The Effect of Dental Operative Procedures on Peripheral Oxygen Saturation and Pulse Rate in Children in Benin- City, Nigeria
Citation: Ize-Iyamu IN, et al. The Effect of Dental Operative Procedures on Peripheral Oxygen Saturation and Pulse Rate in Children in Benin-City, Nigeria. Ann Med Health Sci Res. 2018;8:74-78
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Pulse oximeters are a non-invasive device useful in standardization of care in medical and dental offices for monitoring respiratory status during operative procedures. A close affiliation exists between the peripheral oxygen saturation (SpO2) and pulse rate which is affected by variables including exercise, traumatic events and operative procedures which may be encountered during standardized dental treatment. Aim: This study was carried out amongst 6-10-year-old children to evaluate the effect of dental operative procedures on peripheral oxygen saturation and pulse rate in Benin-City, Nigeria. Materials and methods: The peripheral oxygen saturation and pulse rate was assessed in 20 children each with a total number of 100 children. They were selected via a convenient sampling method for five procedures; 3 invasive (extraction, GIC filling and Pulpotomy) and 2 non-invasive (Fluoride therapy and scaling and polishing) procedures. The pulse oximeter was placed on the left index finger of each child at five different times: child in play room (PR1), child in the operatory (SR1), child on the dental chair before treatment (SR2), during treatment (SR3) and post treatment (PR2). The SpO2 level and pulse rate was then assessed at each time and recorded. Associations between frequencies were evaluated with the chi-square test. The Student’s t-test was used to compare means of the SpO2 and Pulse rate values. One way ANOVA was used for the values measured at different periods. Correlations between age, procedures and time were determined using the Statistical Package for Social Sciences (SPSS version 21) software. Significant values of P<0.05 were applied where applicable Results: The Mean age was 8.2 ± 0.7 years. There was a significant drop in the peripheral oxygen saturation (SpO2) levels for extractions and pulpotomy (mean range from 99% to 89% ± 1.6) respectively. Other procedures recorded a drop with a mean range from 99% to 96% ± 0.4 for GIC fillings and 99% to 94% ± 0.9 for scaling and polishing respectively during operative procedures (SR2). The SpO2 levels remained constant during topical fluoride therapy. The pulse rate increased sequentially for all procedures with its highest recorded value of 134bpm for scaling and polishing. There was also a significant increase in the pulse rate during operative dental procedures (SR2) for extractions, pulpotomies and scaling and polishing. Conclusion: Changes in SpO2 values occurred significantly during routine dental procedures in healthy young children with the critical values of less than 90% recorded during extractions and pulpotomies.
Keywords
Peripheral oxygen saturation; Dental operative procedures; Pulse rate
Introduction
Pulse oximetry is a non-invasive, indirect, continuous and cheap method of monitoring and evaluating the peripheral oxygen saturation in a clinical setting. [1] Operative dental procedures involving the child patient often involves fear and anxiety which may lower the oxygen saturation in the blood resulting in hypoxia. [2] It is essential that a method of assessment which is simple and easy to use encouraged in third world countries where dental awareness and utilization is still in its infancy [3-6] with many child patients exhibiting extreme fear and panic attacks. [2] Various methods of managing anxiety have been identified in paediatric dentistry, [2] and include reducing uncertainty, modeling, cognitive approaches, relaxation and systematic desensitization. While these methods rely on interaction with patient and practitioner, it does not give a quantitative evaluation of the effects of dental anxiety which may be a drop in the peripheral oxygen saturation. [5] This current study aimed to evaluate the effects of invasive and non-invasive treatment modalities on the peripheral oxygen saturation using a reproducible and standardized method.
