Socio-Demographic Determinants of Maternal Health-Care Service Utilization Among Rural Women in Anambra State, South East Nigeria
- *Corresponding Author:
- Dr. Onyeonoro UU
Department of Community Medicine, Abia State University, Aba Campus, Aba, Abia State, Nigeria.
E-mail: hugouche@yahoo.com
Abstract
Background: Although, antenatal care (ANC) attendance in sub Saharan Africa is high, however this does not always translate into quality ANC care service utilization. Aim: This study therefore is aimed at exploring pattern of maternal health (MH) services utilization and the socio‑demographic factors influencing it in Anambra State, South East Nigeria. Subjects and Methods: A total of 310 women of reproductive age with a previous history of gestation attending ANC services between September, 2007 and August, 2008 in selected Primary Health Centers in Anambra State were studied. Responses were elicited from the study participants using a pre-tested, semi-structured interviewer-administered questionnaire. Data collected were analyzed using Statistical Package for Social Sciences (SPSS) version 17 (SPSS Inc, Chicago Illinois, USA). Association between socio‑demographic characteristics and pattern of utilization of ANC and delivery services was measured using χ2‑test, Regression analysis was done to identify factors associated with utilization of MH services. P < 0.05 was assumed to be significant. Results: Use of health facility was 293 (97.0%) and 277 (92,7%) out 302 women for ANC and delivery services respectively . Most women attended their first ANC consultation during the preceding pregnancy was after the first trimester and about 31% (94/298) of them had <4 ANC visits prior to delivery. Socio‑demographic factors were found to be significantly associated with places where MH care services are accessed. Parity was found to be associated with timing of ANC booking and number of ANC attendance (χ2 = 9.49, P = 0.05). Odds of utilizing formal health facility for MH services were found to be significantly associated with increasing age (P < 0.01) and educational status of mothers (P < 0.001). Conclusions: The study revealed high maternal service utilization and 10% fetal loss, hence the need to address the gaps of late ANC booking and low ANC visits.
Keywords
Antenatal care, Delivery, Determinants, Nigeria, Parity, Rural
Introduction
Maternal and reproductive health services in health systems constitute a large range of curative and preventative health services of particular importance to the health of women of reproductive age. It also refers to population-based services such as behavior change and health communication. It includes a range of services provided to women of reproductive age prior to conception, during pregnancy, during and after delivery.[1] Its importance particularly in developing countries cannot be overemphasized. For instance, antenatal care (ANC) helps to ensure the well-being of the mother and fetus through early detection of risks in pregnancy, prevention of pregnancy and labor complications and ensures the safe delivery of mother and child. Furthermore, it exposes pregnant women to counseling and education about their own health and the care of their children. With the strong positive association that has been shown to exist between level of care obtained during pregnancy and the use of safe delivery care, ANC also stands to contribute indirectly to maternal mortality reduction.[2] However, vast majority of women in Sub-Saharan Africa do not have access to safe delivery care.[3]
However, pregnant woman enjoys these benefits when she attends ANC and delivers in appropriate health facility. In addition, pregnancy must be supervised by a trained health personnel and labor attended to by a skilled birth attendant.[4] Furthermore, the woman on her part is expected to book early and attend adequate number of ANC prior to delivery. Although ANC attendance has been measured based on the proportion of women who have attended ANC at least once during pregnancy; World Health Organization (WHO) in 2002 recommends that pregnant women should attend ANC at least 4 times starting from the first trimester.[5] In Nigeria, the current ANC schedule recommends that a pregnant should book for ANC during the first trimester, thereafter attend ANC clinic as follows; 4 weekly until 28 weeks gestation, 2 weekly until 36 weeks gestation and weekly until delivery. Evidence available suggests that most women who attend ANC in the country do not receive adequate attention and care providers are overwhelmed by the number of pregnant women seeking ante natal care. Consequently, some advocates have argued for the adoption of focused ANC care, in which case a woman attends ANC 4 times during pregnancy at specific intervals as recommended by WHO. This allows for adequate attention to be given to each pregnant woman while high-risk pregnancies are better monitored.[6]
To reduce the maternal morbidity, mortality and improve neonatal health, the Nigerian government in time past has focused on improving access and supply of maternal health (MH) services through the primary health-care strategy.[7] Despite these efforts, maternal morbidity and mortality remain a major public health problem in the country. Recently, the country rolled out the integrated maternal, newborn and child health (IMNCH) strategy as part of measures aimed at reducing maternal and infant mortality and the attainment of millennium development goals (MDGs) four and five. This was informed by the fact that significant progress has not been made toward reduction of maternal mortality and under-five deaths. Data from National Health and Demographic Survey revealed that Maternal Mortality ratio declined from 1100 deaths/100,000 live births in 1990-980 deaths/100,000 live births in 2000 and as at 2008 stood at 840 deaths/100,000 live births.[8] Since 1990, the country has only achieved a yearly reduction of under-five mortality of 1.2%, a trend if allowed to continue may lead to non-attainment of MDGs four and five.[9] A number factors have been associated with utilization of MH services, among which are socio-demographic factors – age, religion, maternal education, husband’s education, marital status, employment status and parity. Other factors that influence MH care service use include cost, availability of service, household income and access to health information exposure, previous history of obstetric complications, cultural beliefs and ideas about pregnancy.[2,9-12]
In South East Nigeria, there are variations in the utilization of MH services. Ante natal care attendance (99.7%) and facility delivery (97.0%) is high, but post-natal care service utilization (<10.0%) is low.[13,14] However, not many studies have examined pattern and adequacy of ANC care service utilization. Furthermore, fewer have looked at socio-demographic determinants of uptake of MH care services in the region. This study, therefore, explores the pattern of MH services utilization and the socio-demographic factors influencing it in Anambra State, South East Nigeria.
