Subcutaneous Surprise
- *Corresponding Author:
- Dr. Ramakrishna.Pai. Jakribettu
Department of Microbiology, MES Medical College, Perintalmanna - 679 338, Kerala, India.
E-mail: ramakrishna.paij@gmail.com
Abstract
Melioidosis is a zoonosis caused by the accidental pathogen Burkholderia pseudomallei, which is endemic in Southeast Asia and northern Australia. The mortality of melioidosis is 20-50% even with treatment. Suppurative lymphadenitis caused by melioidosis has been rarely encountered by clinicians practicing in endemic areas. In the majority of previously described patients, the infected lymph nodes were in the head and neck region, except for four patients who presented with unilateral, inguinal lymphadenitis. Hence, we report a case of unilateral suppurative inguinal lymphadenitis caused by B. pseudomallei in a 48‑year‑old lady who presented with groin swelling of 2 months duration.
Keywords
Burkholderia pseudomallei, Inguinal Lymphadenitis, Melioidosis
Introduction
Melioidosis is a zoonotic disease caused by an accidental pathogen Burkholderia pseudomallei. The organism is endemic in Southeast Asia and northern Australia. The mortality of melioidosis is 20-50% even with treatment.[1] Melioidosis has been called the “Great Imitator” because the disease does not show any specific clinical features except perhaps the presentation of suppurative parotitis in children.[2] Suppurative lymphadenitis caused by melioidosis has been rarely encountered by clinicians practicing in endemic areas. Inoculation of B. pseudomallei through the skin is the most common mode of acquisition. In the majority of previously described patients, the infected lymph nodes were in the head and neck region, except for four patients who presented with unilateral, inguinal lymphadenitis in the report of Maciej Piotr Chlebicki and Ban Hock Tan.[3] Here, we report a 48-year-old lady from North Kerala, who presented with groin swelling on the right side of 1 month duration, mimicking tubercular adenitis, which was a clinical surprise of suppurative form lymphadenitis of melioidosis in the subcutaneous region.
Case Report
A 48-year-old homemaker, not a known diabetic, presented with swelling in the right groin and fever of 2 months duration. The fever was mild and intermittent, not associated with chills and rigor. There was no history of trauma to the lower limbs or the right inguinal lymphatics drainage region. The patient was on antibacterial drugs for 2 weeks as prescribed by the family physician. But the swelling did not subside and she was referred to our hospital for further management.
On examination, the patient was well built and well nourished. She was afebrile; pulse was 72 beats per minute regular, and blood pressure was 120/80 mmHg. Systemic examination did not reveal any abnormality. There was a non-tender, 2 × 1.5 cm swelling in the inguinal region on the right side, below the inguinal ligament. Swelling was non-fluctuant, tender, soft in consistency, with local rise of temperature. No cough impulse or bruit was present. There was no ulcer in the draining area. The right lower limb pulses were well felt and there was no evidence of varicose veins or any neurological deficit.
Lab investigations revealed the following: Hemoglobin 12.27 g%, total leukocyte count 8300/mm3, differential count N 68 L 25 E 5 M 1, erythrocyte sedimentation rate (ESR) 25 mm/1st h, HIV/HBsAg negative, random blood sugar 86 mg%, blood urea 20 mg%, and serum creatinine 0.7 mg%. The blood samples sent for culture, two sets with and without antibiotics, were negative. X-ray of the chest as well as an abdominal ultrasound showed no abnormalities.
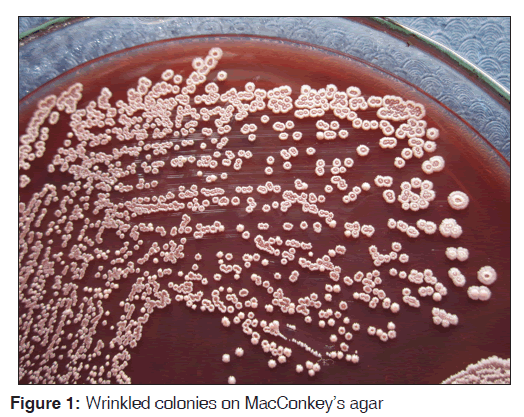
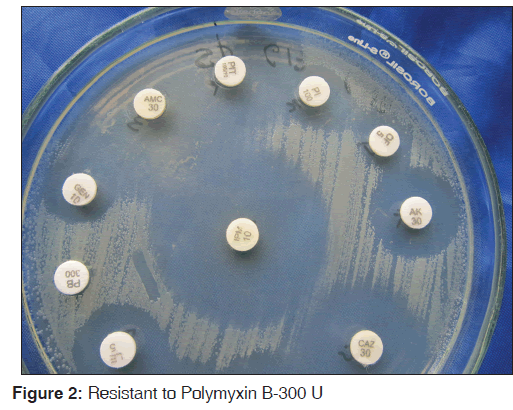
The patient underwent excision biopsy of the lesion through a right inguinal skin crease incision. Intraoperatively, the swelling was above the inguinal ligament and mobile and there was pus in the swelling. The abscess wall was sent for histological examination. Histopathology of the biopsy sample revealed numerous epithelioid granulomas with Langhans giant cells with minimal caseation in fibrous granulation tissue. There were foreign body granulomas and dense lymphoplasmacytic infiltrate with proliferating blood vessels, suggesting tuberculous granulation tissue. The pus was also sent for microbiological investigations, which included Gram’s staining, acid-fast staining, and bacteriological culture, both aerobic as well as anaerobic. The preliminary microbiological testing of the pus by Gram’s staining showed numerous pus cells with bipolar stained (safety pin) Gram-negative bacilli. Hence, B. pseudomallei was suspected. The acid-fast staining did not reveal any acid-fast bacilli (AFB). The sample was later processed for both aerobic as well as anaerobic culture. The aerobic culture revealed wrinkled, lactose-fermenting colonies on MacConkey’s agar [Figure 1]. The isolate was confirmed as B. pseudomallei by characteristic biochemical tests. The isolate gave oxidase-positive, motile, fermented glucose, lactose, mannitol, and maltose with acid only. Nitrate was reduced to free nitrogen. Arginine was dihydrolysed. The isolate was resistant to Polymyxin B [Figure 2]. The anaerobic culture was negative even after 7 days of incubation. Hence, she was given 2 weeks of intravenous ceftazidime and then discharged. She was put on cotrimoxazole and doxycycline for 6 weeks. The AFB culture was found to be negative after 3 months of incubation. On follow-up after 9 months following therapy, the patient had no signs of any recurrence and her systemic examination was normal.
