Spontaneous Intracranial Hypotension–A Rare but Important Cause of Secondary Headache
Received: 09-Jan-2024, Manuscript No. amhsr-24-124756; Editor assigned: 11-Jan-2024, Pre QC No. amhsr-24-124756 (PQ); Reviewed: 26-Jan-2024 QC No. amhsr-24-124756; Revised: 02-Feb-2024, Manuscript No. amhsr-24-124756 (R); Published: 09-Feb-2024
Citation: Soni A. Spontaneous Intracranial Hypotension-A Rare but important Cause of Secondary Headache. Ann Med Health Sci Res. 2024;14:900-904
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Spontaneous intracranial hypotension is an uncommon cause of headache. Diagnosis requires high index of suspicion. It can be easily missed if not considered in differentials. It can be missed on plain MRI if intra venous contrast is not given.
We report nine cases of spontaneous intracranial hypotension who came with acute to subacute presentation of postural headache. Four patients were treated conservatively with bed rest and IV fluids. These patients were followed up clinically and radiologically. Follow up clinical and MRI showed complete resolution of symptoms in 4 conservatively treated patients. Two patients were treated surgically. One patient required bilateral craniotomy in view of worsening of subdural haematoma. One patient was treated with bilateral craniotomy and epidural blood patch. Three patients were treated with epidural blood patch alone. All patients except one responded to treatment on follow up.
Spontaneous intracranial hypotension requires clinical suspicion and a contrast MRI for diagnosis. Conservative trial should be given before proceeding for epidural blood patch unless there is worsening of symptoms or signs. Duration of observation for conservative treatment before proceeding for epidural blood patch is individualized. In select subset bilateral craniotomy for subdural haematoma is required along with epidural blood patch.
Keywords
Spontaneous Intracranial Hypotension (SIH), Epidural Blood Patch (EPB), Subdural Haematoma (SDH), Postural headache.
Introduction
Spontaneous Intracranial Hypotension (SIH) is defined by the international headache society as headache which occurs within 15 minutes of upright position and relieved within 30 minutes of recumbency. It occurs in 5 of 1,00,000 individuals per year with peak incidence in fourth decade of life and female to male ratio of 2:1 [1].
Clinical features include postural headache, nausea, vomiting, cranial nerve palsies leading to diplopia, neck pain and stiffness and obtundation. Tinnitus, hearing loss and vertigo may be associated symptoms. Mean time for onset of symptoms to neurology consultation is 1-2 days in acute postural headache (thunderclap headache) and may be up to one year in chronic postural headache.
Clinical examination is mostly normal and occasionally reveals cranial nerve palsies. It is characterized by very typical contrast MRI brain findings like diffuse pachymeningeal enhancement, brainstem sagging, pituitary enlargement or hyperaemia, venous engorgement and bilateral subdural effusion [2-4]. Investigations are directed to find out cause of CSF leak like CT myelography, MR myelography and radionuclide scans.
Treatment is strict bed rest and supportive treatment initially like anti-emetics, caffeine, glucocorticoids. Worsening of symptoms warrant further investigations to find out cause of leak. Treatment then involves injecting epidural blood patch. Blood culture should be done before collecting autologous blood. Epidural blood patch can be dedicated, if exact site of leak is known. Sometimes a blind epidural autologous blood patch needs to be performed if site of exact CSF leak cannot be localized after thorough investigations. Single or repeat patch may be required if clinically indicated.
In rare cases evacuation of bilateral SDH is required along with blood patch if raised ICP causes mass effect and tonsillar herniation.
We report Nine cases seen within span of 2 years with diagnostic history and MRI findings.