The pulse oximeter works by placing a sensor device on the extremities or a thin part of the patient’s body, usually a finger, toe or earlobe. The device passes two wavelengths of light through the body part to a photodetector. [1,7-9] The sensor measures the amount of red and infrared light received by the detector and calculates the amount absorbed. [1,9] The arterial blood is the only light absorbing component due to its pulsating action over time and gives it an advantage over venous blood and other components of the body which includes bone, tissue, skin, muscle and fat. [1,7-9]
Blood oxygen saturation as measured by the pulse oximeter has been regarded as the fifth vital sign essential for efficient patient monitoring during medical and dental procedures [9] and would be of tremendous benefit in managing the anxious and uninformed child in our environment. [3,4,10] Studies have shown that children have an increased awareness of dental care in advanced countries with more patients seeking procedures for improved oral health. [2,3,8] Dental operative procedures are sometimes extensive with the administration of local anaesthetic agents which may cause stress with resultant anxiety and behavioural problems. [2,7,8] Clinical signs of anxiety include an increase in the heart rate and hyperventilation. [2] The process of inspiration and expiration of air between the atmosphere and the lungs is a vital process which makes oxygen available to cells and removes carbon dioxide from the lungs. Impairment of this process will cause a reduction in oxygen supplied to the tissues leading to the clinical condition of hypoxia [2,9,11] The benefits of pulse oximetry in healthy children has also been identified in studies, [1,7] to monitor cases of suffocation, choking, infections, such as pneumonia, drowning, inhaling poisonous chemicals, allergic reactions and in sleep apnoea. While this present study was carried out in a clinical setting, the findings may guide caregivers, teachers and others on monitoring the peripheral oxygen saturation with knowledge of baseline and acceptable values.
The benefit of this study in our environment would help put in place advanced and current trends in the management of the anxious child patient during operative procedures while using a cheap and readily available device for monitoring SpO2 values and pulse rate.
The purpose of this study was to evaluate the effect of dental operative procedures on peripheral oxygen saturation and pulse rate in Benin-City, Nigeria.
Methodology
This cross-sectional study was conducted in the Paediatric Dentistry Unit of the Department of Preventive Dentistry, University of Benin Teaching Hospital, Benin-City, Nigeria. The study participants consisted of a total number of 100 children aged 6-10-years who were brought to the clinic by their parents or guardians. Informed and written consent was obtained and the various procedures explained in detail to each participant and their parent or guardian before commencement. The study was approved by the Ethics and Research Committee of the University of Benin Teaching Hospital (Protocol number: ADM/E22/A/VOL VII/1266).
Five procedures, 3 invasive (Extraction, Glass Ionomer filling, Pulpotomy) and 2 non-invasive (Fluoride therapy, scaling and polishing) procedures were evaluated. For each of the procedures, 20 children were selected via a convenient sampling method and the parameters above assessed at five different times: child in play room (PR1), child in the dental operatory (SR1), child on the dental chair (SR2), during treatment (SR3) and post treatment (PR2).
Treatment commenced after an oral assessment and was not exclusive to only one dental arch and included treatment of deciduous and permanent teeth. The treatment was carried out at the same time each day (11am) by two paediatric dentists (PO and BM) and a maximum time of 45minutes spent from PR1 to PR2 irrespective of the procedure.
The oxygen saturation and pulse rate was assessed using the same Pulse oximeter CVS Pharmacy® and by the same dental nurse. The children were asked to sit in an upright but relaxed position and the index finger of the left hand inserted into the pulse oximeter until it made initial but gentle contact with the far end of the sensor and then switched on.
Precautions taken when using the pulse oximeter for each patient included:
• removal of external light interferences
• removal of nail polish and dyes from the left index finger
• removal of false fingernails
• ensuring that the sensor application is correctly placed (not too tight or too loose)
• Loosening of tight clothing or restraints on the left hand
Exclusion factors included:
• Patients with underlying medical conditions
• Patients with shivering from elevated temperatures or fear
• Patients with calloused fingers
• Patients below 6-years–of age and above 10-years-of age as at the last birthday
• Patients below 6-years–of age and above 10-years-of age as at the last birthday
• Patients on nerve blocking agents
• Patients with a negative Frankl score [11] as described below:
Frankl behavioural rating Scale 11 and Behavior
• Category 1 (- -) definitely negative - Child refuses treatment, cries forcefully, fearfully, or displays any agitated, overt evidence of extreme negativism. Combative, thrashing, verbal, unable to be restrained, need to terminate procedure.
