Splenic Tuberculosis Presenting as Ascites in Immunocompetant Patient
- *Corresponding Author:
- Dr. Sunil Kumar
Department of Medicine, DMIMS, Sawangi, Wardha, India. Maharashtra - 442 005, India.
E-mail: sunilkumarmed@gmail.com
Abstract
Tuberculosis can involve any part of the gastrointestinal tract from mouth to anus, the peritoneum and the pancreatobiliary system. Here we report a case of splenic tuberculosis in a 60-year-old man who presented with ascitis. Splenic tuberculosis is an unusual clinical presentation, especially in immunocompetent patients. No primary focus of infection was detected in the lungs or any other organs. The postulated mechanisms by which the tubercule bacilli reach the peritoneum is through direct spread from adjacent organs like spleen in this case.
Keywords
Ascites, Immunocompetent, Splenic tuberculosis
Introduction
Tuberculosis (TB) both in pulmonary and extra pulmonary form continues to be a major health problem worldwide despite notable advances in diagnosis and treatment of the disease. Extra pulmonary tuberculosis comprises 15% of all cases and among them splenic TB is very rare.[1] Splenic TB commonly manifests as fever, left upper quadrant abdominal pain, weight loss and diarrhea. There is no case report available regarding presentation with ascitis especially in immunocompetant patients. The diagnosis is often delayed due to its non specific clinical presentation and difficulties in confirming diagnosis. This report reveals splenic TB undetectable in primary sites in the body presenting as ascites. No primary focus of infection was detected in the lungs or any other organs.
Case Report
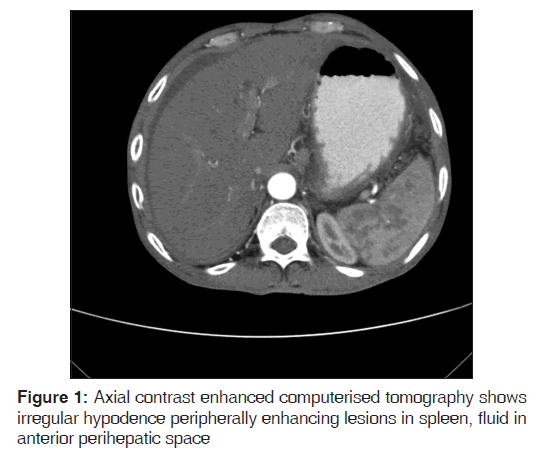
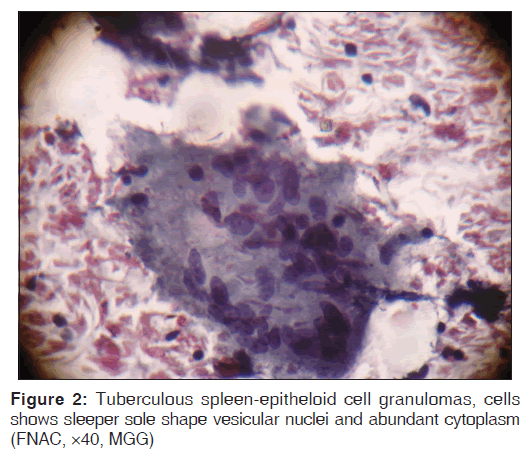
A 60-year-old male patient visited our hospital with vomiting, pain in abdomen and distension of abdomen since one month. He also gives history of weight loss, loss of appetite, low grade fever. He was non-smoker and non-alcoholic. He had no significant past history of pulmonary tuberculosis or any contact with patient of TB or neither had HIV infection. He was not screened for diabetes mellitus and hypertension. On examination he was afebrile, regular pulse at 84/min. His blood pressure was 120/70 mmhg. He was anicteric and there was no lymphadenopathy. On abdominal examination shifting dullness and fluid thrill suggestive of free fluid in the peritoneal cavity was present. Spleen was not palpable. Investigation revealed haemoglobin of 9 gram percent, fasting blood sugar was 98 mg/ dl, erythrocyte sedimentation rate (ESR) of 90 mm/1st hour. His tuberculin test was positive (18 mm). The HIV serologic test was negative. Other Blood biochemical profile like liver function test and kidney function test were within normal limits. The chest X-ray revealed no abnormalities. Abdominal ultrasonography revealed ascites with multiple ill defined areas of hypoechogenesity in spleen. The axial contrast enhanced Computerised Tomography showed irregular hypo dense peripherally enhancing lesions in spleen, and fluid in anterior perihepatic space suggestive of splenic abscess [Figure 1]. There was no bowel thickening, no septa and no lymph node enlargement. The computed tomography (CT) guided fine needle aspiration biopsy from hypo echogenic area of spleen was performed. The cytomorphology showed granulomas with area of caseation in the centre surrounded by variable number of langhans giant cells and epitheloid cells favouring diagnosis of tuberculosis [Figure 2]. Culture and polymerase chain reaction based confirmation could not be contemplated due to inadequacy of sample. Ascitic fluid examination revealed total white cell count of 450 with lymphocyte 85%, protein 4.6 mg/dl, glucose 60 mg/dl, LDH 442 u/l, cholesterol 43 mg/dl. Serum ascitic albumin gradient was 0.8 suggestive of exudative fluid. Tuberculosis is one of the common causes of exudative fluid in this part of the world. Microscopy was requested for malignant cells and mycobacterium which was negative.