Case Presentation
Case 1
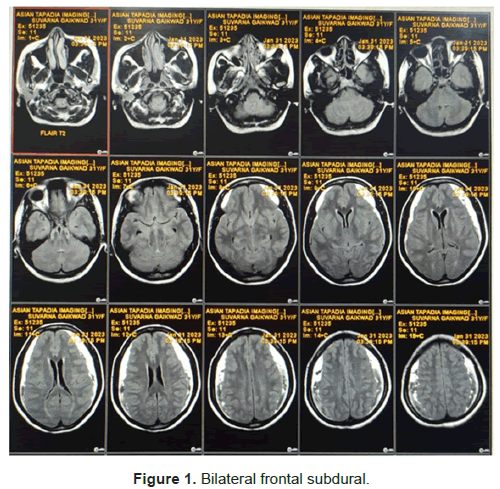
A 34 year old female was referred to ER in view of acute symptomatic headache since 7 days. She had history of sudden bout of severe cough like a spasmodic cough subsequent to which had acute severe neck pain and giddiness and vomiting and worst ever headache. Subsequently she noticed that headache was worst when upright, neck pain, nausea, vomiting and tinnitus worsened when upright. CT brain done showed bilateral subdural haematoma. (Figure 1) Hence was referred to ER regarding need of surgery.
On enquiry there was no history of trauma, fall, fever or any past history of headaches. She was not on any antiplatelets or anticoagulants and no past bleeding tendency and PT/INR, APTT, Bleedng time and clotting time was normal. On clinical examination she was afebrile, there was terminal neck stiffness but field fundus and rest of neurological examination was normal and there were no focal neurological signs.
Based on history and examination and CT findings and postural nature of headache possibility of spontaneous intracranial hypotension was thought and MRI contrast was done which confirmed clinical suspicion.
Started on intravenous fluids, antiemetics strict bed rest and coffee twice a day, patient felt symptomatically better, headache decreased nausea and vomiting decreased. After one week of stay she was given a trial of upright posture and reappearance of headache was noticed but after longer duration that is after two hours of becoming upright, and intensity had decreased. She was advised further rest for two weeks and follow up. Advised to have gradual upright posture.
Headache significantly decreased over follow up, no nausea vomiting, was able to stand without giddiness and tinnitus decreased.
A repeat MRI was done after 4 weeks and showed near complete resolution of subdural and pachymeningeal enhancement. At follow up which is one year from symptoms now. Patient is asymptomatic.
Case 2
A 38 year old female presented with acute severe headache and vomiting started suddenly since 5 days. Recalls worst ever headache of life with nausea and vomiting when upright and neck pain. Headache decreased after lying down.
No fever trauma or past significant history.
Clinical examination was normal. CT brain was done at local place on clinical suspicion of SAH in view of thunderclap headache. As CT was normal and headache persistent was referred to our centre. In view of clinical suspicion contrast MRI brain and venography was done which showed pachymeningeal enhancement and brainstem sagging. MRI spine was done to see for leak. Patient was started on iv fluids bed rest NSAID’s and antiemetics SOS. Patient was symptomatic despite rest for initial 2 days and subsequently improved over next few days and upright trial was given after 7 days where headache intensity had decreased significantly. Patient was observed closely for new signs and symptoms and were explained about Epidural blood patch if worsening.
As was better after 10 days was discharged and advised to take complete bed rest for 2 weeks. Came to follow up was better, advised gradual upright posture till headache reappears. MRI four weeks later showed resolution of enhancement. Patient is asymptomatic now 6 months follow up.
Case 3
A forty-year female came with acute onset headache and vomiting and postural symptoms. She had these symptoms for 2 weeks prior to OPD consultation. She herself took rest for 1 week after which her headache decreased but was persistent. On examination fields and fundus was normal.
No neck stiffness and no focal deficit. MRI brain (P+C) was done which showed bilateral subdural effusion and pachymeningeal contrast enhancement.
As already headache had decreased, she was advised Bed rest at home and oral fluids and Paracetamol SOS. Her headache significantly decreased over course. Repeat MRI showed improvement.
Case 4
Patient 54 year old male came with severe postural headache and bilateral subdural without any history of trauma. Patient was admitted and observed in neurosurgical ICU. In view of worsening of symptoms and drowsiness and mass effect bilateral mini craniotomy with draining of effusion was done. Patient improved initially but again had recurrence of symptoms with reappearance of effusion. Neurology call was given. Retrospectively with nontraumatic bilateral subdural and postural headache and deterioration post craniotomy contrast MRI was done and possibility of SIH was considered. Osmotic diuretics were stopped, patient hydrated well and with gradual improvement was weaned off and extubated. His further hospital course was uneventful. Was advised CT myelography. Lost to follow up after discharge.