• Category 2 (-) Negative - Reluctant to accept treatment and some evidence of negative attitude (not pronounced). Slightly combative, verbal, slightly agitated, able to be restrained and procedure safely completed
• Category 3 (+) Positive - The child accepts treatment but may be cautious. The child is willing to comply with the dentist, but may have some reservations. Quiet, not combative, cooperative, nonverbal.
• Category 4 (+ +) definitely positive - This child has a good rapport with the dentist and is interested in the dental procedures. Happy, helpful
For the invasive procedures, topical anaesthetic gel (20% Bencaine) was placed on the oral mucosa prior to the administration of injectable Local anesthesia (1.8 ml of Lidocaine hydrochloride 2% +adrenaline 1:80,000) solution.
Associations between frequencies were evaluated with the chisquare test.
The Student’s t-test was used to compare means of the SpO2 and Pulse rate values. One way ANOVA was used for the values measured at different periods. Correlations between age, procedures and time were determined using the Statistical Package for Social Sciences (SPSS version 21) software. Significant values of P<0.05 were applied where applicable
Results
A total of 100 children were seen, 20 for each of the procedures. Mean age for the children was 9.5 ± 0.7 years for extraction; 7.7 ± 0.6 years for GIC filling; 8.3 ± 0.6 years for pulpotomy; 7.0 ± 0.6 years for fluoride therapy and 8.4 ± 0.8 years for scaling and polishing.
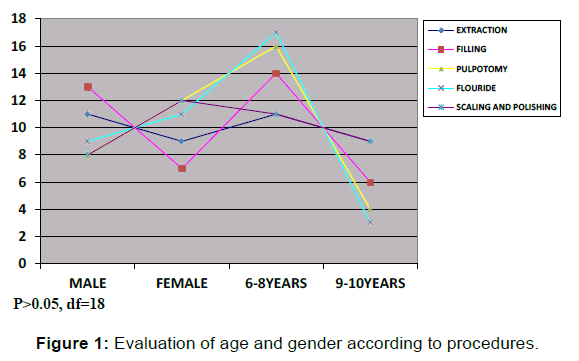
The various age groups identified were the 6-8-year-olds (n=69) and 9-10-year-olds (n=31). There were 49 male and 51 female respectively with the highest number of males, 13(26.5%) seen for fillings. The highest number of females were seen in 12(23.5%) for pulpotomies and scaling and polishing respectively. Figure 1 demonstrates the age and gender distribution according to procedure.
Figure 2 shows the application of a pulse oximeter on the left hand in a child.
Table 1 demonstrates the mean values for peripheral oxygen saturation (SpO2) for the different dental procedures in the waiting room (PR1), on the dental chair (SR1), during operative procedures (SR2), post operatively (SR3) and playroom (PR2). A highly significant drop in values were recorded, (P<0.05) for extractions and pulpotomies with the highest drop in values in SR2 (96.6 ± 0.48 and 95.8 ± 0.44). Values for SR3 were 96.8 ± 0.42 and 95.8 ± 0.44 respectively. There was also a significant change in PR1 irrespective of the procedure type.
| Procedures/ Location |
Extraction | Filling | Pulpotomies | Flouride Therapy | Scaling & Polishing | F-value | P-value |
|---|---|---|---|---|---|---|---|
| PR1 | 98.4 ± 0.11 | 97.9 ± 0.15 | 98.4 ± 0.13 | 98.2 ± 0.17 | 98.5 ± 0.14 | 2.790 | 0.031* |
| SR1 | 98.2 ± 0.17 | 98.1 ± 0.11 | 97.9 ± 0.23 | 98.3 ± 0.13 | 98.2 ± 0.19 | 0.779 | 0.541 |
| SR2 | 96.6 ± 0.48 | 97.9 ± 0.05 | 95.8 ± 0.44 | 98.3 ± 0.11 | 97.9 ± 0.26 | 11.290 | 0.000** |
| SR3 | 96.8 ± 0.42 | 98.0 ± 0.05 | 95.8 ± 0.44 | 98.3 ± 0.11 | 97.9 ± 0.26 | 13.202 | 0.000** |
| PR2 | 98.7 ± 0.15 | 98.1 ± 0.09 | 98.5 ± 0.14 | 98.3 ± 0.11 | 98.4 ± 0.25 | 2.360 | 0.019* |
| F-value | 9.735 | 0.595 | 22.088 | 0.173 | 1.759 | - | - |
| P-value | 0.000 | 0.667 | 0.000 | 0.952 | 0.143 | - | - |
Table 1: Peripheral oxygen saturation values, SpO2 for the different procedures in various locations.
