Transperineal vs. Transrectal Approach for Prevention of Infectious Complications after Prostate Biopsy: Systematic Review and Meta-Analysis
Published: 20-Sep-2024
Citation: Aldoukhi MT, et al. Transperineal vs. Transrectal Approach for Prevention of Infectious Complications after Prostate Biopsy: Systematic Review and Meta-Analysis. Ann Med Health Sci Res. 2021;11:33-38
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: In patients suspicious of prostate cancer, a prostate biopsy should be done. Biopsies are viable either via the transrectal or transperineal routes. As compared with the Transrectal Prostate Biopsy (TRPBx), Transperineal Prostate Biopsy (TPPBx) gives a non-inferior most cancers detection price. Aim: This work aims to determine the safety of the Transperineal (TP) vs. Transrectal (TR) Approach for the prevention of infectious complications after prostate biopsy. Materials and Methods: A systematic search was performed over different medical databases to identify Urology studies, which studied the outcome of the TP group versus the TR group of prostate biopsy patients. Using the meta-analysis process, either with fixed or random-effects models, we conducted a meta-analysis on the rate of infectious complications as a primary outcome (including fever, urinary tract infections, and sepsis), and urine retention and hematuria as secondary outcomes. Results: Seven studies were identified involving 1242 patients, 642 in the TP group and 654 in the TR group. The meta-analysis process revealed a highly significant decrease in the rate of infectious complications in the TP group compared to the TR group (p<0.01). Also, there was a non-significant difference in the rate of urine retention and hematuria in the TP group compared to the TR group (p>0.05 respectively). Conclusion: To conclude, our study indicated that transperineal prostate biopsy has the same diagnostic accuracy as a transrectal prostate biopsy; however, a transperineal prostate biopsy is safer and more valuable because it poses a significantly lower risk of infection and rectal bleeding. Despite the increased risk of pain after TP biopsy, we recommend that doctors should perform a transperineal prostate biopsy if possible.
Keywords
Transperineal; Transrectal approach; Infections; Prostate biopsy
Introduction
Worldwide, prostate cancer accounts for a substantial percentage of males’ most cancers and mortality. Prostate cancer prognosis is based on biopsies following patient evaluation for an elevated prostate-specific antigen or ordinary digital rectal exam and there is an increasing role for pre-biopsy MRI. Prostatic biopsy remains the keystone for prognosis and control of prostate most cancers and the maximum usually achieved diagnostic system in urology with more than 2 million per year. [1]
Two approaches can be used to area fiducial markers into the prostate. One is the transrectal approach, and the other is the transperineal method. In prostate biopsy examinations, the transrectal technique results in a better frequency of foremost headaches, whereas the transperineal method is greater complicated and painful. However, the utility of these two methods for fiducially marker placement has no longer been clarified but. Consequently, the cause of this study became to compare the feasibility of transrectal and transperineal VISICOIL placement before proton therapy for prostate cancer. [2]
Transperineal (TP) prostate biopsies are a widespread and well-documented approach to analyze prostate most cancers. TP biopsies have widespread blessings over the conventional Transrectal (TR) method, which includes reduced rates of sepsis and being better able to sample the anterior prostate. [3]
The systematic TR prostate biopsy, which’s the gold popular for the detection of PCa, has been performed for decades internationally. This method, but, reportedly underestimates PCa incidence with a false negative rate of as much as 49%. Additionally, TR prostate biopsy has been mentioned to purpose excessive complications along with rectal bleeding, fever, sepsis, hematuria, and acute urinary retention. [4]
In patients suspicious of prostate cancer, a prostate biopsy should be done. Biopsies are viable either via the transrectal or transperineal routes. as compared with the Transrectal Prostate Biopsy (TRPBx), Transperineal Prostate Biopsy (TPPBx) gives a non-inferior most Cancers Detection Price (CDR), especially in patient’s present process re-biopsy for consistently improved PSA and in instances of Active Surveillance (AS), in which TPPBx seems to be advanced. Furthermore, the transperineal route achieves advanced sampling of the anterior and apical regions, particularly after preceding multiple poor TRPBx. Infectious headaches are nullified due to avoidance of needle passage through the rectal mucosa, and there’s a particularly significant proof of reduced fever and sepsis quotes while as compared with TRPBx, with preserving acceptable urinary retention rates. [5]
This work aims to determine the safety of the Transperineal vs. Transrectal Approach for the prevention of infectious complications after prostate biopsy.