Case 5
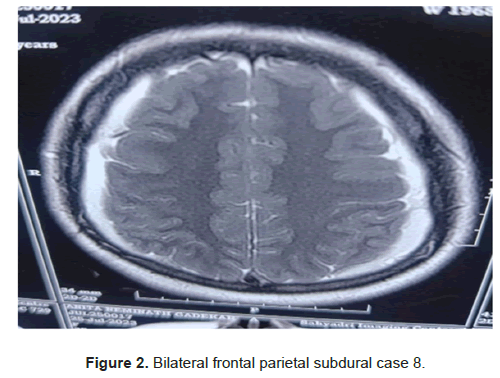
A 38 year male, presented to OPD with severe headache especially on upright and complained of uneasiness on standing. Duration of symptom were almost 1 month. There was no history of trauma or any inciting event. His MRI brain showed findings typical for intracranial hypotension (Figure 2). He was given a conservative trial with rest antiemetics and acetaminophen. But had persistent symptoms. MRI myelography did not reveal any localized area of leak. Hence lumbar epidural blood patch 10 ml was done by anaesthetist and Trendelenburg position given. Headache decreased by 50 percent but had some radiculopathy symptoms which settled with pregabalin. He was slowly given upright position. His headache significantly decreased and was allright on 15 days follow up. His repeat MRI done showed complete resolution of symptoms.
Case 6
A 30 year female was referred from neurosurgeon in view of MRI showed bilateral SDH. No h/of trauma. History of headache 25 days back subsided with symptomatic treatment. Now headache on upright and vomiting with sitting. Had persistent vomiting in ER. No h/of fever. MRI contrast showed typical pachymeningeal enhanacement and brainstem sagging. Started on iv fluids and symptomatic treatment and bed rest. Significantly improved over 2 weeks. Had mild symptoms on getting up.
Case 7
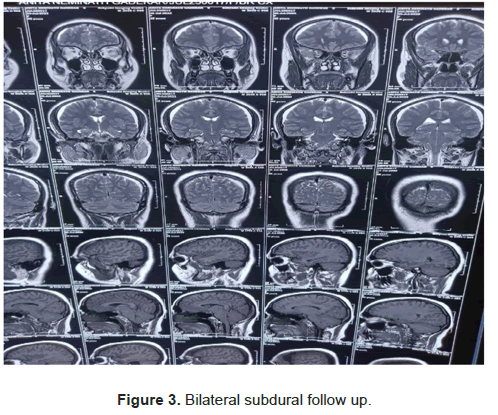
A 25 female came with acute severe headache nausea and vomiting and tinnitus on getting up. She improved with symptomatic treatment at local place. In view of recurrence of headache CT was done and referred in view of bilateral SDH. MRI Brain (P+C) done on clinical suspicion of SIH. On bed rest was 50 percent better. Recurrence on upright. MR myelo did not reveal any significant demonstratable leak. Had worsening of headache and became drowsy and subdurals increased. Hence bilateral craniotomy and epidural blood patch done in same setting and followed up. Symptomatically improved over next few days. Signficantly improved over next follow up (Figure 3).
Case 8
A 37 year old male came with severe headache and neck pain of almost one and half months duration. In view of initial MRI showing subdural haeamatoma was investigated with DSA. After DSA, contrast MRI was done and diagnosed intracranial hypotension. Conservative trial failed as neck pain was persistent. MR myelogram did not localize site of leak hence blind patch 20 ml was given under C-arm guidance by anaesthesiologist at lower dorsal level. Followed by symptomatic relief for few days followed by relapse. Repeat MR myelo showed leak at cervical site. As anaesthetist deferred injecting EPB at cervical area. Hence was referred to higher centre.