Pulse rates for these procedures increased significantly in the operatory (SR2) during extraction and pulpotomy procedures (102.8 ± 6.4 and 104.0 ± 3.6 beats per minute respectively, Table 2). Significant changes were noted during the SR1 and PR2 periods for all procedures. The lowest value in the pulse rate was however noted in the PR1 period.
| Procedures | Extraction | Filling | Pulpotomies | Flouride Therapy | Scaling & Polishing | F-value | P-value |
|---|---|---|---|---|---|---|---|
| PR1 | 84.9 ± 2.45 | 84.1 ± 2.02 | 90.4 ± 2.37 | 83.8 ± 2.52 | 83.8 ± 2.83 | 2.243 | 0.070 |
| SR1 | 89.1b ± 3.07 | 83.45 ± 2.60 | 98.2 ± 2.15 | 86.3 ± 2.73 | 92.5 ± 2.67 | 4.629 | 0.002** |
| SR2 | 102.8 ± 6.41 | 89.9 ± 3.03 | 103.9 ± 3.60 | 91.2 ± 3.24 | 134.7 ± 41.68 | 0.900 | 0.467 |
| SR3 | 95.2 ± 4.29 | 90.5 ± 2.55 | 101.6 ± 3.21 | 91.9 ± 2.84 | 94.2 ± 2.87 | 1.769 | 0.141 |
| PR2 | 88.3 ± 2.97 | 85.8 ± 2.12 | 93.5 ± 2.30 | 88.8 ± 2.25 | 89.8 ± 2.84 | 1.235 | 0.029* |
| F-value | 2.973 | 1.723 | 4.051 | 0.173 | 0.362 | - | - |
| P-value | 0.023 | 0.151 | 0.004 | 0.193 | 0.835 | - | - |
Table 2: Pulse rate values for the different procedures at various locations.
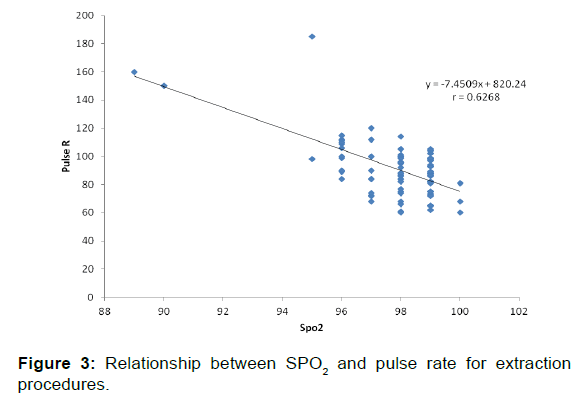
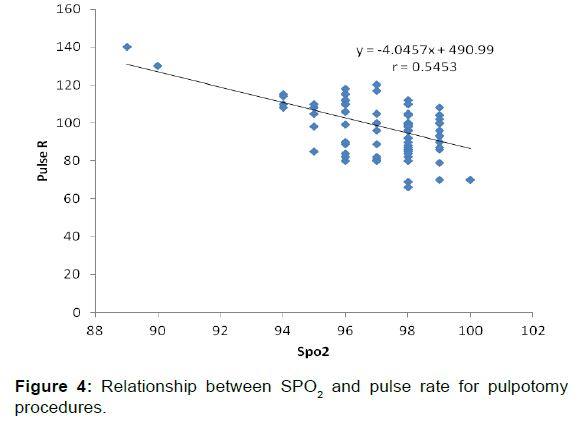
The relationship between SpO2 and pulse rate for various procedures were very weakly correlated for fillings and fluoride therapy (r=-0.2922 and r=+0.1026) respectively. Figures 3 and 4 shows scatter plots with the strongest negative correlations of r=-0.6268 for extractions and r=-0.5453 for pulpotomies respectively.