Materials and Methods
Our review came following the (PRISMA) statement guidelines. [6]
Study eligibility
The included studies should be in English, a journal published article, and a human study describing prostate biopsy patients. The excluded studies were non-English or animal studies or describing other urological procedures.
Study identification
Basic searching was done over the PubMed, Cochrane library, and Google scholar using the following keywords: transperineal, transrectal approach, infections, prostate biopsy.
Data extraction and synthesis
RCTs, clinical trials, and comparative studies, which studied the outcome of the TP group vs. TR group of prostate biopsy patients, will be reviewed. Outcome measures included the rate of infectious complications as a primary outcome (including fever, urinary tract infections, and sepsis), and urine retention and hematuria as secondary outcomes.
Study selection
We found 150 records, 90 excluded because of the title; 60 articles are searched for eligibility by full-text review; 22 articles cannot be accessed; 13 studies were reviews and case reports; 11 were not describing functional outcome; the desired procedure not used in 7 studies leaving 7 studies that met all inclusion criteria.
Statistical analysis
Pooled Odds Ratios (OR), proportions (%), with 95% Confidence Intervals (CI) assessed, using a statistical package (MedCalc, Belgium). The meta-analysis process was established via I2- statistics (either the fixed-effects model or the random-effects model), according to the Q test for heterogeneity.
Results
The included studies were published between 2008 and 2020 [Table 1]. Regarding patients’ characteristics, the total number of patients in all the included studies was 1242 patients, 642 in the TP group and 654 in the TR group [Table 1]. The mean age of all patients was (67.5 years) [Table 1].
| N | Author | Total | Number of patients TP group |
TR group | Age (average years) |
|---|---|---|---|---|---|
| 1 | Hara et al., 2008 | 246 | 126 | 120 | 71 |
| 2 | Takenaka et al., 2008 | 200 | 100 | 100 | 71.5 |
| 3 | Cerruto et al., 2014 | 54 | 54 | 54 | 66.5 |
| 4 | Di Franco et al., 2017 | 257 | 125 | 132 | 67 |
| 5 | Huang et al., 2019 | 238 | 130 | 108 | 66.6 |
| 6 | Wegelin et al., 2019 | 157 | 79 | 78 | 64.7 |
| 7 | Roberts et al., 2020 | 90 | 28 | 62 | 65.1 |
Table 1: Patients and study characteristics.
A meta-analysis study was done on 7 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=1242) [Table 2].
| N | Author | Primary outcome Rate of infectious complications | Secondary outcome Rate of urine retention | Rate of hematuria | |||
|---|---|---|---|---|---|---|---|
| TP group | TR group | TP group | TR group | TP group | TR group | ||
| 1 | Hara et al., 2008 | 0 | 2 | 2 | 3 | 13 | 11 |
| 2 | Takenaka et al., 2008 | 1 | 2 | 2 | 3 | 11 | 12 |
| 3 | Cerruto et al., 2014 | 0 | 1 | 0 | 1 | 5 | 0 |
| 4 | Di Franco et al., 2017 | 0 | 3 | 2 | 3 | 3 | 3 |
| 5 | Huang et al., 2019 | 3 | 27 | 4 | 9 | 7 | 15 |
| 6 | Wegelin et al., 2019 | 3 | 9 | --- | --- | --- | --- |
| 7 | Roberts et al., 2020 | 5 | 38 | 27 | 36 | 6 | 3 |
Table 2: Summary of outcome measures in all studies.
Each outcome was measured by: Odds Ratio (OR), for the rate of infectious complications, for the rate of urine retention, for the rate of hematuria, concerning the primary outcome measure.