Case 9
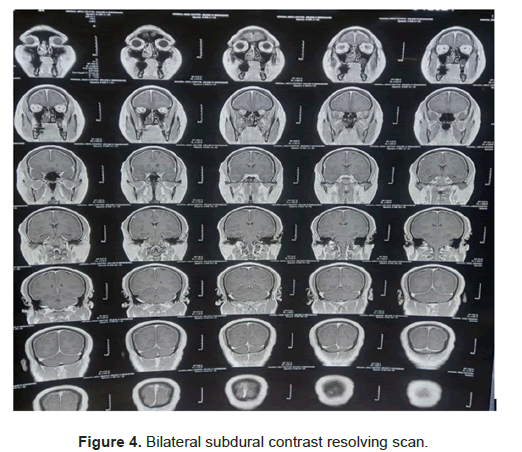
A 34 female with persistent throbbing headache predominantly postural presented to OPD after 1 month of symptoms. MRI brain and contrast did show bilateral subdural and pachymeningeal contrast enhancement (Figure 4). Tried conservative trial but pain was very severe and patient was not able to even sit for few minutes. Hence a blind epidural 15 ml blood patch was done at lower dorsal and upper lumbar level. Symptomatically patient was significantly better within 48 hours .Follow up MRI showed resolution of subdurals. At 1 month follow up MRI shows significant resolution. Patient is asymptomatic.
Discussion
Spontaneous intracranial hypotension can be easily missed without a thorough history. Postural Headache is the commonest symptom. Over a period the postural variation may not be present. Cases described in literature are mostly patients who had come for chronic postural headache.
Only few cases had presented acutely with thunderclap headache and so initially diagnosis was missed. In a survey of 28 patients Schieving and colleagues reported that a thunderclap headache was presenting symptom in only four cases and three of them who were admitted early after headache onset had nuchal rigidity [5]. Most of the patients seen our series had presented with acute thunderclap headache.
Diagnosis can be easily missed if not clinically suspected in acute setting.
The disruption of meningeal continuity can be triggered by a trivial event such as a minor fall, a sudden twist or stretch, sexual intercourse, a sudden sneeze or vigorous exercise, which the patient often fails to recall as the inciting event [6]. The evidence identifying possible predisposing conditions is limited but enquiry may be made about connective tissue disorders and joint hypermobility disorders; and spinal pathology including osteophytes, disc herniation and discogenic microspurs in direct relation to the site of the spinal leak [7].
Traction on pain-sensitive intracranial and meningeal structures because of the CSF hypovolaemia, particularly sensory nerves and bridging veins, is thought to cause headache and associated symptoms. In the upright position this traction is exaggerated, hence the postural component of the headache. Secondary vasodilation of the cerebral vessels to compensate for the low CSF pressure may contribute to the vascular component of the headache by increasing brain blood volume.
Because jugular venous compression increases headache severity, it seems likely that venodilatation is also a contributing factor to the headache.
Tinnitus, hearing loss and vertigo result from transmission of abnormal CSF pressure to perilymph of cochlea. In a study of 30 consecutive patients of SIH, neurotologic symptoms included dizziness (30) percent, tinnitus (20) percent, aural fullness (20) percent and hearing loss (3) percent.Tinnitus was present in case 1 and subsided over course and ear fullness was present in case 2 and case 3.
Diagnosis is missed when patient presents late and should always be suspected in bilateral non traumatic subdurals. Gadolinium enhanced MRI is must in these settings as diagnosis is missed otherwise.
Role of contrast MRI cant’t be over-emphasized in this setting.
The possibility that the timing of the MRI determines the presence or absence of diffuse pachymeningeal enhancement was reported by Fuh et al., [8] In their series, three of nine (33%) patients did not demonstrate pachymeningeal enhancement on the initial study but had postural headaches with low lumbar opening pressure. Therefore, they recommend that invasive studies, such as lumbar puncture including measurement of lumbar opening pressure, should be done in patients with clinically typical postural headache but normal findings on MRI for the diagnosis of SIH.
How ever MRI can be normal initially in few cases.
MRI may take time to evolve, if clinical suspicion is high diagnosis can be confirmed with CSF manometry or a repeat MRI. Similarly clinical improvement will precede MRI improvement and MRI improvement may take 4-6 weeks.