Discussion
Diagnostic, restorative, surgical and preventive treatments are invasive and non invasive options available in the management of the child patient. [5,11] These have been shown to evoke dental anxiety which may lead to hypoxia and a resultant drop in SpO2 levels. [1,2] This current study showed 3 invasive (extraction, GIC filling and Pulpotomy) and 2 non-invasive (Fluoride therapy and scaling and polishing) procedures with a higher number of male children within the 6-8-year-old age range undergoing extractions and fillings. Also identified were a higher number of females within this same age range for pulpotomies, fluoride therapy and scaling and polishing.
This current study identifies procedures for all treatment options in 6-10-year-olds. Studies have shown that the highest percentage of children seeking dental care is within this age range, [3-5,11-13] which is in conformity with this present study. A survey of the demographic characteristics of children attending clinic identified more male than female children within this age range, [12] which is at variance with this study. Other studies showed an almost equal gender ratio with more females than males which are in agreement with this current study. [6,10]
Studies that measure the SpO2 and pulse rate during routine dental treatment are not common. [1,14] This study showed a drop in the peripheral oxygen value for extractions and pulpotomies with the child on the dental chair (SR2), and during treatment (SR3). Studies have identified dental anxiety in the child patient [2,14] as being associated with fear while sitting on the dental chair which compared favourably with the results of this current study. This could explain the drop in oxygen saturation with resultant hypoxia. [1,2] Studies have shown that certain dental procedures induce hypoxia [7-8,14] which is in agreement with this present study.
Rayen et al. [14] reported that SpO2 did not change considerably before or during routine dental treatment. This does not agree with the findings from this study where there was a significant drop in SpO2 values for extractions and pulpotomies. Normal SpO2 values range between 95%- 98%. [1,7-9] It has been recommended that SpO2 values below 90% require administration of oxygen. [1,14-16] In this current study, none of the children recorded values of less than 95% in all the procedures carried out at different time periods.
An increase in the pulse rates of the children in this current study recorded more significant changes for extractions and pulpotomy procedures. This is in disagreement with other studies [14] where there was a significant decrease in the pulse rate. Some authors have reported an increase in pulse rate during dental procedures [17-19] which is in agreement with this current study, while others have reported a constant pulse rate during dental procedures. [20] Dental anxiety which may be the reason for the increase in pulse rate in this study has been identified to be more prominent in patients with a low level of awareness, knowledge and utilization of dental services especially in our environment. [2-4,13]
Our study showed a strong correlation between SpO2 values and the various dental procedures with extractions and pulpotomies having a negative effect on the oxygen saturation. This is in agreement with studies [1,2,9,14-18] where dental procedures like extractions and restorative procedures like pulpotomies could have a negative effect on the child. This could manifest as hypoxia with the resultant increase in pulse rate and drop in the SpO2 value. [1,7-9,14-18]
Conclusion
The pulse oximeter is a simple method of measuring SpO2 and pulse rate in healthy children as restorative (pulpotomies) and surgical treatments (extraction) have been shown to evoke dental anxiety which may lead to hypoxia and a resultant drop in SPO2 levels in healthy children. These procedures could also lead to an increase in the pulse rate which could have adverse effects in children who have underlying cardiac conditions. Efforts at reducing anxiety levels in these children cannot be over emphasized.
Pulse oximeters should be made available in all dental clinics in our environment to monitor the SpO2 values of the child patient before, during and after invasive procedures. Behaviour management techniques should be utilized judiciously in managing children in the dental clinic to reduce anxiety.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Fukayama H, Yagiela JA. Monitoring of vital signs during dental care. Int Dent J. 2006; 56: 102-108.