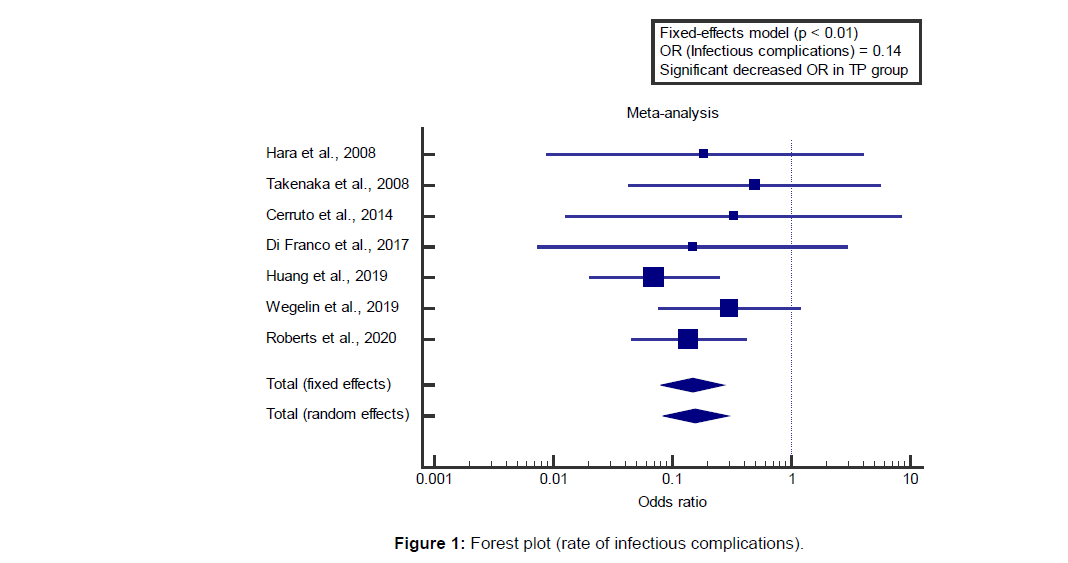
We found 7 studies reported the rate of infectious complications. I2 (inconsistency) was 0%, Q test for heterogeneity (p>0.05), so fixed-effects model was carried out; with overall OR=0.14 (95% CI=0.0797 to 0.273).[7-13]
Using the fixed-effects model, the meta-analysis process revealed a highly significant decrease in the rate of infectious complications in the TP group compared to the TR group (p<0.01) [Figure 1].
Concerning the secondary outcome measures,
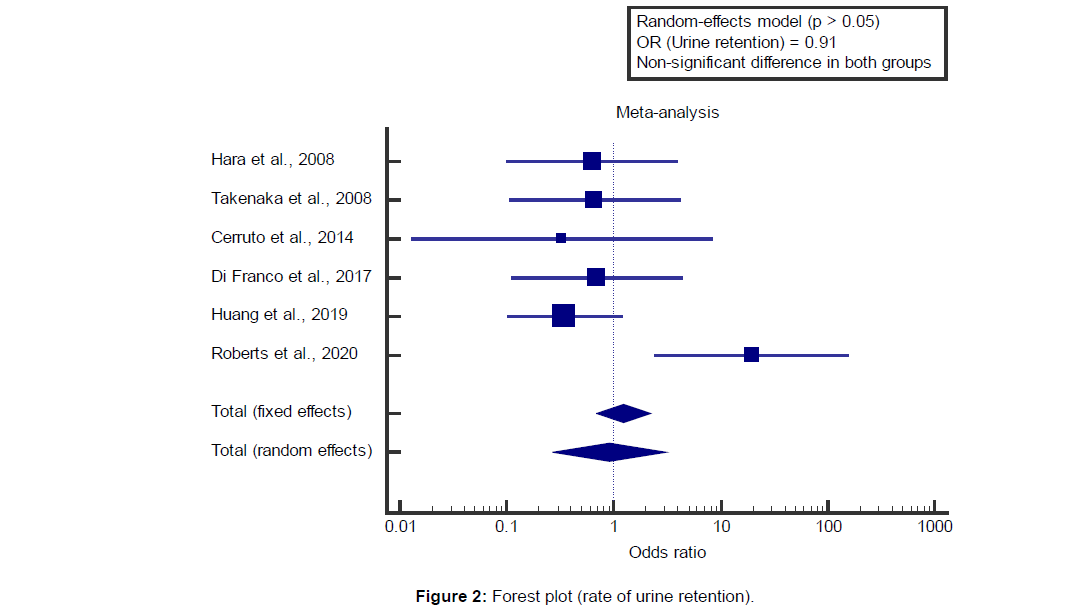
We found 6 studies that reported a rate of urine retention.