Subjects and Methods
The study was carried in three health centers in Anambra State under the management of Nnamdi Azikiwe University Teaching Hospital (NAUTH) and they are Primary Health Centre (PHC), Neni, Anaocha Local Government Area (LGA), Comprehensive Health Centre, Ukpo, Dunukofia LGA and PHC, Umunya, in Oyi LGA. The health center at Neni and Ukpo are supervised by the Department of Community Medicine and also serves as community outreach center for the Department of Family Medicine. These communities are predominantly rural and most common economic they are engaged in is farming and trading. All the health centers provide primary health-care services including maternal and child health services. Health services in all the facilities are provided by a team of doctors, pharmacists, nurses, community health extension workers, laboratory scientists and technicians. The study was conducted between September, 2007 and August, 2008. ANC and infant welfare clinic services are provided in the facilities weekly. Average ANC clinic attendance was 20-25 women per facility per week while average booking rate for new clients per month is 8-10. The entire women attending ANC within the period in these facilities and consented to participate in the survey within the period were selected until a total of 310 women were recruited. Primigravida were excluded from the survey.
Responses were elicited from the study participants using a pre-tested, pre-validated, semi-structured interviewer-administered questionnaire on socio-demographic characteristics – age, marital status, educational status and parity, pattern of ANC and natal service utilization and outcome of pregnancy during their most recent confinement. Parity was classified as follows – 1 = primiparous, 2-4 = multiparous and 5+ = grand multiparous. ANC service utilization was assessed based on the following – type of facility utilized for ANC care, timing of booking for ANC and number of ANC visits made during the last pregnancy. While utilization of natal services was assessed using, type of facility used during delivery, mode of delivery and outcome of pregnancy. Verbal consent was extracted from the women after due explanation of the procedure, risk and benefits of the survey. Ethical clearance was obtained from Nnamdi Azikiwe University Teaching Hospital, Nnewi Ethics Committee. Data collected were analyzed using the Statistical Package for Social Sciences (SPSS) version 17 (SPSS Inc, Chicago Illinois, USA). Frequency statistics was used to describe general characteristics and pattern of utilization of MH care of service among the mothers. Association between socio-demographic characteristics and pattern of utilization of ANC and natal care services was measured using χ2-test and level of statistical significance was assumed to be P = 0.05 and where the value of a cell is <5 Fischer’s exact (F) test was used. Following test of significance where P < 0.05. Multinomial logistic regression was used to estimate the of odds (Odds Ratio [OR]) of utilizing MH services by selected socio-demographic characteristics-age, parity, educational status and marital status found to statistically significantly associated with utilization of MH services, which were primarily place utilized for ANC and delivery services. Socio-demographic characteristics of the mothers were categorized and coded as follows: Age - 0= ≤24 years, 1 = 25-29 years and 2= ≥30 years; parity - 0 = primiparous, 1 = multiparous, 2 = grand multiparous; educational status - 0 = primary, 1 = secondary, 2 = tertiary and marital status 0 = married, 1 = others-single, widowed or divorced, with 0 as the dummy variable. Place of utilization of ANC and delivery services was compared between health center, hospital and others-none, home/traditional birth attendants (TBA)/maternity with others as the reference category.
Results
Out of a total of 310 women recruited for the survey, eight of them did not complete the interview. The survey showed that the median age of the women was 27 years. Out of 302, 2 96.0% (296/302) of them were Christians 68.0% (201/296) of them was Catholics. Also, 95% (287/302) was married, all of them had at least primary education and 64.6% (195/302) were multiparous as shown in Table 1.
| Socio-demographic characteristics | N=302 | Percentage |
|---|---|---|
| Age (in years) | ||
| ≤24 | 58 | 19.2 |
| 25-29 | 119 | 39.4 |
| 30+ | 125 | 41.4 |
| Marital status | ||
| Married | 287 | 95.0 |
| Single | 6 | 2.0 |
| Divorced/separated/widowed | 9 | 3.0 |
| Educational status | ||
| Primary | 29 | 9.6 |
| Secondary | 137 | 45.4 |
| Tertiary | 136 | 45.0 |
| Parity | ||
| Primiparous | 69 | 22.8 |
| Multiparous | 195 | 64.6 |
| Grand multiparous | 38 | 12.6 |
Table 1: Socio-demographic characteristics of mothers
During their last confinement, four women (1.3%) out of 302 did not attend ANC services. A total of 293 (97.0% out of 302 mothers) utilized the formal health facility for ANC servicTwo hundred and thirty eight (78.8%) of the 302 women utilized the hospital during the last ANC while five women (1.6%) out 302 utilized the services of TBA/maternity. Only19.1%(57/298) booked for ANC during the first trimester and 174 women (58.4%) out of 298 attended ANC at least 4 times.
