire developed by the Tobacco Free Initiative, a project of the World Health Organization, in collaboration with the Centers for Disease Control and a number of additional partners.
This standardized survey instrument aims to monitor and document the prevalence of tobacco use among health professionals and assess their knowledge, attitudes and behaviors towards tobacco and tobacco control policies. This semi-structured questionnaire is divided into six aspects to assess: Tobacco use prevalence among health professional students, exposure to environmental tobacco smoke, attitudes, behavior/cessation, curriculum/training, and demographics, the questionnaire was not modified as English is the official language of the country. The questionnaires were distributed just as normal lectures in their respective classrooms. An “ever smoker” was defined as one who had ever smoked during life-time, even if had tried a few puffs, once or twice. A “current smoker” was defined as one who had smoked during 30 days prior to the survey including the ones who smoked every-day.
We used SPSS (Statistical Package for Social Sciences) version 16.0 (Chicago IL. USA) for statistical analysis. We checked for any inconsistencies in the data entry. If inconsistencies were found, we verified them with the completed questionnaires. The data were summarized using percentages and confidence interval (CI) was calculated using standard error of mean. Pearson’s Chi-square and fisher’s exact were employed to test the significance between ever smokers and non-smokers. Permission was obtained to carry out the survey from each school.
Results
Demographics
Of 830 sampled, 675 returned the questionnaires giving a response rate of 81.3%. There are 343 students from Ile-Ife and 332 from Lagos. The distribution by course is as follows 228 (33.8%) were medical students, 50 (7.4%) were dental students, 216 (32.0%) were nursing students and 181 (26.8%) were pharmacy students. Female constitute 51.1% (345/675) and most 404/660 are in age group 19-24 years and other demographics of the respondents are shown in Table 1.
| Data | Frequencies | Percentages | |
|---|---|---|---|
| Age group | |||
| <18 years | 40 | 6.1 | |
| 19-24 years | 404 | 61.2 | |
| 25-29 years | 190 | 28.8 | |
| >30 years | 26 | 3.9 | |
| Gender | |||
| Male | 330 | 48.9 | |
| Female | 345 | 51.1 | |
| Course year in school | |||
| 3rd year | 311 | 46.1 | |
| 4th | year | 92 | 13.6 |
| 5th | year | 105 | 15.6 |
| 6th | year | 167 | 24.7 |
| Course of study | |||
| Medical students | 228 | 33.8 | |
| Dental student | 50 | 7.4 | |
| Nursing students | 216 | 32.0 | |
| Pharmacy students | 181 | 26.8 | |
Table 1: Socio-demographic characteristics of the respondents
Prevalence
Life-time prevalence of ever smoking cigarette among all respondents was 121/675; 17.9% with 95% CI (15-20.8), with prevalence of 11.9% (42/345) among females compared with 23.9% (79/330) among males however only 5.04% (34/675), 95% CI (3.7-7.1) of all respondents had currently smoked in the last 30 days. The prevalence of smoking among male and female is 3.4% (23/330) and 1.6% (11/345) respectively in the last 30 days [Table 2].
| Ever smokedcigarette(n=121) % | Smoked in thelast 30 days(n=34) % | |
|---|---|---|
| Sex | ||
| Male | 11.4 | 3.4 |
| Female | 6.5 | 1.6 |
| Total | 17.9 | 5.0 |
| Students course | ||
| Medical students | 6.4 | 1.5 |
| Dental students | 1.6 | 0.3 |
| Nursing students | 3.8 | 0.8 |
| Pharmacy students | 6.1 | 2.4 |
| Total | 17.9 | 5.0 |
Table 2: Prevalence of smoking according to sex and students course
Out of the people that ever smoked, 34.7% (42/121) were females and 65.3% (79/121) were males. Twenty nine percent of them (196/675) initiated smoking before the age of 10 years and 22.6% (153/675) initiated smoking between 11 years and 15 years of age.