I2 (inconsistency) was 61.7%, Q test for heterogeneity (p=0.022), so random-effects model was carried out; with overall OR=0.914 (95% CI=0.268 to 3.118).
Using the random-effects model, the meta-analysis process revealed a non-significant difference in the rate of urine retention in the TP group compared to the TR group (p>0.05) [Figure 2].
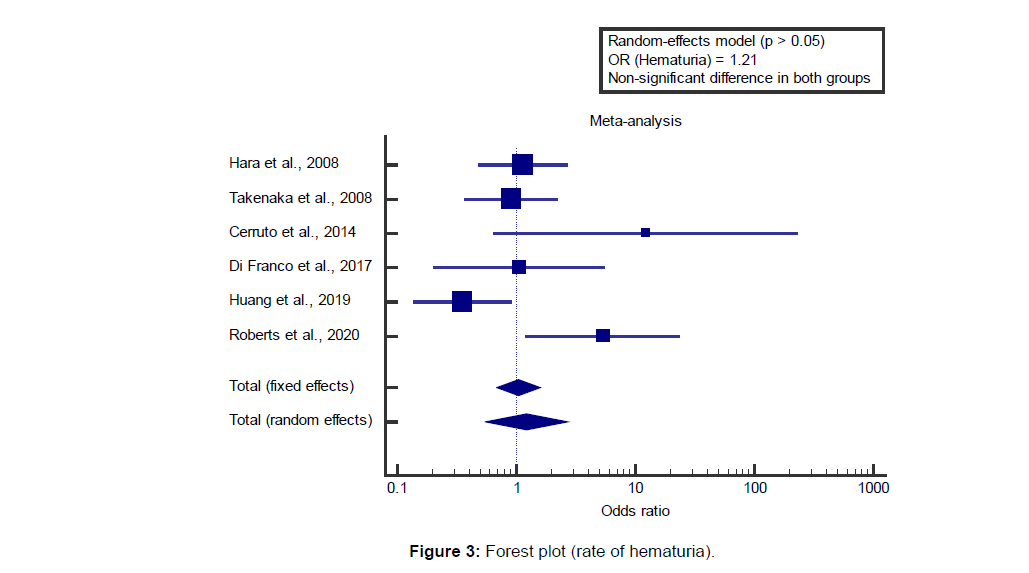
We found 6 studies reported a rate of hematuria.
I2 (inconsistency) was 60.8%, Q test for heterogeneity (p=0.025), so random-effects model was carried out; with overall OR=1.21 (95% CI=0.547 to 2.680).
Using the random-effects model, the meta-analysis process revealed a non-significant difference in the rate of hematuria in the TP group compared to the TR group (p>0.05) [Figure 3].
Discussion
This work aims to determine the safety of the transperineal vs. transrectal Approach for the prevention of infectious complications after prostate biopsy.
The included studies were published between 2008 and 2020. Regarding patients’ characteristics, the total number of patients in all the included studies was 1242 patients, 642 in the TP group and 654 in the TR group. The mean age of all patients was (67.5 years).
A meta-analysis study was done on 7 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=1242).
Concerning the primary outcome measure, we found 7 studies reported a rate of infectious complications.