Among 298 of them who attended ANC, 30 (10.1%) could not remember or did not know the number of times they attended ANC. Median ANC attendance among them was 4 times [Table 2].
| Pattern of maternal care utilization | N=302 | Percentage |
|---|---|---|
| Place of ANC attendance | ||
| Hospital | 238 | 78.8 |
| Health center | 55 | 18.2 |
| TBA/maternity | 5 | 1.6 |
| None | 4 | 1.3 |
| Timing of ANC booking | N=298 | |
| ≤3 months | 57 | 19.1 |
| 4-6 months | 165 | 55.4 |
| ≥7 months | 76 | 25.5 |
| Number ANC attendance | N=298 | |
| 1 | 32 | 10.7 |
| 2-3 | 62 | 20.8 |
| ≥4 | 174 | 58.4 |
| DNK/cannot remember | 30 | 10.1 |
| Place of delivery | N=302 | |
| Hospital | 238 | 78.8 |
| Health center | 42 | 13.9 |
| TBA/local midwife | 16 | 5.3 |
| Home | 6 | 2.0 |
| Mode of delivery | ||
| Spontaneous vaginal delivery | 274 | 90.7 |
| Assisted vaginal delivery | 14 | 4.6 |
| Cesarean section | 14 | 4.6 |
| Pregnancy outcome | ||
| Abortion | 9 | 3.0 |
| Still birth | 22 | 7.3 |
| Live birth | 271 | 89.7 |
DNK: Do not know, TBA: Traditional birth attendants, ANC: Antenatal care
Table 2: Pattern of maternal health-care service utilization
Two hundred seventy-seven women (92.7%) out of 302 delivered in a formal health facility and they included hospital- 78.8% (238/302) and health center-13.9%(42/302). Sixteen women (5.3%) were delivered by TBA/maternity while 6 of them (2.0%) delivered at home. However, all the four women who did not attend ANC consultation were delivered by TBA. Most of them delivered via spontaneous vaginal delivery-(90.7% (274/302) while 14 (4.6%) delivered by cesarean section and 14 (4.6%) by assisted vaginal delivery. Two hundred ninety-three (97.0%) of 302 women carried their pregnancy to term. Two hundred and seventy one (90%) out of 302 of them had live births; the remainder -7.3% (22/302) was still birth. About 280 (92.7%) of the 302 deliveries were attended to by skilled birth attendants including trained auxiliary nurses.
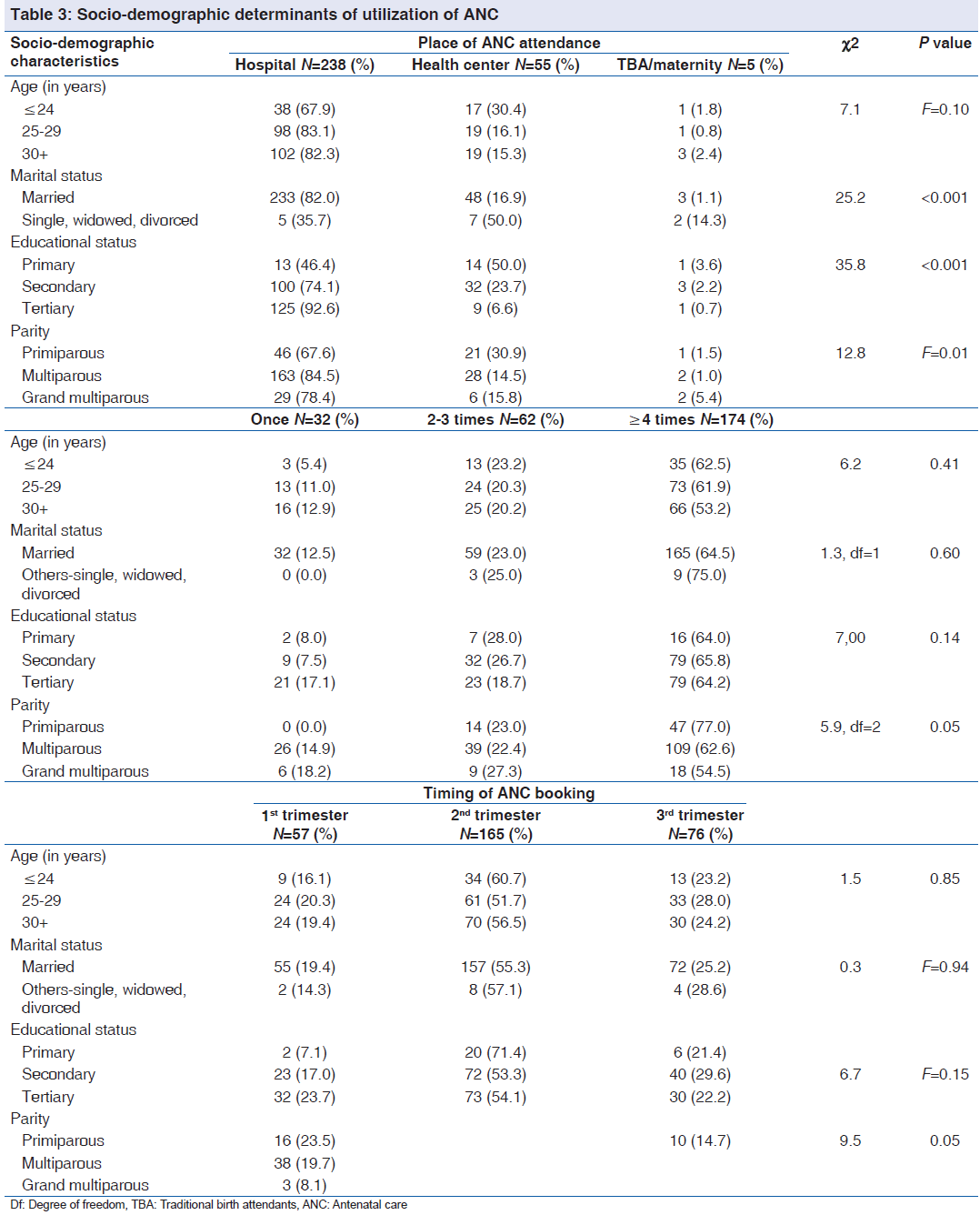