Discussion
The Gram-negative bacterium, B. pseudomallei, was first isolated by Captain A. Whitmore, a British pathologist at Burma, while treating a young boy dying with pneumonia in 1911.[4] In 1921, Stanton and Fletcher coined the term melioidosis.[5] It is endemic in Southeast Asia and northern Australia. The mortality of acute severe melioidosis is 20-50% even with treatment.[1] B. pseudomallei is an “accidental pathogen.”[6] It is an environmental organism that has no requirement to pass through an animal host in order to replicate. From the point of view of the bacterium, human infection is an evolutionary “dead end.”[6] The infection is acquired mainly by inoculation of the pathogen through the skin or pre-existing skin wounds.[7] But person to person transmission of the infection is a relatively rare entity.[8] The infection is mainly seen in the individuals who are in contact with soil, mainly farmers and gardeners. Melioidosis is mainly associated with diabetes mellitus. Even chronically ill patients with chronic renal disease, alcoholism, malignancy, connective tissue diseases, and chronic lung disease are at higher risk for the development of melioidosis. It can have various presentations, ranging from mild and subclinical infection to acute septicemia, and even chronic localized infection. Uncomplicated, localized infection usually involves skin or subcutaneous tissues.
Melioidosis has been called the “Great Imitator” because the disease does not show any specific clinical features except perhaps the presentation of suppurative parotitis in children.[2] The histopathology of the specimens in melioidosis usually reveals the features of chronic granulomatous infection like tuberculosis. If bacterial culture of the infected specimen is not done, then the disease is considered as tuberculosis and treated for the same. So, in our case, if we had not done the bacteriological culture, then the patient would have been misdiagnosed as tubercular adenitis, based on histopathological finding of chronic granulomatous infection alone. Therefore, this case shows the importance of the bacteriological culture for the diagnosis of melioidosis.
Suppurative lymphadenitis caused by melioidosis has been rarely encountered by clinicians practicing in endemic areas. In the majority of previously described patients, the infected lymph nodes were in the head and neck region, except for four patients who presented with unilateral, inguinal lymphadenitis in the report of Maciej Piotr Chlebicki and Ban Hock Tan.[3] Here, we report a case of suppurative inguinal lymphadenitis caused by melioidosis in a 48-year-old lady who presented with groin swelling of 2 months duration which did not subside with antibiotics. This case report may increase the awareness among the clinicians to consider melioidosis as a differential diagnosis in a patient presenting with lymphadenitis. Even though tubercular adenitis is the differential diagnosis for inguinal lymphadenopathy, melioidosis must be considered in patients with chronic lymphadenopathy, especially in those from melioidosis-endemic areas, who do not respond to the regular antibacterial therapy, which usually mimics cold abscess or tubercular adenitis.
Acknowledgments
We would like to thank Fr. Denis D’Sa, Administrator, FMMC, and Dr. B. Sanjeev Rai, Chief of Medical Services, Father Muller Charitable Institutions, for rendering whole-hearted support for all the research endeavors in our department..
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Hodgson K, Engler C, Govan B, Ketheesan N, Norton R. A comparison of routine bench and molecular diagnostic methods in the identification of Burkholderia pseudomallei”. J Clin Microbiol 2009;47:1578-80.
- Walsh AL, Wuthiekanun V. The laboratory diagnosis of melioidosis. Br J Biomed Sci 1996;53:249-53.
- Chlebicki MP, Tan BH. Six cases of suppurative lymphadenitis caused by Burkholderia pseudomallei infection TransR Soc Trop Med Hyg 2006;100:798-801.
- Whitmore A. An account of a glanders-like disease occurring in Rangoon. J Hyg (Lond) 1913;13:1-34.
- Stanton AT, Melioidosis FW. Studies from the Institute of Medical Research, Federated Malay States, 21. London: John Bale and Son and Danielson; 1932.
- Nandi T, Ong C, Singh AP, Boddey J, Atkins T, Sarkar-Tyson M, et al. A genomic survey of positive selection in Burkholderia pseudomallei provides insights into the evolution of accidental virulence. PLoS Pathog 2010;6:e1000845.
- Cheng AC, Currie BJ. Melioidosis: Epidemiology, pathophysiology, and management. Clin Microbiol Rev 2005;18:383-416.
- Loveleena, Chaudhry R, Dhawan B. Melioidosis; The remarkable imitator: Recent perspectives J Assoc Physicians India 2004;52:417-20.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.