Using the fixed-effects model, the meta-analysis process revealed a highly significant decrease in the rate of infectious complications in the TP group compared to the TR group (p<0.01), which came in agreement with Pradere et al., [1] Starmer et al., [3] Wenzel et al., [14] Ohta et al., [2] Xiang et al., [4] Mian et al. [15] and Steinberg et al. [16]
Pradere et al., reported that meta-analysis based on 7 RCTs confirmed this important aspect and confirmed an extensive decrease in the infection rate the usage of the transperineal direction (RR=0.55). Despite the potential logistic challenges attached to the giant introduction of the local anesthetic transperineal technique, our findings support the “TREXIT 2020” method to desert transrectal prostate biopsy. [1]
Starmer et al. reported that, the hazard of sepsis from nearby anesthetic (Los Angeles) TP biopsy techniques zero. [2] Information from a worldwide prevalence take a look at of infections in urology showed 3.5% of patients undergoing TR biopsy had febrile Urinary Tract Contamination (UTI) with 3.1% requiring hospital admission. [3]
Wenzel et al. reported that prostate most cancers, the maximum common cancer in men international, is diagnosed with prostate biopsies. Currently, exclusive relevant biopsy procedures are to be had a transrectal and transperineal approach. Several studies mentioned that cancer detection quotes through systematic biopsies are comparable among each process. But, concerning infectious fees, some research recommends that the transperineal approach is related to lower rates of infectious complications. [14]
Ohta et al. reported that, in a study of biopsy procedures, the transperineal approach was reported to be safer than the transrectal approach, based on the frequency of major complications, such as infection and bleeding. [2]
Xiang et al. reported that the TR technique still had an extensively higher risk of contamination than the TP technique. For patients who’re vulnerable to contamination which includes people with diabetes, prostatitis, and urinary catheterization, the transperineal prostate biopsy turned into encouraged to avoid sepsis and severe fever after the procedure. [4]
Mian et al. reported that, due to the increasing issues over infections, there may be renewed interest in the use of the TPBx approach in all men to avoid rectal wall puncture and inoculation of the urinary tract with enteric bacteria. numerous observational studies inspecting the consequences of TPBx, using diverse antibiotic regimens, have reported publish-biopsy infections and/or hospitalization rates at <1%. [15]
Steinberg et al. reported that Men experiencing an infectious complication were more likely to have their biopsy performed in an outpatient hospital (26% vs. 15% no infection, p<0.001), reside in non-urban areas (18% vs. 15% no infection, p<0.001), and have a diagnosis of diabetes (18% vs. 16% no infection, p<0.01). Men who had a transperineal prostate biopsy had a decreased risk of infection (5.4% vs. 6.2% transrectal approach, p<0.001). [16]
Concerning the secondary outcome measures, we found 6 studies reported a rate of urine retention. Using the randomeffects model, the meta-analysis process revealed a nonsignificant difference in the rate of urine retention in the TP group compared to the TR group (p>0.05), which came in agreement with Günzel et al. [17] and Ohta et al. [2]
Günzel et al. reported that Gross haematuria became the most common postoperative difficulty (51%). One affected person developed a bladder tamponade and required a transurethral catheter with irrigation. In all other instances, hematuria ceased spontaneously in the first days after the biopsy. As compared with the problem rates of transrectal prostate biopsies comparable complication quotes are found for microhematuria. [17]
Ohta et al. reported that there were no major complications, such as sepsis, uncontrollable bleeding, or urinary retention, in either group. Marker migration was observed in 3 of 524 markers (0.6%) in the transrectal group and 2 of 182 markers (1.1%) in the transperineal group (P>0.05). [2]
Our study came in disagreement with Starmer et al. [3] Starmer et al. reported that there have been concerns regarding increased risks of Acute Urinary Retention (AUR) after TP prostate biopsy as demonstrated in the prostate imaging compared to transperineal ultrasound-guided biopsy for significant Prostate Cancer Risk Evaluation (PICTURE) study with risk of AUR at 24%. [3]
We found 6 studies reported a rate of hematuria. Using the random-effects model, the meta-analysis process revealed a nonsignificant difference in the rate of hematuria in the TP group compared to the TR group (p>0.05), which came in agreement with Günzel et al. [17] and Xiang et al. [4]
Günzel et al. reported that gross haematuria was the most frequent postoperative complication (51%). One patient developed a bladder tamponade and required a transurethral catheter with irrigation. In all other cases, hematuria ceased spontaneously in the first days after the biopsy. Compared with the complication rates of transrectal prostate biopsies similar complication rates are found for dysuria and acute urinary retention. [17]
Xiang et al. reported that the TP approach significantly protected the patients from rectal bleeding (RR=0.02) and fever (RR=0.26); however, the TP approach significantly increased patient pain (RR=1.83). No significant difference was found in the acute retention of urine and hematuria between the two approaches. [4]
Conclusion
To conclude, our study indicated that transperineal prostate biopsy has the same diagnostic accuracy as a transrectal prostate biopsy; however, a transperineal prostate biopsy is safer and more valuable because it poses a significantly lower risk of infection and rectal bleeding. Despite the increased risk of pain after TP biopsy, we recommend that doctors should perform a transperineal prostate biopsy if possible
Authorship
All the listed authors contributed significantly to the conception and design of study, acquisition, analysis, and interpretation of data and drafting of the manuscript, to justify authorship.