Attitude
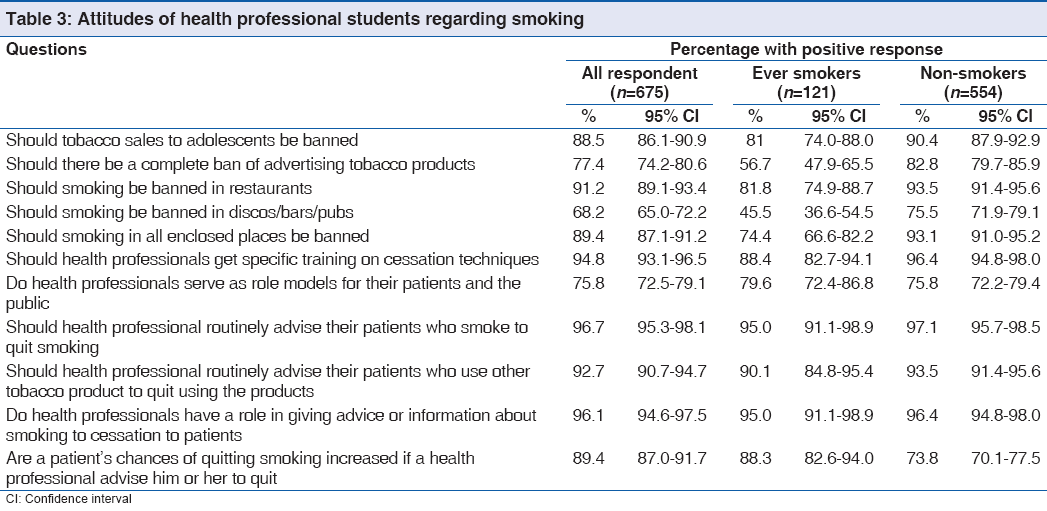
Majority of the health professional students 88.5%; (599/675) 95% CI 86.1-90.9 agreed that tobacco sales to adolescents should be banned, also 91.2% (617/675) 95% CI 89.1-93.4 accepted that smoking should be banned in restaurants and 89.4% (606/675); 95% CI 87.1-91.2 of the students agreed that smoking in all enclosed places be banned, while only 68.8% (486/675); 95% CI 65.0-72.2 believed that smoking should be banned in disco/bars/pubs and 77.4% (522/675); 95% CI 74.2-80.6 agreed that there should be a complete ban.
There were clear differences between smokers and non-smokers in their attitudes to smoking issues. Ever smokers (81%: 98/121) were significantly less likely than non-smokers (90.4%: 501/554) to indicate that tobacco sales to adolescents should be banned (P = <0.01). Fewer smokers (56.7%: 68/121) than non-smokers (82.8%: 458/554) agreed that there should be a complete ban on advertising of tobacco product (P < 0.001). Regarding the question, should smoking be banned in disco/pubs/ bars, a reduced number of ever smokers (45.5%: 55/121) answered in affirmative compare to non-smokers (75.5%: 413/554), this is highly significant (P < 0.001).
Generally, there was clear majority support for the statements: Should health professional routinely advise their patients who smoke to quit smoking, should health professional routinely advise their patients who use other tobacco product to quit using the products, do health professionals have a role in giving advice or information about smoking to cessation to patients, however only three quarters believed that health professionals serve as role models [Table 3] with comparable results between smokers (79.6%: 93/121) and non-smokers (75.8%: 420/554).
Training
Concerning training 93.3% (629/675); 95% CI (91.4-95.2) were taught about danger of smoking, 93.6% (632/675); 95% CI (91.7-95.4) learned that it is important to record tobacco use history as part of a patient’s general medical history. Seventy-two percent (485/675) of the respondents reported they had ever received any formal training in smoking cessation, however, 48.6% (328/675); 95% CI (44.8-52.5) ever heard of using anti-depressant in tobacco cessation program.
Discussion
The smoking rate among health professional students in this survey was lower than reported when compared to other parts of the globe’s previous studies, using the same questionnaire, findings from GHPSS showed that over 20% of students currently smoked cigarettes in 47 of 80 sites surveyed, although, the prevalence ranges from 1.3% in Ghana among medical students to as high as 47% in Bosnia and Herzegovina federation.[18] The findings in Africa are generally lower than their counterpart in Europe and in the Middle Eastern countries.
In Africa, the smoking prevalence varies from region to region, rate being the highest in North African countries when compared to other parts of Africans, the GHPSS study result showed the following prevalence of current smoker among medical students: Tunisia 11.1%; Egypt 7.9%; Uganda 2.8% and Ghana I.3%. This might be due to the difference in socio-economic factors and influence of westernization, more so, in North Africa smoking is culturally acceptable.
The smoking rate among health-professional students is low compared to general population in Nigeria and other category of people that have been studied, Fawibe and Shittu[21] reported that the prevalence of smoking among medical students is significantly low compared to other non-medical students 0.9% compared to 6.4% this may be due to a number of factors Firstly, they may recognize the negative medical consequences more quickly than the general public. Secondly, their devotion to health naturally conflicts with unhealthy behaviors. Thirdly, tobacco smoking usually incurs a negative image in the health-care profession long before it does so in the wider community.
Of importance in this study is that one-third of all the ever smokers are females; Previous investigation conducted among physicians showed females smoked less compared to their male[21,22] counterparts while other research revealed no female smokers[23-25] however, other study found a comparable rate between male and female physicians.[26,27] In fact a study[28] reveal that more female smoked compared to the males. In a study conducted exclusively among female secondary school students, a prevalence 7.7% was reported in South-Eastern Nigeria.[7] Generally, there is an increasing prevalence of smoking among females health professionals which might be attributable to improvement in women’s social factor such as education, employment, and urbanization.
