Systemic Lupus Erythematosus Presenting as Acute Adrenal Insufficiency: A Rare Clinical Presentation
- *Corresponding Author:
- Dr. Riyaz Ahmad Bhat
House No. 2, Madina Bagh Chanapora, Srinagar - 190 009, Kashmir, India.
E-mail: bhatdrriaz@hotmail.com
Abstract
Systemic lupus erythematosus is a complex autoimmune disease with multisystem involvement with varied presentation. Autoimmune adrenal disease, on the other hand, can be associated with other autoimmune diseases. Adrenal insufficiency as a presenting feature of Systemic lupus erythematosus is a rare occurrence. We hereby report a case of a 20 year‑old female who presented to us in an acute hypoadrenal state and was found to have Systemic lupus erythematosus with renal involvement. Patient was successfully managed with steroids and improved clinically.
Keywords
Addison’s disease, Autoimmune diseases, Systemic lupus erythematosus
Introduction
Systemic lupus erythematosus (SLE) is the prototypic autoimmune disease characterized by the production of autoantibodies to components of the cell nucleus and is an association with diverse clinical manifestations encompassing almost all organ systems.[1] It is a complex disease characterized by remissions and flares and has variable presentation and course. Although 50% of patients with Addison’s disease have an associated autoimmune disease, its association with SLE has rarely been reported.[2] To our knowledge, SLE presenting as Addison’s disease is reported very rarely in literature. We hereby report such a case of SLE presenting as acute adrenal insufficiency.
Case Report
A 20-year-old female unmarried regularly menstruating presented to us with a history of anorexia, progressive darkening of the face and hands for the last 3 months and 4 days history of fever and vomiting. Patient also gave a history of periorbital puffiness and multiple joint pains for the last 2 months.
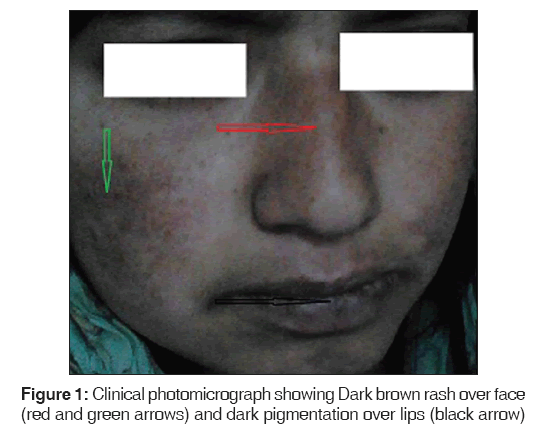
On examination, patient had pallor, puffiness of face, hyperpigmentation over face, nose and lips [Figure 1]. Vital examination revealed pulse rate of 90 beats/min and blood pressure of 90/60 mm Hg supine and 80/50 mm Hg standing. Rest of the general and systemic examination was unremarkable. Investigations revealed hemoglobin of 9.3 g/dl, Leukocyte count of 2200/mm3, Platelet count of 60,000/mm3. Kidney function tests, Liver function tests, serum calcium, and electrolytes were normal. Spot urine examination revealed pus cells of 2-3/high power field, no red blood cells and casts and albumin was ++. Chest X-ray showed right mid and lower zone infiltrates., 24 h urine examination showed 1.2 g of protein per day. Blood and urine cultures were sterile.
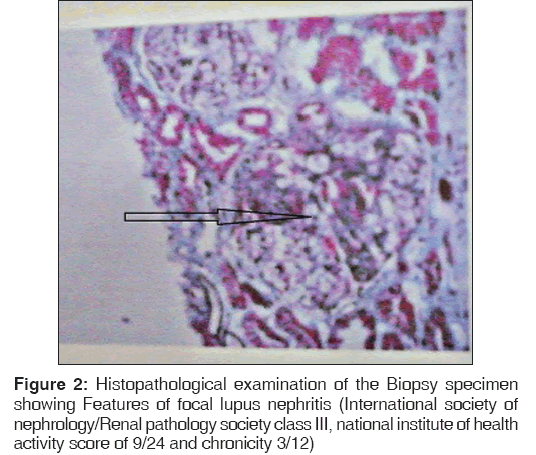
Patient was put on intravenous fluids and antibiotics were started empirically. Bone marrow examination performed in view of pancytopenia revealed hypercellular marrow with megaloblastoid and erythoid maturation with adequate iron stores. Antinuclear antibodies and antidouble stranded deoxyribonucleic acid (DNA) antibodies were positive. Patient was labeled as a case of SLE and renal biopsy was carried out in view of proteinuria. Histopathological examination of the biopsy tissue showed features consistent with focal lupus nephritis, International Society of Nephrology/Renal Pathology Society (ISN/RPS) class III, National Institute of Health (NIH) activity score of 9/24 and chronicity 3/12 [Figure 2]. Immunofluorescence showed immune deposit pattern suggestive of SLE. Echocardiography was normal. Patient continued to be in hypotension even on inotropic support and her clinical condition remained same. Based on clinical parameters, adrenal insufficiency was suspected. After taking 8 am sample for cortisol, patient was started on steroids. Serum antiadrenal antibody test showed results as 3 U/ml (normal range < 1 U/ml). Patient showed dramatic improvement in clinical parameters and hemodynamics. Morning cortisol levels were 7.5 μg/dl (normal range > 15 μg/ dl). A short synecthen test (SST) using 250 mcg synecthen carried out after stopping steroids showed 30 min value of 10 μg/dl and 60 min value of 12 μg/dl. Computed tomographic scan of the abdomen was normal. Thyroid function test was normal. Antithyroid peroxidase antibody levels were normal.