Table 3 shows that there is a significant association was demonstrated between place of ANC attendance and marital status (χ2 = 25.2, P < 0.001), educational status (χ2 = 35.8, P < 0.001) and parity (χ2 = 12.8, F = 0.01). Women who were not in any current marital relationship, as well as those with lower educational status and lower parity were more likely utilize health center or TBA/maternity for ANC. Parity was found to be significantly associated with a number of ANC visits and time of ANC booking. Grand multiparous women were more likely to book for ANC after the first trimester (χ2 = 5.9, P = 0.05) and to have attended ANC less than 4 times prior to delivery (χ2 = 9.50, P = 0.05).
Determinants of place of delivery included age (χ2 = 14.8, P < 0.01 marital status (χ2 = 12.2, P < 0.01), educational status (χ2 = 32.6, P < 0.001) and parity (χ2 = 11.5, P = 0.02) as shown in Table 4. The likelihood of not delivering in a hospital was associated with being single and having lower educational status. On the other hand, those with higher educational status and are multiparous were more likely to have delivered in a hospital while a significant proportion of grand multiparous women delivered in the TBA/maternity.
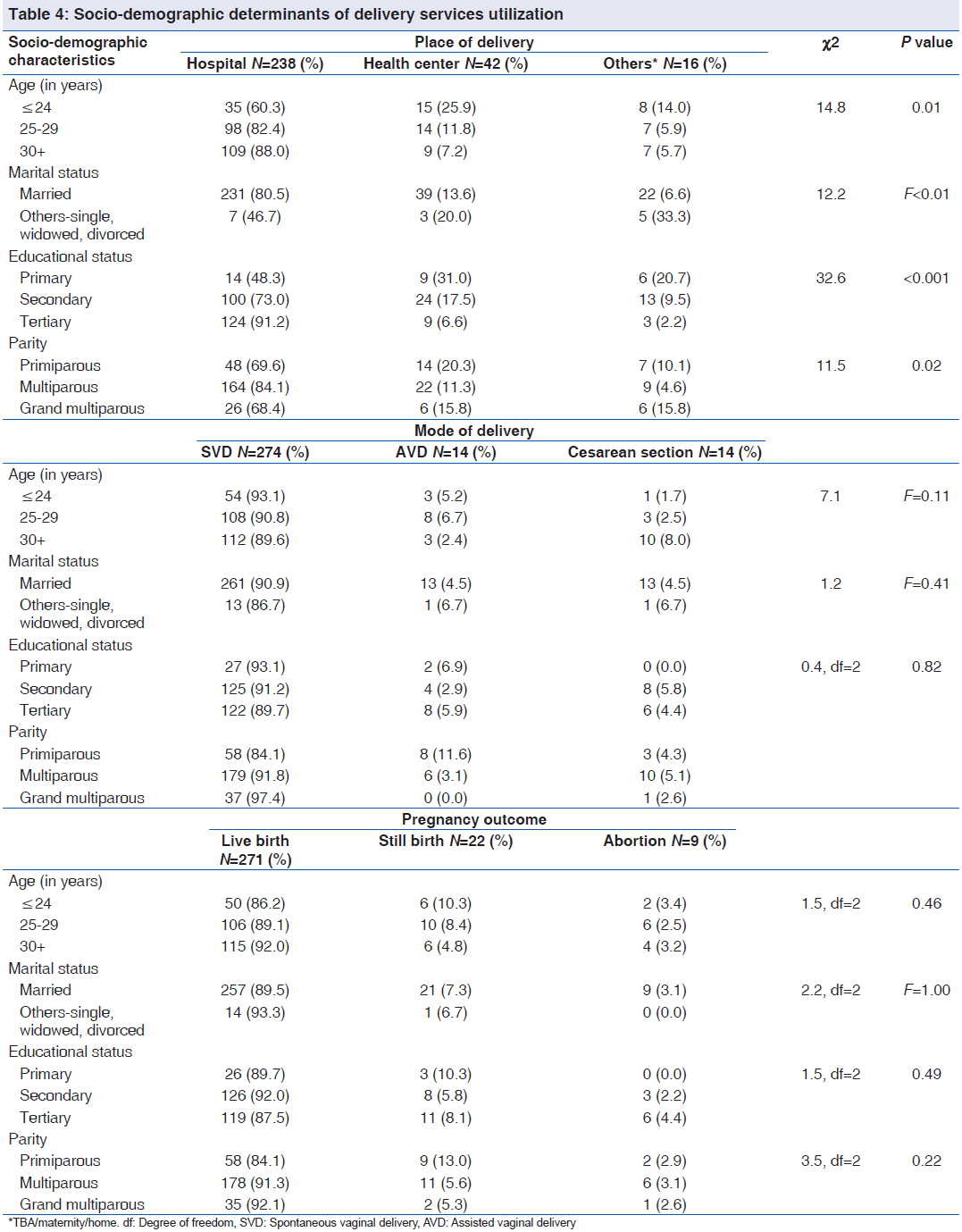
Socio-demographic factors were found to significantly influence the choice of place of delivery. Younger women, those who were not married, those with lower educational status as well as grand multiparous women were more likely to have delivered either by TBA/maternity. More primiparous women delivered either by assisted vaginal delivery or by cesarean section. Furthermore, a greater proportion of them suffered more fetal loss, although not statistically significant.
Table 5 shows that older mothers were more likely to have utilized the health center or hospital for ANC services than either not utilizing any all or patronizing TBA/maternity. Furthermore, women with higher educational status were more likely to have utilized hospitals for ANC services rather than not utilizing or utilization of informal health facility. Women of higher parity and those who were not married on the other hand were less likely to have used health center or hospital for ANC services. For the increase in age the odds of utilizing a health center (P = 0.10, OR = 1.37; CI = 0.52-3.63) and the hospital (P = 0.10, OR = 1.70, CI = 0.66-4.38) for ANC increased by 37.0% and 70%, respectively.
