Tuberculous Choroidal Granuloma in Immunocompetent South African Indians: A Case Series
Citation: Visser L, et al. Tuberculous Choroidal Granuloma in Immunocompetent South African Indians: A Case Series. Ann Med Health Sci Res. 2021;11:1309-1314.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Purpose: To report cases of tuberculous choroidal granuloma in retroviral negative South African Indians with no obvious systemic illness with a view to emphasizing the need for high clinical index of suspicion in the management of patients in tuberculosis endemic areas. Methods: This is a case report. Patients: Ophthalmic patients referred from a Provincial Eye Hospital for complaints of poor vision and subretinal lesions. Results: A presumptive diagnosis of tuberculous (TB) choroidal granuloma was made in both cases based a high index of suspicion. Both cases responded positively to empirical treatments with antituberculosis medications. Discussion/Conclusion: Tuberculous choroidal granuloma usually occurs following a systemic spread to the choroid. In the absence of systemic signs/symptoms and negative laboratory investigations, a positive response to anti TB medication is confirmatory. A high index of suspicion is needed in TB endemic areas.
Keywords
Choroid; Granuloma; Tuberculosis; Indians
Introduction
Ocular tuberculosis in immunosuppressed individuals or HIV patients with systemic or miliary tuberculosis (TB) is not surprising especially in the developing countries with a high burden of TB and human immunodeficiency virus (HIV). However, ocular TB in HIV negative patients without TB or previous TB contacts is rare. We report two cases of TB choroidal granuloma without a history of HIV, TB or contacts with a known TB patient.
Case one
A 57- year old Indian lady was referred from a Provincial Hospital for a one- month history of pain, redness and deterioration of vision in the left eye. She had no significant past medical history, no family history of malignancies or similar symptoms. There were no significant findings on general examination including a breast examination. She was HIV negative, did not have tuberculosis (TB) and had no previous tuberculosis contacts.
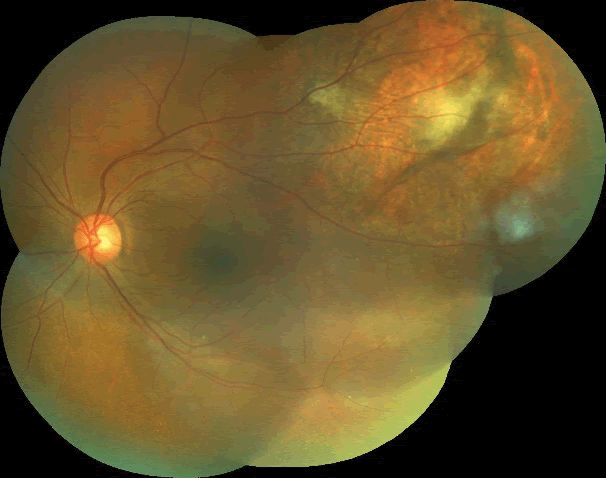
Ocular examination revealed a visual acuity of 0.7 on the right eye aided with pin hole to 0.8 and 0.7 on the left eye which worsened with pin hole to 0.5. The only significant findings on the right eye was an early nuclear sclerosis. The left eye examination revealed trace cells in the anterior chamber, early nuclear sclerosis, 1+ vitreous cells, 26mmHg intraocular pressure (Left eye was 17mmHg). Fundal examination showed a large choroidal lesion, creamy in colour with leopard like edges along the superior temporal arcade with an associated exudative retinal detachment below the inferotemporal arcade and choroidal folds [Figures 1a and1b].
The exudative retinal detachment was worse in the supine position (shifting fluid) sparing only the superior and nasal retina.
All investigations carried out including full blood count, urea and electrolytes, liver function test, thyroid function test, CPM, clotting profile, erythrocyte sedimentation rate were normal. HIV, Mantoux (tuberculin skin test), Treponema Pallidium Haemaglutinin Antibodies, Fluorescein Treponema Antibody, Rapid Plasma Reagin were all negative. Abdominal ultrasound, chest X-ray and Computerized tomography scan of the brain were also normal. The Positron emission tomography scan reported the lesion to be a low grade metabolically active disease with Melanoma and TB as possible differentials. A biopsy was suggested for a definitive diagnosis and patient was booked accordingly. Fundus fluorescein angiography (FFA) showed hyperfluorescence.
However, she was empirically started on anti TB medications as presumed left ocular TB but showed no significant change after approximately 4 weeks treatment but from the 8th week of treatment, there was evidence of gradual clinical improvement. By the 6th month the lesion had scarred with complete resorption of the subretinal fluid. She was advised to complete the 9 months regimen for extrapulmonary TB with follow up to monitor any possible re-activation post TB treatment. Three months after stopping treatment, she is still stable with the lesion much smaller [Figure 2].