References
- Pradere B, Veeratterapillay R, Dimitropoulos K, Yuan Y, Omar MI, MacLennan S, et al. Nonantibiotic strategies for the prevention of infectious complications following prostate biopsy: A systematic review and meta-analysis. J Urol. 2021;205:653–663.
- Ohta K, Ogino H, Iwata H, Hashimoto S, Hattori Y, Nakajima K, et al. Feasibility of transrectal and transperineal fiducial marker placement for prostate cancer before proton therapy. Jpn J Clin Oncol. 2021;51:258–263.
- Starmer B, Iordan N, McCabe J. Comparing tolerability of local anaesthetic transperineal and transrectal prostate biopsies. J Clin Urol. 2021.
- Xiang J, Yan H, Li J, Wang X, Chen H, Zheng X. Transperineal vs. transrectal prostate biopsy in the diagnosis of prostate cancer: A systematic review and meta-analysis. World J Surg Oncol. 2019;17:1–11.
- Ortner G, Tzanaki E, Rai BP, Nagele U, Tokas T. Transperineal prostate biopsy: The modern gold standard to prostate cancer diagnosis. Turk J Urol. 2021;47:S19.
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. Bmj. 2009;339.
- Hara R, Jo Y, Fujii T, Kondo N, Yokoyoma T, Miyaji Y, et al. Optimal approach for prostate cancer detection as initial biopsy: Prospective randomized study comparing transperineal vs. transrectal systematic 12-core biopsy. Urology. 2008;71:191–195.
- Takenaka A, Hara R, Ishimura T, Fujii T, Jo Y, Nagai A, et al. A prospective randomized comparison of diagnostic efficacy between transperineal and transrectal 12-core prostate biopsy. Prostate Cancer Prostatic Dis. 2008;11:134–138.
- Cerruto MA, Vianello F, D’Elia C, Artibani W, Novella G. Transrectal vs. transperineal 14-core prostate biopsy in detection of prostate cancer: A comparative evaluation at the same institution. Archivio Italiano Di Urologia e Andrologia. 2014;86:284–287.
- Di Franco CA, Jallous H, Porru D, Giliberto GL, Cebrelli T, Tinelli C, et al. A retrospective comparison between transrectal and transperineal prostate biopsy in the detection of prostate cancer. ArchivioItaliano Di Urologia e Andrologia. 2017;89:55–59.
- Huang GL, Kang CH, Lee WC, Chiang PH. Comparisons of cancer detection rate and complications between transrectal and transperineal prostate biopsy approaches: A single center preliminary study. BMC Urology 2019;19:1–8.
- Wegelin O, Exterkate L, van der Leest M, Kummer JA, Vreuls W, De Bruin PC, et al. The FUTURE trial: A multicenter randomised controlled trial on target biopsy techniques based on magnetic resonance imaging in the diagnosis of prostate cancer in patients with prior negative biopsies. European Urology. 2019;75:582–590.
- Roberts MJ, Macdonald A, Ranasinghe S, Bennett H, Teloken PE, Harris P, et al. Transrectal vs. transperineal prostate biopsy under intravenous anaesthesia: A clinical, microbiological and cost analysis of 2048 cases over 11 years at a tertiary institution. Prostate Cancer and Prostatic Dis. 2020:1–8.
- Wenzel M, Von Hardenberg J, Welte MN, Doryumu S, Hoeh B, Wittler C, et al. Monoprophylaxis with cephalosporins for transrectal prostate biopsy after the fluoroquinolone- era: A multi-institutional comparison of severe infectious complications. Front Oncol. 2021;11:2139.
- Mian BM, Kaufman RP, Fisher HA. Rationale and protocol for randomized study of transrectal and transperineal prostate biopsy efficacy and complications (ProBE-PC study). Prostate Cancer and Prostatic Dis.2021:1–9.
- Steinberg RS, Kipling L, Bens KB, Patil D, Henry M, Mehta A, et al. Enhanced antibiotic prophylaxis and infection- related complications following prostate biopsy. World J Urol.2021:1-8.
- Günzel K, Magheli A, Baco E, Cash H, Heinrich S, Neubert H, et al. Infection rate and complications after 621 transperineal MRI-TRUS fusion biopsies in local anesthesia without standard antibiotic prophylaxis. World J Urol. 2021:1–6.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.