| Socio-demographic characteristics | Place of ANC | OR | 95% CI |
|---|---|---|---|
| Age (in years) | Health center | 1.37 | 0.52-3.63 |
| Parity | 0.19 | 0.05-0.78 | |
| Educational status | 0.56 | 0.18-1.7 | |
| Others-single, | 0.11 | 0.02-0.75 | |
| widowed, divorced | |||
| Age (in years) | Hospital | 1.70 | 0.66-4.38 |
| Parity | 0.30 | 0.08-1.18 | |
| Educational status | 2.06 | 0.69-6.16 | |
| Others-single, | 0.03 | 0.00-0.21 | |
| widowed, divorced | |||
| Reference category | Othersµ | ||
| Age (in years) | Health center | 1.17 | 0.57-2.39 |
| Parity | 0.50 | 0.19-1.32 | |
| Educational status | 1.09 | 0.48-2.48 | |
| Others-single, | 0.20 | 0.38-1.10 | |
| widowed, divorced | |||
| Age (in years) | Hospital | 2.06 | 1.08-3.92 |
| Parity | 0.50 | 0.21-1.19 | |
| Educational status | 3.18 | 1.53-6.63 | |
| Others-single, | 0.12 | 0.03-0.54 | |
| widowed, divorced | |||
| Reference category | Othersβ |
TBA: Traditional birth attendants, ANC: Antenatal care, OR: Odds ratio, CI: Confidence interval. μNo ANC, TBA/maternity, βHome, TBA/maternity
Table 5: Odds of utilization of maternal health-care services and socio-demographic characteristics
Similarly, increase in age (P < 0.01, OR = 2.06; CI = 1.08-3.92) and higher educational status of mothers (P < 0.001, OR = 3.18; CI = 1.53-6.63) were associated with an increased chance of utilizing of the hospital for delivery services. Women who were aged were twice more likely to have used hospital for delivery, likewise women who were aged less than. Also, for every change in educational status the odd of utilizing hospital for delivery increases by 3 times. While women high parity and those who were not married is were less likely to have utilized both health center and hospital for delivery.