The final diagnosis was multiple splenic tubercular abscesses with tubercular ascites. We put him on DOTS category two anti tubercular therapy. He was doing well on follow up which was regular for three month.
Discussion
Extra pulmonary tuberculosis comprises almost 15% of all cases of tuberculosis and among them abdominal organ involvement was observed in 11%.[1] Splenic tuberculosis is a rare clinical condition usually encountered during miliary TB especially in immunocompromised patients in which this is third most (75%) commonly involved organ after lung 100% and liver 82%.[2] The other form is primary involvement of spleen which is extremely rare even rarer if it occurs in immunocompetent person as in our case who presented with tubercular ascites. Only few literatures has mentioned about splenic TB in immunocompetent patients with ascitis.[3] Tuberculous ascites/ peritonitis is always secondary to other tuberculous lesions. This appears to be more common in females than in males, because in females it commonly reaches the peritoneum through tubal infection and attacks the tubes during the sexually active period of life. It may be due to either a local extension from tuberculous lymph node, fallopian tube, tuberculous intestinal ulcer or may be caused by haematogenous or lymphatic spread from distant sources of infection.[4] Although this patient had no previous medical history of pulmonary or extra pulmonary tuberculosis, his only complain was ascites and due to tubercular etiology we searched other site which came out to be splenic abscess as tuberculosis on ultrasonography of the abdomen. Ultrasonography of the spleen can be useful in diagnosis of splenic TB and therapeutic response assessment, it is cost effective and non invasive modality and especially relevant as screening tool. However, histopathological diagnosis is required to pinpoint the aetiology. Tubercular infection can be histopathologicaly identified by the presence of typical caseation along with granulomas of epitheloid cells and langhans giant cells.[5,6] Molecular techniques like real-time PCR can be used for detection of tubercle bacilli directly on clinical specimens but they have limited role in resource poor, developing countries like India. Final diagnosis may need spleenectomy although CT guided splenic puncture as aspiration biopsy is emerging as more ideal and popular methods nowadays.[1] Laparoscopy has role in diagnosis of spleenic T.B. and has proved to be a minimally invasive approach avoiding unnecessary splenectomy.[7]
Peritoneal tuberculosis occurs in three forms: Wet type with ascitis, dry type with adhesions, and fibrotic type with omental thickening and loculated ascites. The postulated mechanisms by which the tubercle bacilli reach the peritoneum and gastrointestinal tract are: (i) hematogenous spread from the primary lung focus in childhood, with later reactivation; (ii) ingestion of bacilli in sputum from active pulmonary focus; (iii) direct spread from adjacent organs; and (iv) and through lymph channels from infected nodes.[8]
Splenic abscess which was turned out tubercular on histological examination and our assumption is tubercular ascites may be extension from splenic abscess.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Ray S, Kundu S, Goswami M, Sarkar D, Saha M. Isolated tubercular splenic abscess: Can we defer splenectomy? Our single experience with anti-tuberculous therapy alone. Indian J Med Microbiol 2012;30:101-3.
- Zhan F, Wang CJ, Lin JZ, Zhong PJ, Qiu WZ, Lin HH, et al. Isolated splenic tuberculosis: A case report. World J Gastrointest Pathophysiol 2010;1:109-11.
- Sahoo SP, Shukla HS. Abdominal tuberculosis. In: Sharma SK, Mohan A, editors. Tuberculosis. New Delhi: Jaypee Brothers; 2001. p. 187-200.
- Kundu PR, Mathur SK, Singh S, Duhan A, Agarwal G, Sen R. Isolated tuberculous splenic abscess in an immunocompetent individual. Asian Pac J Trop Med 2011;4:81-2.
- Gupta A, Hunjan PS, Jain SK, Kaza RC, Kumar V. Tubercular splenic abscess in an immunocompetent patient-A rare entity. Southeast Asian J Trop Med Public Health 2006;37:1196-8.
- Imani Fooladi AA, Hosseini MJ, Azizi T. Splenic tuberculosis: A case report. Int J Infect Dis 2009;13:e273-5.
- Dixit R, Arya MK, Panjabi M, Gupta A, Paramez AR. Clinical profile of patients having splenic involvement in tuberculosis. Indian J Tuberc 2010;57:25-30.
- Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res 2004;120:305-15.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.