Majority of the ever smokers initiated smoking before 15-year of age and this is in consonance with other studies, this is corroborated by Ibeh study[7] and Fawibe and Shittu[21] study with mean age of smoking 12.6 years and 15.4 years respectively. Adolescent first cigarette is usually obtained from friends and family members and smoking can be viewed as rite of passage from childhood to adulthood.[29] However, a quarter of them also started smoking between 20 years and 24 years of age, which may be related to peer pressure in the university.
The attitudes of these students are essential as it is going to affect how seriously they are likely to adopt smoking cessation program and patients’ counseling. Only three-fourth of the students believed that smoking should be completely banned. This is similar to 63% reported by Awotedu[30] among tertiary institutions in South Africa and also as might be expected, these clear difference between smokers and non-smokers attitudes with regards to banning and advertising of tobacco in public places, this in consonance with other studies.[12,31,32] Smoking by health-care professional may actually hamper their capacity to render smoking cessation counseling to their patients, more so three-quarters of them believed that health professional serve as models.
Majority of them reported that they were taught about the dangers of smoking and that it is important to record tobacco use history, this is off-set by the fact that only about 50% have ever heard of using anti-depressant, although, about 70% of them claimed they had formal training in smoking cessation approaches. The percentage of students who claimed they had formal training is rather high compared to the study of Warren,[18] where less than 40% of the students in 73 of 80 sites reported that they have received such training but when school administrators were asked, 25 out of 31 countries had no formal training at any time. This difference might be due to the fact that students in our study were over reporting, probably to please the faculty. Even, in a study conducted among practicing physicians, only 30% had knowledge of smoking cessation therapy and 70% reported that tobacco education content in the medical school curriculum was inadequate.[9] This underscores the importance of training of professional health students in courses that detailed the harmful health effect of tobacco use and exposure to second smoke and specific training in counseling on tobacco cessation techniques.
Although, our study has demonstrated smoking habits, attitudes, and training among tomorrow’s health care professionals, this should be interpreted in the light of some limitations. First, this study reports behavior rather than the behavior itself, which might be influenced by recall or by perception of social desirability and may under-estimate smoking compared to cotinine measurement[33] and over-estimate smoking attitude and behavior. Secondly, our results may not be applicable to all health professional students in Nigeria as we only sampled cluster of students in south-western region. Thirdly, although, participation is voluntary, we still cannot rule out some selection bias. Nevertheless, our study would serve as bench mark for further studies in other regions of Nigeria.
In conclusion, this study revealed that smoking rate is relatively low among our health professional students, compared to other developing world; it identified the need for attitudinal change in this set of students who should consider themselves pivotal to global tobacco control. It also highlighted the need for a detailed professional training to include, dangers of smoking, counseling on smoking cessation, act of legislation, and tobacco tax policy. Ensuring smoking cessation best practice into health professional students’ curriculum will not only alter their attitudes but it may also prevent new physician smokers.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Comparative risk assessment collaborating group. Selected major risk factors and global and regional burden of disease. Lancet 2002;360:1347-60.
- International Union Against Tuberculosis and Lung Diseases. Paris: The Union. 10 Facts on tobacco use. 2009. Available from: http://www.theunion.org/download/factsheets/ facts_tobacco.pdf. [Last accessed 15 May 2011].
- U.S. Dept. of health and human services; Public Health Service; Centers for Disease Control; Center for Health Promotion and Education; Office on smoking and health. The health consequences of smoking: Nicotine addiction: A report of the Surgeon General. DHHS publication, no. (CDC) 88-8406. Rockville: U. S. Dept. of Health and Human Services; 1988. p. 30.
- Centers for Disease Control and Prevention (CDC). Cigarette smoking among adults: United States, 2000. MMWR Morb Mortal Wkly Rep 2002;51:642-5.
- Aït-Khaled N, Enarson D, Bousquet J. Chronic respiratory diseases in developing countries: The burden and strategies for prevention and management. Bull World Health Organ 2001;79:971-9.
- Shafey O, Dolwick S, Guindon GE. Tobacco control country profiles. 2nd ed. Atlanta GA: American Cancer Society, Inc., World Health Organization and International Union against Cancer; 2003. p. 38-40.
- Ibeh CC, Ele PU. Prevalence of cigarette smoking in young Nigerian females. Afr J Med Med Sci 2003;32:335-8.
- Odeyemi KA, Osibogun A, Akinsete AO, Sadiq L. The Prevalence and predictors of cigarette smoking among secondary school Students in Nigeria. Niger Postgrad Med J 2009;16:40-5.