The outcome of spontaneous intracranial hypotension has been unpredictable. The results of initial MRI were correlated to outcome of treatment in 33 patients with spontaneous intracranial hypotension. A good outcome was obtained in 25 (97%) of 26 patients with an abnormal MRI vs only 1 (14%) of 7 patients with a normal MRI (p=0.00004). These findings show that normal initial MRI is predictive of poor outcome in spontaneous intracranial hypotension. [2,8,9]
Aetiology is also not clear as described in case 1 spasmodic cough literature review, spasmodic cough as a cause of dural tear.
Epidural blood patch (targeted or blind) has been the best modality of treatment described.
How ever many patients who present acutely can be managed conservatively with strict neuro observation for worsening. Both modalities have advantages and disadvantages over one another. Risk of adhesions with blood patch and meningitis, need of repeat patch are worrisome but uncommon complications.
Risk of worsening dementia encephalopathy remains risk of observational treatment.
In a series of 12 patients by ARAI and Rinsho et al., 5 patients responded to conservative treatment and mean duration of response was 13.6 days. 5 patients responded to first EPB. Patients with severe orthostatic headache which persisted two weeks and longer in spite of conservative measures are candidates for EPB.
Single level versus multiple leak sites cannot be commented on basis of clinical findings and requires CT myelo or cisternography to demonstrate leak. Conservative approach may fail if leak is at multiple sites.
Though data is short a large cohort of patients should be studied for conservative trial vs EPB especially in acute setting in resource poor country like India.
Conclusion
Spontaneous intracranial hypotension can easily be missed if not considered in differential diagnosis of secondary headaches. It has varied presentation from thunderclap headache to chronic daily headache. Always suspect in patients with postural headache, and nontraumatic bilateral subdural collection.
Diagnosis is clinical and MRI is confirmatory but may be normal in few cases initially. Conservative treatment like bed rest intra venous fluids remain cornerstone of treatment in select group of individuals.
EPB (either blind patch or dedicated if leak site is found), one or multiple is required if conservative trial fails.
References
- Schievink WI, Meyer FB, Atkinson JL, Mokri B. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286-96.
[Crossref] [Google Scholar] [PubMed]
- Lin WC, Lirng JF, Fuh JL, Wang SJ, Chang FC, et al. MR findings of spontaneous intracranial hypotension. Acta Radiol 2002; 43:249–255.
[Crossref] [Google Scholar] [PubMed]
- Fishman RA, Dillon WP. Dural enhancement and cerebral displacement secondary to intracranial hypotension. Neurology 1993; 43:609–611.
[Crossref] [Google Scholar] [PubMed]
- Tosaka M, Sato N, Fujimaki H, Tanaka Y, Kagoshima K, et al. Diffuse pachymeningeal hyperintensity and subdural ef-fusion/hematoma detected by fluid-attenuated inversion recovery MR imaging in patients with spontaneous intracranial hypotension. AJNR 2008; 29:1164–1170.
[Crossref] [Google Scholar] [PubMed]
- Schievink WI, Maya MM, Moser FG, Simon P, Nuño M. Incidence of spontaneous intracranial hypotension in a community: Beverly Hills, California, 2006–2020. Cephalalgia. 2022;42:312-316.
[Crossref] [Google Scholar] [PubMed]
- Murakami M, Morikawa K, Matsuno A, Kaneda K, Nagashima T. Spontaneous intracranial hypotension associated with bilateral chronic subdural hematomas-case report. Neurol Med Chir. 2000;40:484-8.
[Crossref] [Google Scholar] [PubMed]
- Cheema S, Anderson J, Angus-Leppan H, Armstrong P, Butteriss D. Multidisciplinary consensus guideline for the diagnosis and management of spontaneous intracranial hypotension. J Neurol Neurosurg Psychiatry. 2023;94:835-843.
[Crossref] [Google Scholar] [PubMed]
- Fuh JL, Wang SJ, Lai TH, Hseu SS. The timing of MRI determines the presence or absence of diffuse pachymeningeal enhancement in patients with spontaneous intracranial hypotension. Cephalalgia. 2008;28:318–322.
[Crossref] [Google Scholar] [PubMed]
- Wouter I. Schievink, M. Marcel Maya, Charles Louy. Cranial MRI predicts outcome of spontaneous intracranial hypotension. Neurology. 2005;64:1282-4.
[Crossref] [Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.