- Shah PP, Patne SY, Patil LS, Patil SS. Dental anxiety in child patients: A review. UJMDS 2014; 02: 161-162.
- Sofola OO. Implications of low oral health awareness in Nigeria. Niger Med J 2010; 51: 131-133.
- Sofola OO, Agbelusi GA, Jeboda SO. Oral health knowledge, attitudes and practices of primary school teacher in Lagos State. Nig J Med 2002; 11: 73-76.
- Akpata ES. The prevalence and distribution of dental caries and gingivitis in the primary dentitions of 6-year old Lagos children. J Int Ass Dent Child 1979; 10: 3-9.
- Kubota K, Yonemitsu M, Hollist NO, Ono Y, Nakata M, Ajayi-Obe SO, et al. AI: Five-year follow-up caries study among Nigerian children. Community Dent Oral Epidemiol 1990; 18: 197-199.
- Rohlfing GK, Dilley DC, Lucas WJ, William FV. The effect of supplemental oxygen saturation on apnoea and oxygen saturation during pediatric conscious sedation. Padiatric Dentistry 1998; 20; 8-16.
- Goodday RHB, Crocker DA. The effect of rubber dam placement on the arterial oxygen saturation in dental patients. Operative Dentistry 2006; 31: 176-179.
- Sapira JD. The art and science of bedside diagnosis. 1st edition, Baltimore; Williams and Wilkins 1990; 139: 85-104.
- Folayan MO, Oziegbe E, Oyedele T, Ola D. Factors limiting dental service utilization by pupils in Ile-Ife, Nigeria. Niger J Health Sci 2013; 2: 18-23.
- Wright GZ, Stigers JI. Nonpharmacologic management of children’s behaviors. In: Dean JA, Avery DR, McDonald RE, eds. McDonald and Avery’s Dentistry for the Child and Adolescent. 9th ed. Maryland Heights, Mo: Mosby-Elsevier; 2011: 27-40.
- Sanu OO, Oredugba FA, Adeboa RA. Oral and dental diseases among children and adolescents in Kano, Nigeria. Pesq Bras Odontoped Clin Integr, João Pessoa 2010; 10: 445-450.
- Folayan OF, Chukwumah NM, Onyejaka N, Adeniyi AA, Olatosi OO. Appraisal of the national response to the caries epidemic in children in Nigeria. BMC Oral Health 2014; 14: 1-10.
- Rayen R, Muthu MS, Chandrasekhar RR, Sivakumar N. Evaluation of physiological and behavioral measures in relation to dental anxiety during sequential dental visits in children. Indian J Dent Res 2006; 17: 27-34
- Dutra RM, Neves IL, Neves RS, Atik E, Santos UP. Peripheral oxygen saturation, heart rate, and blood pressure during dental treatment of children with cyanotic congenital heart disease. Clinics 2014; 69: 314-318.
- Shirakawa T, Noe Y, Oikawa T, Shinoguchi K, Oguchi H. Pulse oximetry for noninvasive oxygen monitoring during dental treatment in children with congenital heart disease. Shoni Shikagaku Zasshi 1990; 28: 1056- 1065.
- Folayan MO, Idehen EE, Ufomata D. The effect of sociodemographic factors on dental anxiety in children seen in a suburban Nigerian Hospital. Int J Ped Dent 2003; 13: 20-26.
- Messer JG. Stress in dental patients undergoing routine procedures, J Dent Res 1977; 56: 362-367.
- Sowjanya V, Tandon S, Tharian E. Physiological response to dental anxiety in children. J Indian Soc Prev Dent 1995; 13: 13-17.
- Emara MM, Yamany HA, Awad S, Elshazly, Shamaa A. Do dental procedures affect lung function and arterial oxygen saturation in asthmatic patients. Egyptian Journal of Chest Diseases and Tuberculosis 2013; 62: 207-214.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.