Case Two
A 25-year old Indian male was referred for a right hyperpigmented lesion in the iris and a choroidal lesion in the right eye associated with complaints of blurred vision, and photopsia.
He had a history of poor vision in the left eye of 10 years duration, used spectacles in the past 3 years for myopia and had no family history of blindness.
He was retroviral negative and had no tuberculosis (TB) contacts.
Clinical examination revealed a visual acuity of 0.9 in the right eye which improved with pinhole to 1.2 and 0.2 in the left eye improved with pinhole to 0.8. The iris lesion was a naevus and the other significant findings were vitreous cells, inferior peripapillary atrophy, nil disc edema, and a large subretinal mass about 2 ½ disc diameter in size in the superonasal retina at the arcade. The intraocular pressure was 19mmHg in the right eye and 18 mmHg in the left eye. The left eye was essentially normal.
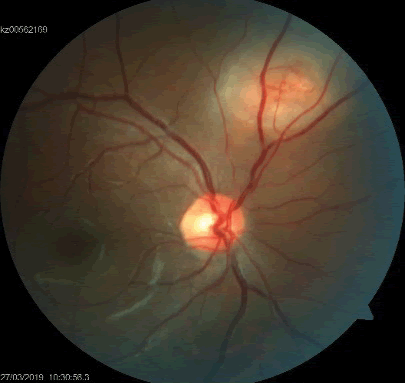
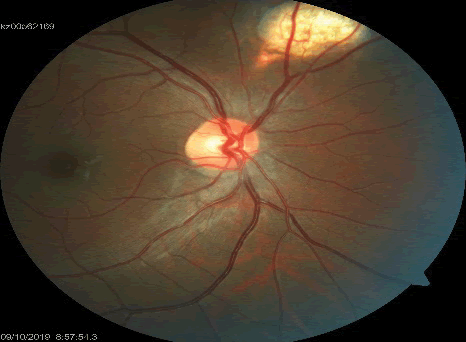
Fundus photograph showed a creamy orange coloured hyperaemic mass with vessels [Figure 3] which was hyperfluorescent on fluorescein angiography [Figure 4].
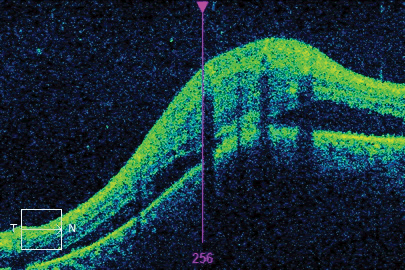
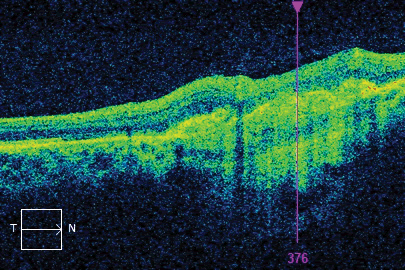
Optical coherence tomography (OCT) showed a large choroidal lesion with subretinal and intraretinal fluid [Figure 5]. There was also diffuse intraretinal fluid in the macula. An impression of right choroidal infective lesion presumably TB choroidal granuloma was made.
Full blood count, electrolytes, urea, creatinine, c-reactive protein, Real time Polymerase chain reaction for Mycobacterium tuberculosis, and chest X-ray were done but all results were negative. Mantoux test was not done in this patient.
The initial plan was to commence anti TB treatment if the results were positive for TB. Two weeks later, he was yet to start any treatment and the clinical picture was unchanged. The assessment of presumed TB granuloma was maintained based on a high index of suspicion. TB treatment was therefore initiated.
At a one-month review following the commencement of TB treatment, the lesion was less hyperaemic with distinct margins. The visual acuity in the right eye had improved to 1.2. He was asked to continue his TB treatment for 9 months and was reviewed in the Eye clinic monthly. The lesion progressively resolved and showed signs of pigmentation and scarring. Three months after onset of treatment, the visual acuity remained 1.2 and repeat colour photos at 6 months [Figure 6] showed the lesion had scarred down while OCT showed the subretinal and intraretinal fluid had absorbed completely [Figure 7]. He was advised to complete the 9 months TB treatment.