- Desalu OO, Adekoya AO, Elegbede AO, Dosunmu A, Kolawole TF, Nwogu KC. Knowledge of and practices related to smoking cessation among physicians in Nigeria. J Bras Pneumol 2009;35:1198-203.
- Hussain NA, Akande M, Adebayo ET. Prevalence of cigarette smoking and knowledge implications among Nigerian soldiers of its health. East Afr J Public Health 2010;7:81-3.
- Desalu OO, Olokoba A, Danburam A, Salawu F, Issa B. Epidemiology of tobacco smoking among adults population in North-East Nigeria. Internet J Epidemiology 2008;6:1. Available from: http://www.Ispub.com. [Last accessed 17 May 2011].
- Olive KE, Ballard JA. Attitudes of patients toward smoking by health professionals. Public Health Rep 1992;107:335-9.
- Bandura A. Social foundation of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
- A clinical practice guideline for treating tobacco use and dependence: A US public health service report. The tobacco use and dependence clinical practice guideline panel, staff, and consortium representatives. JAMA 2000;283:3244-54.
- Lancaster T, Stead L, Silagy C, Sowden A. Effectiveness of interventions to help people stop smoking: Findings from the Cochrane Library. BMJ 2000;321:355-8.
- Pollak KI, Arredondo EM, Yarnall KS, Lipkus I, Myers E, McNeilly M, et al. How do residents prioritize smoking cessation for young “high-risk” women? Factors associated with addressing smoking cessation. Prev Med 2001;33:292-9.
- Jenkins K, Ahijevych K. Nursing students’ beliefs about smoking, their own smoking behaviors, and use of professional tobacco treatment intervention. Appl Nurs Res 2003;16:164-72.
- Warren CW, Jones NR, Chauvin J, Peruga A, GTSS Collaborative Group. Tobacco use and cessation counselling: Cross-country. Data from the Global Health Professions Student Survey (GHPSS), 2005-7. Tob Control 2008;17:238-47.
- Barlett JE, Kotrlik JW, Higgins C. Organization research: Determining appropriate sample size for survey research. Inf Technol Learn Perform J 2001;19:43-50.
- Neuman WL. Social Research Methods: Qualitative and Quantitative Approach. 2nd ed. Boston: Brill Academic Publishers; 2005. p. 235.
- Fawibe AE, Shittu AO. Prevalence and characteristics of cigarette smokers among undergraduates of the University of Ilorin, Nigeria. Niger J Clin Pract 2011;14:201-5.
- Josseran L, King G, Guilbert P, Davis J, Brücker G. Smoking by French general practitioners: Behaviour, attitudes and practice. Eur J Public Health 2005;15:33-8.
- Smith DR, Wei N, Zhang YJ, Wang RS. Tobacco smoking habits among a cross-section of rural physicians in China. Aust J Rural Health 2006;14:66-71.
- Yaacob I, Abdullah ZA. Smoking habits and attitudes among doctors in a Malaysian hospital. Southeast Asian J Trop Med Public Health 1993;24:28-31.
- Cheng KK, Lam TH. Smoking among young doctors in Hong Kong: A message to medical educators. Med Educ 1990;24:158-63.
- Samuels N. Smoking among hospital doctors in Israel and their attitudes regarding anti-smoking legislation. Public Health 1997;111:285-8.
- Scott HD, Tierney JT, Buechner JS, Waters WJ Jr. Smoking rates among Rhode Island physicians: Achieving a smoke-free society. Am J Prev Med 1992;8:86-90.
- Zanetti F, Gambi A, Bergamaschi A, Gentilini F, De Luca G, Monti C, et al. Smoking habits, exposure to passive smoking and attitudes to a non-smoking policy among hospital staff. Public Health 1998;112:57-62.
- Simons-Morton B, Chen R, Abroms L, Haynie DL. Latent growth curve analyses of peer and parent influences on smoking progression among early adolescents. Health Psychol 2004;23:612-21.
- Awotedu AA, Jordaan ER, Ndukwana OZ, Fipaza NO, Awotedu KO, Martinez J, et al. The smoking habits, attitudes towards smoking and knowledge regarding anti smoking legislation of students in institution of higher learning in Eastern Cape province of South Africa. SA Fam Pract 2006;48:14-8.
- Hughes AM, Rissel C. Smoking: Rates and attitudes among health services staff in central Sydney, Australia. Tob Control 1998;7:441.
- Jiang Y, Ong MK, Tong EK, Yang Y, Nan Y, Gan Q, et al. Chinese physicians and their smoking knowledge, attitudes, and practices. Am J Prev Med 2007;33:15-22.
- Pérez-Stable EJ, Benowitz NL, Marín G. Is serum cotinine a better measure of cigarette smoking than self-report? Prev Med 1995;24:171-9.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.