Patient was managed as a case of SLE with lupus nephritis with adrenal insufficiency and was discharged on steroids and hydroxychloroquine in a satisfactory clinical condition.
Discussion
SLE is an autoimmune disease in which organs and cells undergo damage initially mediated by tissue binding autoantibodies and immune complexes.[3] It has a varied systemic presentation. Primary adrenal insufficiency is most commonly caused by autoimmune adrenalitis. It can be associated with various diverse autoimmune conditions such as autoimmune thyroid disease, vitiligo, premature ovarian failure, type 1 diabetes and pernicious anemia.[4] The common presentation of acute adrenal insufficiency includes nausea, vomiting, vascular collapse, and abdominal pain.[5] Common presentation suggestive of chronic hypoarenal state includes progressive weakness, fatigue, poor appetite, and weight loss. Hyperpigmentation of the skin and mucous membranes often precedes all other symptoms by months to years. Uncommon associations include flaccid paralysis due to hyperkalemia, diarrhea, impotence, decreased libido, amenorrhea, and steatorrhea.[6]
Association of Addison’s disease with SLE has not been reported in the literature so far except in a few case reports.[7,8] The possible explanation for this association could be explained by a common autoimmune process, which is found in both clinical conditions. Alternatively, adrenal insufficiency could result from vasculitis induced by SLE per se.[9] Furthermore, SLE with antiphospholipid antibody syndrome can present as acute addisonian crisis due to acute adrenal hemorrhage.[10]
Kuster and Merlo reported a case of 44-year-old patient referred with weight loss of some 6 kg in 2 months, weakness and diarrhea. The patient had photodermatosis, nephropathy, and pancytopenia with positive antinuclear antibodies and antibodies against native DNA. Adrenal failure was diagnosed by hypernatremia, relapsing fever, and low baseline cortical and impaired response to adrenocorticotrophic hormone (ACTH) stimulation. The patient’s condition significantly improved under steroid therapy.[11] High index of suspicion is required in diagnosing adrenal insufficiency in SLE patients because clinical features of SLE may obscure signs of adrenal insufficiency.
Although, association of SLE with adrenal insufficiency has been reported in many reports, however, SLE presenting as acute adrenal insufficiency is very rarely reported. We report such a case of SLE presenting as acute adrenal insufficiency. The diagnosis of Addison’s disease in our patient was conclusively established on following grounds: (1) Clinical presentation (2) Inadequate response in SST (3) Positive results in antiadrenal antibody test (4) Dramatic response to steroids. The diagnosis of Lupus nephritis was firmly established on laboratory parameters and conclusively proven on renal biopsy. This patient was therefore managed as a case of SLE with Lupus Nephritis with Addison’s disease first time presenting as acute adrenal insufficiency. ACTH estimation was not carried out as all the parameters were in favor of Primary adrenal insufficiency with autoimmune etiology.
It is thus concluded that Addison’s disease in patients of SLE is a rare occurrence. Addison’s disease in SLE patients should be evaluated at presentation if clinical suspicion is high. However, high index of suspicion is required.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Rahman A, Isenberg DA. Systemic lupus erythematosus. N Engl J Med 2008;358:929-39.
- Stewart PM. The adrenal cortex. In: Kronenberg HM, Melmed S, Polonsky KS, Larsen PR, editors. Williams Textbook of Endocrinology. 11th ed. Saunders: An Imprint of Elsevier; 2008. p. 477-8.
- Hahn BH. Systemic lupus erythematosus. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J, editors. Harrison’s Principles of Internal Medicine. 18th ed. USA: Mc Graw-Hill Companies; 2012. P. 2724-35.
- Arlt W. Disease of the adrenal cortex. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J, editors. Harrison’s Principles of Internal Medicine. 18th ed. USA: Mc Graw-Hill Companies; 2012. P. 2940-61.
- White K, Arlt W. Adrenal crisis in treated Addison’s disease: A predictable but under-managed event. Eur J Endocrinol 2010;162:115-20.
- Guarini G, Macaluso M. Steatorrhoea in Addison's disease. Lancet 1963;1:955-6.
- Eichner HL, Schambelan M, Biglieri EG. Systemic lupus erythematosus with adrenal insufficiency. Am J Med 1973;55:700-5.
- Jakobsen AS, Cvitanich VB, Kirkegaard BC. Acute Addisonian crisis in a patient with systemic lupus erythematosus and secondary antiphospholipid syndrome. Ugeskr Laeger 2007;169:2224-5.
- Kuster GM, Merlo CM. An uncommon case of lupus. Schweiz Med Wochenschr 1999;129:961-5.
- Rigalleau V, Pommereau A, Martin L, Guérin V, Aparicio M. Unilateral adrenal hemorrhage in antiphospholipid syndrome associated with a lupus. Presse Med 1994;23:1092.
- Da Costa GM, Forga Llenas L, Martínez Bruna MS, Orta Martiartu M. Adrenal hemorrhage linked to systemic lupus erythematosus associated with the antiphospholipid syndrome. Rev Clin Esp 1992;191:54-5.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.