Discussion
Tuberculosis is a chronic granulomatous infection caused by Mycobacterium tuberculosis. It is largely a pulmonary disease but can also occur in other parts of the body including the eyes. Ocular TB can occur as a primary lesion in the conjunctiva, cornea or sclera or secondarily from a haematogenous spread to the retina, optic nerve and uvea including choroiditis and choroidal granuloma.[1] The index case presented as a choroidal granuloma. However, primary disease is rare, and the commonest form of ocular TB is inflammation of the uvea.[2]
Choroidal granuloma presents as a focal dome shaped elevated lesion. It can be unilateral, bilateral, solitary or multiple. Extensive lesions are usually associated with AIDS. The above cases presented as solitary focal creamy/orange lesions with no pulmonary TB, no TB contacts and RVD negative. These are rare findings as the presence of choroidal granuloma usually suggests a systemic spread and where it is a solitary presentation, other differentials such as sarcoidosis, leprosy, toxoplasmosis, toxocariasis should be considered in addition to ocular TB.[3] Similar cases of TB choroidal granuloma have been reported in literature but with associated miliary TB, and history of TB contact prior to presentation but no pulmonary or systemic TB signs.[4,5] A similar case with no other symptoms was confirmed following enucleation of the affected blind eye but the patient developed pulmonary TB fifteen days after the surgery.[6] The absence of pulmonary TB does not exclude the possibility of ocular TB. In fact, it has been reported that up to 60% of patients with extrapulmonary TB do not have any evidence of pulmonary TB.[1] A high index of suspicion in the absence of systemic signs is required in countries with a high burden of tuberculosis. South Africa is one of the 30 high TB burden countries.[7] The 2018 incidence of TB in South Africa was 301,000 with a rate of 520 per 100,000 population.[7]
OCT can also be used to confirm a diagnosis of choroidal tuberculoma if there’s a positive contact sign(localized inflammatory adhesion between the choriocapillaris-RPE layer and overlying neurosensory retina)[8] [Figure 5]. Hyperfluoresecence in the late stage of FFA have been reported in other studies with choroidal TB granuloma however,[3] there isn’t a characteristic FFA presentation for choroidal TB granuloma.[9]
In these cases, all the investigations carried out were negative as outlined above including RT-PCR which has been suggested as a confirmatory tool. IGRA a recent sensitive technique for TB diagnosis unaffected by BCG vaccination was however not done in the index cases. Based on a high level of suspicion, antituberculosis treatment was initiated. The response to treatment was marked with the lesions becoming fibrotic within 3 months of treatment.
A definitive diagnosis requires a histologic confirmation; however, this is only feasible with enucleation and so a diagnosis of choroidal tuberculoma is usually presumptive based on clinical and laboratory results and a high level of suspicion.[10]
Conclusion
Tuberculous choroidal granuloma can occur in healthy individuals with no positive TB contacts and no positive laboratory findings.
A high index of suspicion is needed for early diagnosis and treatment especially in TB endemic areas and resource constrained environments. In addition, tuberculous choroidal granuloma is responsive to anti-tuberculous treatment.
Competing Interests
The authors indicate no potential conflicts of interest.
REFERENCES
- Shakarchi FI. Ocular tuberculosis: current perspectives. Clinical Ophthalmology 2015;9:2223-2227.
- Varma D, Anand S, Reddy AR, Das A, Watson JP, Currie DC, et al. Tuberculosis: an under-diagnosed aetiological agent in uveitis with an effective treatment. Eye (Lond). 2006;20:1068-1073.
- Jabbour NM, Fans B, Trempe CL. A case of tuberculosis presenting with choroidal tuberculoma. Ophthalmology. 1985;92:834-837.
- Wang JC, Chuah GC, Yap EY Tuberculous choroidal granulomas in a patient with systemic lupus erythematosus. Int Ophthalmol. 2002;24:107-109,
- Rebello AC, Leonardo de Sousa JH, Gilberto de Sá J, Kalif de Sousa Rebello K. Macular granuloma due to tuberculosis without pulmonary symptoms. Rev Bras Oftalmol. 2015;74:251-253.
- Karim A, Laghmari M, Boutimzine N, Lamarti A, Ibrahimy W, Essakali N, et al. Choroidal granuloma revealing tuberculosis. A case report. J Fr Ophtalmol. 2003;26:614-617.
- WHO: Global Tuberculosis Report 2019.
- Sudarshan S, Ganesh SK, Biswas J. Current approach in the diagnosis and management of posterior uveitis. Ind J Ophthalmol 2010;58:29-34.
- Annamalai R, Biswas J. Bilateral choroidal tuberculoma in military tuberculosis - report of a case. J Ophthalmic Inflamm Infect. 2015;5:4
- Yeh S, Sen HN, Colyer M, Zapor M, Wroblewski K. Update on ocular tuberculosis. Curr Opin Ophthalmol. 2012;23:551-556.






 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.