Discussion
Most mothers in our study utilized a formal health facility (hospital and health center) for ANC (97.0%) and delivery (92.7%) services and 58.4% of then visited the ANC clinic at least 4 times prior to delivery even though only about 19% of them booked within the first 3 months of pregnancy. About 10% of them had adverse pregnancy outcome. Use of hospital for MH services was significantly associated with older age, being married, high educational status and high parity. Late booking for ANC services was found to be associated with high parity.
The study revealed that most women studied accessed ANC services in formal health facility. ANC attendance reported in this study is more than the national average of 61% of at least one ANC visit during the pregnancy.[9,14] Most of the women utilized hospitals, which in most cases are a private facility rather than health centers because of convenience. It also showed that ANC service utilization in rural communities South Eastern Nigeria is better than in other parts of the country. In western Nigeria, ANC attendance was reported to be 84%,[15] while in northern Nigeria ANC service utilization rate was found to be < 40%.[16,17] Although most women surveyed accessed ANC services, a closer look into ANC service utilization revealed obvious inadequacies. Few (19%) of them attended ANC for the first time during their most recent pregnancy in the first trimester. Also, about 30% of them attended ANC less than 4 times prior to the delivery which is less than the minimum number of attendance recommended by WHO. More than half (55.4%) of the respondents surveyed booked for ANC in the second trimester of their pregnancy. Gharoro and Igbafe[18] reported a median booking gestational period of 23.7 weeks among ANC attendees in Benin. Metgud et al.[19] reported that 56.9% of ANC attendees in Ethiopia booked within 4-6 months of gestation.
High ANC attendance (>90%) is common among pregnant women in sub Saharan Africa.[10,11,19-21] However, there are variations in the average number of ANC visits and in most cases timing of ANC booking is poor as only 19.1% of the mothers booked within the first trimester. In Kenya, only 14% of the pregnant women in rural areas attend ANC for the first time in pregnancy during the first trimester, even though median ANC visit is 4. In Uganda, self-reported ANC visits among attendees was 37.1% while < 30% of them reported attending ANC for the first time in the first trimester.[10] The scenario is even worse in some countries in South East Asia. In Bangladesh, only half of the rural pregnant women received ANC services during their last pregnancy and average ANC visits per pregnancy among these women were less than optimal (1.39 times).[12]
Most common reasons identified why pregnant women book late for ANC were ignorance or misconception of the purpose and right timing of ANC.[22] Kessner index classifies women who book at 28 weeks or later as high-risk pregnancy are considered as not having adequate care, even though are booked pregnancies. In line with this WHO emphasizes early booking rather than the number of ANC attendance.[23] Late ANC registration and inadequate ANC attendance pre-dispose pregnant women to increased risk of maternal morbidity and mortality and poor pregnancy outcome. Women who book late for ANC lose the opportunity to benefit from early detection and effective control/treatment of some disease conditions that may impair their health and that of their babies.
In this survey, more than 90% of the women delivered in a health facility and were attended to by a skilled birth attendant, however few of them were delivered by TBA and fewer delivered at home. Hence, agrees with the findings of an earlier study conducted in the region.[12] Expectedly, the most common mode of delivery was via spontaneous vaginal delivery; however, cesarean section rate of 5% was reported in this study. This invariably suggests availability of emergency obstetric care service to these women. Furthermore, the study revealed a high fetal loss of about 10%. Hence, it can be said that availability of routine and emergency obstetrics services though improves MH outcome, does not always translate into better pregnancy outcome; rather adequate utilization of MH services. In Nigeria, despite the availability of numerous interventions aimed at reducing perinatal and maternal mortality, much progress has not been made over the years.[9] In addition, high fetal loss often results in high fertility rate, which further increases risks associated with pregnancy with result negative impact on maternal morbidity and mortality. Consequently, even as efforts are being made toward increasing access to these services, measures should also be taken to ensure the adequate utilization. Invariably, this is what the recently launched IMNCH strategy is aimed at achieving.
Majority of these women (92.7%) delivered in a formal health facility. Only 7% of them delivered outside a health facility, a proportion, which is low when compared with other parts of Nigeria.[17,23,24] In Sagamu and Ife reported rate of non-facility delivery among pregnant women were 14% and 24%, respectively while 70% home delivery rate has been reported in northern Nigeria. Also, in East Africa high ANC attendance was not associated with high facility delivery. Facility delivery ranges between 41% and 83%. Most deliveries take place at homes and some occasions in the house of a TBA.[11,25] Outcome of 10% of the pregnancies was not favorable. A study in Kenya reported higher fetal loss of 14%; however, highlighted a positive association between higher ANC attendance and perinatal outcome.[26] Also, when compared to some rural communities in South East Asia, proportion of facility delivery reported in this region was found to be higher.[27,28]
Association between MH service utilization and socio-demographic characteristics are varied. Socio-demographic factors primarily influenced the choice of place utilized for MH services. Women who were not married alongside women with lower educational status and parity utilized lower level of health-care and non-formal health-care facilities. Also, younger women utilized the hospital less for delivery. This is probably because such women are often less socio-economically empowered and as such will prefer health facilities providing care at minimal cost. Also, these women are less experienced on issues pertaining to MH and hence depend more on opinions of relatives and friends on issues pertaining to MH care seeking practices. In addition, fewer ANC visits and late timing of ANC registration was found to be associated with higher parity. While non-facility delivery was a commoner among younger women, unmarried women – single, widowed, divorced or separated women with lower educational status and grand multiparous women. However, age, marital status and educational status were found not to have any significant influence on the timing of first ANC visit and number of ANC visits.
Several local and international studies have consistently linked maternal educational status and MH care service utilization. Better service utilization is often associated with a higher educational status.[2,10,11,26,28] The effects of age, marital status and parity on MH services care seeking behavior are varied. Among women in northern Nigeria, Idris et al.[16] had earlier reported that women with higher educational status and those who were aged >18 years at first pregnancy were more likely to at access MH care services in a health facility. However, no association was demonstrated between parity and MH care service utilization. However, other studies have demonstrated an inverse relationship between parity and ANC attendance as women of higher parity tend to use ANC less.[11,26,29,30]
Elsewhere in Kenya low ANC utilization was associated with extremes reproductive age and low socio-economic status and being a single woman.[21] In Bangladesh beside higher educational status, age at birth, parity and access to media were found to be associated with adequate and satisfactory MH care services. It was also observed that women in the extremes of their reproductive age utilized MH care services more than those in the middle of their reproductive age.[12,28]
Some studies attributes low maternal care utilization in most rural communities to believe that pregnancy is a natural process requiring no medical intervention and low awareness of benefits of ANC. Others report that women in rural areas rate the services of TBA as being of higher quality than that of medical health-care providers, particularly with regards to interpersonal communication and relationship.[2,28,31] On the hand, education is believed to improve MH care service utilization by the increased level of health awareness and greater knowledge of available health services among educated women, increased knowledge of benefits of maternal care services, improved ability of educated women to afford the cost of medical health-care and their enhanced level of autonomy.[2]
Conclusions
The study revealed high maternal services utilization in South East Nigeria, even though there are obvious gaps of delayed booking for ANC services and inadequate ANC attendance. Fetal loss of 10% is also significant and should be addressed. The risk of non-utilization of ANC was associated with younger age and high parity while the use of use of hospital services was high for multiparous women. Consequently as part of measures to ensure successful implementation of IMNCH Strategy, health education interventions should be focused on encouraging pregnant women to register for ANC early and to have at least 4 ANC visits prior to delivery. Full adoption and implementation of focused ANC therefore provides a viable option for addressing this challenge. Also, measures should be taken to address barriers that limit utilization of MH care services by socially disadvantaged women.
Acknowledgment
The authors greatly appreciate the participation in this study of women who attend the ANC at the Nnamdi Azikiwe University Teaching Hospital outstations at Neni, Ukpo and Umunya all in Anambra State.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Lule E, Ramana GN, Rosen J. Maternal and Reproductive Health Services. Washington DC, USA. World Bank Group; 2011. Available from: http://www.web.worldbank.org. [Last accessed on 2012 Oct 5].
- Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria – Looking beyond individual and household factors. BMC Pregnancy Childbirth 2009;9:43.
- Boschi-Pinto C, Bahl R, Martines J. Limited progress in increasing coverage of neonatal and child-health interventions in Africa and Asia. J Health Popul Nutr 2009;27:755-62.
- WHO, UNICEF, UNFPA, World Bank. Trends in Maternal Mortality: 1990-2010. WHO, UNICEF, UNFPA and The World Bank Estimates. Geneva: World Health Organization; 2012. p. 59.
- WHO. Who Antenaltal Care Randomised Trial: Manual for the Implementation of the New Model. WHO/RHR/01.30. Geneva: UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction; 2002. Available from: http://www. whqlibdoc.who.int/hq/2001/WHO_RHR_01.30.pdf. [Last accessed on 2013 Mar 28].
- Villar J, Bergsjo P. WHO Antenatal Care Randomized Trial: Manual for the Implementation of the New Model. Geneva: WHO; 2002.
- Ejembi CL, Alti-Muazu M, Chirdan O, Ezeh HO, Sheidu S, Dahiru T. Utilization of maternal health services by rural Hausa women in Zaria environs, Northern Nigeria: Has primary health care made a difference? J Community Med Prim Health Care 2004;16:47-54.
- FMOH. Saving Newborn Lives in Nigeria: Newborn Health in the Context of the Integrated Maternal, Newborn and Child Health Strategy. 2nd ed. Abuja: Federal Ministry of Health, Save the Children, Jhpiego, FMOH; 2011.
- FMOH. Saving Newborn Lives in Nigeria: Newborn Health in the Context of Integrated Maternal, Newborn and Child Health Strategy. Abuja: FMOH, Save the Children, Access, FMOH; 2009.
- Kiwuwa MS, Mufubenga P. Use of antenatal care, maternity services, intermittent presumptive treatment and insecticide treated bed nets by pregnant women in Luwero district, Uganda. Malar J 2008;7:44.
- Mpembeni RN, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, Mushi D, et al. Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: Implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth 2007;7:29.
- Rahman MM, Islam RM, Islam AZ. Rural-urban differentials of utilization of ante-natal health-care services in Bangladesh. Health Policy Dev J 2008;6:117-25.
- Ibeh CC. Is poor maternal mortality index in Nigeria a problem of care utilization? A case study of Anambra State. Afr J Reprod Health 2008;12:132-40.
- National Population Commission (NPC)/Orc Macro. National Demographic and Health Survey. Abuja: NPC; 2008.
- Iyaniwura CA, Yussuf Q. Utilization of antenatal care and delivery services in Sagamu, South Western Nigeria. Afr J Reprod Health 2009;13:111-22.
- Idris SH, Gwarzo UM, Shehu AU. Determinants of place of delivery among women in a semi-urban settlement in Zaria, Northern Nigeria. Ann Afr Med 2006;5:68-72.
- Adamu YM, Salihu HM. Barriers to the use of antenatal and obstetric care services in rural Kano, Nigeria. J Obstet Gynaecol 2002;22:600-3.
- Gharoro EP, Igbafe AA. Antenatal care: Some characteristics of the booking visit in a major teaching hospital in the developing world. Med Sci Monit 2000;6:519-22.
- Metgud CS, Katti SM, Mallapur MD, Wantamutte AS. Utilization patterns of antenaltal services among pregnant women: A longitudinal study in rural area of North Karnataka. Al Ameen J Med Sci 2009;2:58-62.
- Blaauw D, Penn-Kekana L. Socio-economic Inequalities and Maternal Health in South Africa. Johannesburg: Health Systems Development Programme; 2002. Centre for Health Policy, University of Witwatersrand. [Last accessed on 2010 Jan 31].
- van Eijk AM, Bles HM, Odhiambo F, Ayisi JG, Blokland IE, Rosen DH, et al. Use of antenatal services and delivery care among women in rural western Kenya: A community based survey. Reprod Health 2006;3:2.
- Ebeigbe PN, Igberase GO. Reasons given by pregnant women for late initiation of antenatal care in the Niger Delta, Nigeria. Ghana Med J 2010;44:47-51.
- Lamina MA, Sule-Odu AO, Jagun EO. Factors militating against delivery among patients booked in Olabisi Onabanjo University Teaching Hospital, Sagamu. Niger J Med 2004;13:52-5.
- Asekun-Olarinmoye EO, Bamidele JO, Egbewale BE, Oyebola I, Olarinmoye A, Ojofeitimi EO. Consumer assessment of perceived quality of antenatal care services in a tertiary health care institution in Osun State, Nigeria. J Turk Ger GynecolAssoc 2009;10:89-94.
- Ankunda R, Arinaitwe M, Ekirapa-Kiracho E, Bakeera S, Mutebi A, Kiwanuka SN, et al. Making health systems work for the poor: Women’s perceptions of ANC and delivery care services, a community perspective. Future health systems study, Makerere University School of Public Health: Research summary. Available from: http://www.musph. ac.ug, www.futurehealthsystems.org. [Last accessed on 2010 Mar 21].
- Brown CA, Sohani SB, Khan K, Lilford R, Mukhwana W. Antenatal care and perinatal outcomes in Kwale district, Kenya. BMC Pregnancy Childbirth 2008;8:2.
- Nisar N, White F. Factors affecting utilization of antenatal care among reproductive age group women (15-49 years) in an urban squatter settlement of Karachi. J Pak Med Assoc 2003;53:47-53.
- Ye Y, Yoshida Y, Harun-Or-Rashid M, Sakamoto J. Factors affecting the utilization of antenatal care services among women in Kham District, Xiengkhouang province, Lao PDR. Nagoya J Med Sci 2010;72:23-33.
- Rahman KM. Determinants of maternal health care utilisation in Bangladesh. Res J Appl Sci 2009;4:113-9.
- Jimoh AA. Utilisation of antenatal services at the provincial hospital, Mongomo, Guinea Equatoria. Afr J Reprod Health 2003;7:49-54.
- Ribera JM, Hausmann-Muela S, D’Alessandro U, Grietens KP. Malaria in pregnancy: What can the social sciences contribute? PLoS Med 2007;4:e92. [Last accessed on 2011 Jan 30].




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.